To check the speed of blood clotting, doctors prescribe a coagulogram to patients, which can be signed up for on the website of the GoldenMed clinic. One of the main factors determining the speed of the blood clotting process is fibrinogen or the first clotting factor. But the purpose of a protein compound is not limited to one function. Knowing what protein is needed for, what causes it, and what causes its quantity to deviate from the norm, you can take better care of your health.
What is fibrinogen in a blood test?
Fibrinogen is a dissolved protein component circulating in the bloodstream that plays a key role in the formation of blood clots. The function of producing a substance that is renewed every 3-5 days lies with the liver cells.
The compound is involved in the initial stage of blood clot formation, being cleaved by thrombin to thread-like fibrin. Protein strands form a framework at the border of the injury, to which blood cells adhere, forming a blood clot. The resulting solid clot closes the wound and stops further bleeding. In addition to the hemostatic function, the protein compound is involved in:
- accelerating the regeneration of damaged areas of the skin, mucous membranes, soft tissues;
- fibrinolysis - the process of dissolving a blood clot as damaged areas are restored to normalize blood supply and prevent embolism;
- angiogenesis – the process of vascular growth;
- strengthening the walls of blood vessels to limit foci of inflammation and prevent further spread of pathogenic microorganisms.
Participation in many processes makes the amount of circulating protein within normal limits extremely important for the normal functioning of the body.
What does fibrinogen show in the blood?
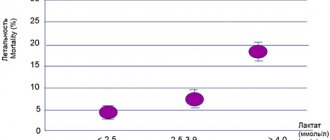
Accurate assessment of test results is of particular importance due to the tasks assigned to fibrinogen. Calculating the concentration of a protein compound helps in diagnosing many diseases, as it directly controls blood clotting processes, thereby maintaining hemostasis. A shift in normal protein levels in any direction leads to severe deterioration in health, even threatening life.
How to take a fibrinogen test?
To measure the level of protein compounds, you need to do a coagulogram or biochemical analysis of the blood composition. In both cases, a small amount of venous blood is used. To get the correct result, the procedure must be performed on an empty stomach, waiting at least 10-12 hours after the last meal.
Also, 2-3 days before the test, it is worth eliminating fatty, fried, smoked foods and alcohol from the diet, reducing physical activity, organizing a normal rest schedule and protecting yourself from emotional stress. The last cigarette can be smoked at least half an hour before the test.
With the permission of the doctor, you should also temporarily stop taking medications that affect plasma coagulation or liver protein synthesis.
Preparation before taking the test
For the study, venous blood is collected in the morning, on an empty stomach; it is advisable not to eat anything 12 hours before collecting biological material. You can also take the test throughout the day, provided you fast for 2-4 hours before the procedure. 2 hours before it, you should give up intense physical activity and smoking. Fibrinogen levels in the blood can be affected by certain drugs and medications, for example, heparin, anabolic steroids, androgens, antioxidants and oral contraceptives.
Avoid taking a fibrinogen hormone test during treatment for infectious diseases and severe bleeding, as well as for 1 month after a blood transfusion.
Fibrinogen is normal
Regulation of the amount of fibrinogen in the blood is determined by many factors, including gender, age category, and general condition of the body. The physiological norm is considered to be the average value obtained through mass studies on healthy patients from each category.
Fibrinogen in the blood is normal in women
The normal level of protein in the female bloodstream is considered to be 2-4 g/l. But you should remember about changes in blood composition under the influence of hormonal factors during menstruation. Increased viscosity and blood clotting during this period prevents the development of severe bleeding, but makes the research results incorrect. Women should not perform a venous puncture to assess protein levels earlier than 3-5 days after the end of menstruation.
Fibrinogen during pregnancy is normal
Pregnancy affects all functions of the female body, without bypassing the production of the first coagulation factor. During gestation, its concentration in the bloodstream can increase to 6.5 g/l. The increasing concentration of protein contributes to the successful course of pregnancy and childbirth. In this case, the amount of protein in the bloodstream should rise gradually, without going beyond the norm for each period of gestation.
The normal level of fibrinogen in the blood of men
In normal health, the level of coagulation factor in the blood of men, like that of women, ranges from 2 to 4 g/l. This indicator indicates the absence of a predisposition to bleeding or thrombosis, as well as a low likelihood of developing many dangerous disorders in the functioning of the cardiovascular system.
The normal level of fibrinogen in the blood of children
For children under 18 years of age, regardless of gender, the normal level of protein in the bloodstream is 1.25-4 g/l. The exception is newborn children, whose normal level of circulating fibrinogen is 1.3-3 g/l. The situation levels out as soon as the formation of a mature hemostatic system is completed, and the liver becomes capable of producing a sufficient amount of protein.
Complexes with this research
Preventive check-up Universal annual preventive screening RUR 11,960 Composition
Pregnancy planning. Clinical indicators 6,630 R Composition
Coagulogram Study of the functional state of hemostasis 2,020 R Composition
IN OTHER COMPLEXES
- Entry into IVF RUB 23,020
- Examination during pregnancy. 1st trimester 16,690 RUR
- Miscarriage RUB 40,070
- Extended coagulogram RUB 4,150
- Female infertility RUB 16,210
What does increased fibrinogen mean?
An increase in fibrinogen content in the bloodstream often warns of serious illnesses. It may be caused by:
- infectious and inflammatory pathologies (tuberculosis, pancreatitis, pneumonia, mononucleosis, etc.);
- growth of tumors;
- processes accompanied by massive cell death (blood poisoning, gangrene, cerebral stroke, myocardial infarction, burns);
- amyloid dystrophy;
- diabetes mellitus;
- suppression of the secretory function of the thyroid gland;
- autoimmune inflammatory diseases (scleroderma, Libman-Sachs disease, rheumatoid arthritis);
- vascular diseases (atherosclerosis, thrombophlebitis, varicose veins);
- excessive weight;
- hepatitis;
- recent surgery.
Taking certain groups of medications can also affect the level of this protein.
Coagulogram
Factors of the coagulation, anticoagulant (anticoagulant) and fibrinolytic blood systems take part in the hemostasis system. A change in the functional state of one of the systems is accompanied by compensatory changes in the activity of the other. Violation of functional relationships can lead to severe pathological conditions of the body, consisting of either increased bleeding or intravascular thrombus formation. The study of the hemostatic system has the following goals:
- diagnosis of disorders in the hemostasis system;
- clarification of the admissibility of surgical intervention in case of identified disorders in the hemostasis system;
- monitoring treatment with direct and indirect anticoagulants, as well as thrombolytic therapy.
Currently, the usual practice for recognizing hemostasis disorders is heterogeneous and often varies in different clinics from performing one or two uninformative tests (prothrombin index, fibrinogen) to using an overloaded list of methods, some of which duplicate each other.
Many routine tests are outdated, of little value and inaccurate. To date, assessment of the results of prothrombin time using the prothrombin index is incomparable with global methodological approaches. Conditions for taking a coagulogram
Eating food, including juice, tea, coffee, and alcohol, is not allowed for 8 hours (preferably 12) before the test. You can drink plain water. If your doctor has prescribed a test while you are taking medications that affect blood clotting, please note this when taking the test.
List of coagulogram tests:
- Lupus anticoagulant;
- D-dimer;
- Antithrombin II;
- Thrombin time;
- APTT;
- INR (PTV, PTI);
- Fibrinogen;
- Screening for antiphospholipid syndrome.
Lupus Anticoagulant
Lupus Anticoagulant is an inhibitor of the blood anticoagulant system. Being present in the blood, it increases the coagulation activity of the hemostasis system, which adversely affects the process of implantation of the embryo, the course of the entire pregnancy, and the development of the fetus.
D-dimer (fibrin degradation product, D-dimer, Fibrin degradation fragment)
Determination of D-dimer level is a highly specific and sensitive marker of thrombus formation. However, its level also increases in pathological conditions accompanied by increased fibrinolysis: hemorrhagic complications, infections, wound healing, in the presence of rheumatoid factor in the blood, etc. However, the determination of D-dimer has important diagnostic value in the diagnosis of thrombosis. Its normal level allows, with 98% accuracy, to exclude conditions accompanied by increased thrombus formation.
Antithrombin III
AT III is determined by thrombin inhibition. AT III deficiency can be hereditary or acquired. The most common clinical manifestation of hereditary AT III deficiency is the development of deep vein thrombosis and, as a consequence, pulmonary embolism. The likelihood of developing thrombotic complications in patients with AT III deficiency increases with age.
Acquired AT III deficiency may be due to decreased synthesis, increased protein intake, or loss of protein. In all these cases, there is a parallel decrease in the concentration and activity of AT III. AT III is synthesized in the liver, so some liver diseases lead to decreased AT III levels. If, in parallel with the decrease in AT III, there is an increase in the thrombogenic properties of the vascular wall and activation of coagulation, then a further decrease in AT III is observed due to its consumption, which occurs in DIC caused by various pathologies: massive injuries, sepsis, inflammation of wounds, snake bites, complicated pregnancy, cancer, etc.
In addition, a decrease in AT III synthesis is observed during therapy with estrogens and synthetic drugs with estrogenic effects, nephrotic syndrome and gastrointestinal diseases, when the loss of protein exceeds the rate of its synthesis. In these cases, a parallel decrease in AT III and albumin is observed.
Thrombin time (TV)
Gives a general assessment of the final stage of blood coagulation. This is an indicator of the transition of fibrinogen to fibrin, the state of the anticoagulant system. Does not depend on the internal and external activation system, but depends on the concentration of fibrinogen, the presence of abnormal fibrinogen, the activity of antithrombins, the processes of polymerization and stabilization of fibrin.
In the clinic, TV determination is used to monitor heparin therapy (especially high molecular weight heparin) and fibrinolytic therapy; for the diagnosis of activation of fibrinolysis, indirect diagnosis of hypo- and dysfibrinogenemia.
Clinical and diagnostic value
TV shortening:
- hyperfibrinogenemia (more than 6 g/l);
TV extension:
- severe hypofibrinogenemia (less than 1.0 g/l), dysfibrinogenemia;
- heparin therapy with regular heparin (the test detects relatively low concentrations of the anticoagulant - from 0.05 IU/ml of blood);
- the presence of fibrin polymerization inhibitors (PDF, paraproteins, etc.);
- increase in immunoglobulins;
- use of asparaginase, streptokinase, urokinase;
- a decrease in fibrinase activity (factor XIII) does not affect thrombin time.
Activated partial thromboplastin time (APTT)
APTT evaluates the intrinsic pathway of activation of the coagulation process. The test is also called kaolin-kephalin time. It is a simple and comprehensive test, sensitive to deficiencies of all coagulation factors. But it is mainly used to evaluate factors VIII, IX, XI, XII and prekallikrein. Sensitive to excess plasma anticoagulants. Does not depend on platelet count.
This test is one of the main tests for monitoring heparin treatment. In patients receiving heparin therapy, the aPTT lengthens by 1.5–2 times, which indicates the effectiveness of treatment.
Determining the APTT allows you to finally resolve the issue of tolerance to heparin: for this purpose, the APTT is determined 1 hour before the next administration of heparin. If the APTT is prolonged by more than 2.5 times compared to the norm, an increased sensitivity to heparin is noted, its dose is reduced or the interval between injections is increased.
Clinical and diagnostic value
of test extension:
- hypocoagulation and bleeding tendency;
- hemophilia (A, B, C);
- significant deficiency of factors II, V, X, XII, fibrinogen;
- von Willebrand disease;
- heparin therapy with unfractionated heparin (the test detects low concentrations of the anticoagulant - from 0.05 IU/ml of blood);
- treatment with indirect anticoagulants;
- the presence of blood clotting inhibitors (PDF, lupus anticoagulant).
A shortened test indicates hypercoagulability and a tendency to thrombus formation;
and is also observed during normal pregnancy and taking oral contraceptives. Prothrombin (thromboplastin) time (PT)
By means of PT with calculation of the international normalized ratio (INR) and prothrombin index (PI), the external mechanism is assessed in total. Prothrombin time depends on the content of prothrombin itself - factor II, as well as factors V, VII, X and fibrinogen. Used to diagnose thromboembolic and hemorrhagic conditions, to monitor treatment with indirect anticoagulants.
Clinical and diagnostic value
Prolongation of prothrombin time (PI decreases, INR increases) - a tendency to hypocoagulation. Main reasons:
- violation of protein-synthetic function of the liver;
- vitamin K deficiency (usually due to impaired breakdown and absorption of fats in the intestines);
- treatment with indirect anticoagulants;
- deficiency of factors II, V, VII, X;
- heparin therapy with regular heparin (the test responds to relatively high concentrations of the anticoagulant - from 0.5 IU/ml of blood);
- hypo-, dysfibrinogenemia, impaired fibrin polymerization;
- the presence of clotting factor inhibitors (PDF, lupus anticoagulant);
- medications: anabolic steroids, antibiotics, acetylsalicylic acid in large doses, laxatives, methotrexate, nicotinic acid, thiazide diuretics, etc.
Shortening of prothrombin time is rare and has no independent diagnostic value. Together with a shortening of APTT, it indicates a tendency towards hypercoagulation:
- thrombosis;
- increased activity of factor VII (trauma, necrosis);
- pregnancy, childbirth;
- medications: acetylsalicylic acid in small doses, oral contraceptives, corticosteroids, vitamin K, barbiturates, antihistamines, caffeine.
Currently, recording the results of prothrombin time using the prothrombin index does not meet modern requirements.
To unambiguously interpret the results of prothrombin time measurements, regardless of the laboratory, INR is used: this method allows you to mathematically correct the difference given by thromboplastins with different sensitivities. Calculated using thromboplastin standardized to the international sensitivity index. Determination of fibrinogen content
Its concentration is determined by the time of clot formation in diluted platelet-free plasma with the addition of excess highly active thrombin (according to Clauss). Fibrinogen is synthesized in the liver, from where it enters the blood. Changes in fibrinogen concentration are observed in various diseases - primarily in disorders of the hemostasis system and acute inflammation.
An increase in the amount of fibrinogen, even within normal values, is considered a risk factor for cardiovascular diseases.
Clinical and diagnostic value
Increased concentration (tendency to hypercoagulation):
- physiological (pregnancy, menstruation);
- mild forms of hepatitis;
- kidney disease;
- acute phase reactions, myocardial infarction;
- collagenoses;
- radiation sickness;
- malignant tumors (especially lung cancer);
- estrogens, oral contraceptives.
Decreased concentration (a decrease below 0.5–1 g/l causes bleeding):
- congenital afibrinogenemia, hypo- and dysfibrinogenemia;
- severe liver damage;
- condition after bleeding, injury, burn;
- bone marrow lesions (leukemia, tumor metastases);
- activation of fibrinolysis (including drugs);
- phenobarbital, anabolic steroids, unfractionated heparin in high doses.
In DIC syndrome, changes in coagulogram tests depend on the form and stage of the process.
Antiphospholipid syndrome (APL)
This is a group of diseases caused by the presence of antibodies to phospholipids. Antiphospholipid antibodies (APL) are autoantibodies of the IgG and IgM class, capable of binding to the antigenic determinants of phospholipids (cardiolipin, phosphatidylserine, phosphatidylinositol, phosphatidylic acid, phosphatidylcholine) and phospholipid binding proteins. Binding with cardiolipin occurs with the obligatory participation of a cofactor, rg-glycoprotein I.
The reasons for the production of APL have not been established. Presumably, long-term persistence of viruses that are tropic to the vascular endothelium causes: morphological and functional changes in endothelial membrane cells with the development of hypercoagulation syndrome, stimulation of B-lymphocytes, which under certain conditions produce aPL.
APL bind to phospholipids of cell membranes, changing the conformational and metabolic structure of the cell, which leads to disruption of cell function with the development of stasis and thrombosis. Due to the fact that vessels of different sizes and different locations are affected, the range of clinical manifestations of APS is diverse - thrombosis, strokes, obstetric pathology, thrombocytopenia. The incidence of aPL in various pathological conditions is presented below.
Pathological condition/APL detection frequency, %:
- Recurrent venous thrombosis: 28–71
- Recurrent miscarriage: 25–64
- Transverse myelitis: 50
- Thrombocytopenia: 27–33
- Hemolytic anemia: 38
- Arterial thrombosis: 25–31
- Pulmonary hypertension: 20–40
The most significant manifestation of APS is obstetric pathology associated with placental decidual vasculopathy - recurrent miscarriage, antenatal fetal death (usually in the 1st and 2nd trimester), severe forms of gestosis, intrauterine growth retardation.
In the population, aPL is found in 2–4% of the population. The incidence of aPL increases in patients with autoimmune, inflammatory, infectious diseases, malignant tumors, while taking oral contraceptives, psychotropic drugs. APS can be primary (there are no signs of other autoimmune diseases) or secondary (against the background of other autoimmune diseases, most often systemic lupus erythematosus). There is also a seronegative variant of APS, characterized by the absence of aPL and lupus anticoagulant in the presence of clinical manifestations of APS. In this form, only antibodies to glycoprotein I are detected.
The main criterion for the laboratory diagnosis of APS is the presence of aPL (or antibodies to cardiolipin) and lupus anticoagulant in 2 or more studies at least 6 weeks apart.
Indications for prescribing analysis for aPL:
- Obstetric pathology (recurrent miscarriage).
- Recurrent thrombosis of various locations.
- Systemic connective tissue diseases (systemic lupus erythematosus, Sjogren's syndrome).
- Thrombocytopenia.
- False-positive reaction to syphilis using cardiolipin antigen (RW, RPR).
Indications of basic coagulation tests
Test Deficiency and/or inhibition of factors/Effects of anticoagulants
XII, XI, IX, VIII, von Willebrandt, Fletcher, Fitzgerald factors V, X VII II (prothrombin) I (fibrinogen) direct/indirect.
- Thrombin time
- normal/normal/normal/extended/extended/extended/normal. - APTT
- prolonged/prolonged/normal/normal/prolonged/normal/prolonged/prolonged/prolonged. - Prothrombin time (INR)
- normal/extended/extended/extended/normal/extended/extended/extended. - Fibrinogen
- normal/normal/normal/reduced or undetectable/reduced or undetectable/normal/reduced/normal.
Note.
Prothrombin time (INR) results are inversely proportional to prothrombin index results. Outdated methods for studying hemostasis disorders and options for their replacement
Method/Disadvantages/Modern methods.
- Clotting time/Low standardization/APTT.
- Recalcification time/Low standardization/APTT.
- Plasma tolerance to heparin/Low standardization/Plasma thrombin-heparin time, determination of anti-Xa activity.
- Autocoagulation test (ACT)/Low standardization/APTT, antithrombin III activity.
- Beta-naphthol (fibrinogen B), ethanol or protamine sulfate tests / Low-informative, low-quality expression of results, often false positive / Tests for thrombinemia: quantitative determination of SFMC (soluble fibrin-monomer complexes).
Optimal complex of hemostasiological laboratory tests
Test/Hemostasis link/Diagnostic significance.
- Platelet count/Vascular platelet/Main component of platelet hemostasis.
- Von Willebrand factor (VWF)/Vascular platelet/Plasma platelet adhesion cofactor and marker of vascular wall endothelial damage.
- Prothrombin time (PT)/Procoagulant (extrinsic coagulation mechanism)/Screening test to determine the factors (fibrinogen, prothrombin, factors v, VII and X) involved in blood clotting initiated by high concentrations of tissue factor.
- APTT (aPTT)/Procoagulant (intrinsic coagulation mechanism)/Screening test to determine factors (fibrinogen, prothrombin, factors V, VIII, IX, X, XI, XII, prekallikrein and high molecular weight kininogen) involved in blood coagulation upon contact activation. A phospholipid-dependent screening test that provides insight into disorders associated with the effect of the lupus anticoagulant - VA.
- Thrombin time (TT)/Procoagulant (fibrin formation)/Screening test of the last stage of blood coagulation - reaction between thrombin and fibrinogen - anticoagulant activity of antithrombin III.
- Fibrinogen/Procoagulant (substrate)/The main substrate from which fibrin is formed under the action of thrombin.
- D-dimer/Procoagulant and fibrinolytic (activation of coagulation in vivo)/Fibrin degradation product, one of the most specific tests for the diagnosis of DIC syndrome, thrombophilia and thrombosis, a marker of thrombin formation, fibrin formation and activation of secondary fibrinolysis.
- Antithrombin III/Anticoagulant/Basic physiological anticoagulant, for which heparin is a cofactor, inactivates thrombin and active factors IX, X, XI, XII.
- Protein C / Anticoagulant / Physiological anticoagulant, in the activated state, inactivates active factors V, VII, inhibits plasminogen activator (activity manifests itself mainly in the microcirculatory bed).
- Lupus Anticoagulant (LA) Confirmatory Test/Done as part of an extended screening test to confirm the presence of LA.
It is possible that this range of studies is insufficient for patients with severe pathology of the hemostatic system, but in the case of preliminary screening and monitoring of therapy, it seems necessary and sufficient.
What to do if there is elevated fibrinogen?
If the analysis shows that the coagulation factor in the blood exceeds the permissible norm, you should consult a doctor for a more detailed examination and identify the cause of the increase. The specialist’s task in this case is to prescribe effective therapy to eliminate the underlying disease. Eliminating the root cause of the increase in the amount of protein leads to its gradual independent reduction to acceptable limits.
If necessary, fibrinogen levels can be normalized:
- antiplatelet agents;
- anticoagulants;
- thrombolytics;
- fibrinolytics.
A revision of the diet with the inclusion of fresh vegetables, seafood and fish, red berries, dark chocolate or cocoa has a beneficial effect on the amount of protein compounds in the blood. If you follow your doctor's instructions, elevated fibrinogen does not pose a serious health hazard.
Low protein
As the amount of fibrinogen decreases, the rate of blood clotting decreases and the risk of spontaneous bleeding increases. The root cause of the anomaly lies in congenital characteristics or individual diseases:
- due to DIC syndrome;
- congenital afibrinogenemia, hypofibrinogenemia;
- deficiency of ascorbic acid and cobalamin;
- treatment with anticoagulants;
- polycythemia, taking androgens or anabolic steroids, fish oil;
- toxicosis of pregnant women - early and late type;
- poisonous snake bites;
- liver cirrhosis;
- amniotic fluid embolism - a problem that occurs in infants.
A decrease in protein units occurs in vegetarians, during therapy with antioxidants, and moderate consumption of alcoholic beverages (with clearly adjusted dosages). When the level drops from 0.5 to 1 g/l, there is a risk of bleeding from the arteries and veins of the internal organs. The condition requires hospitalization and observation by medical personnel.
Fibrinogen is below normal - what does this mean?
A drop in fibrinogen levels below the physiological norm poses a serious health hazard. Its deficiency leads to the inability to quickly stop bleeding, which means a large loss of blood even with a minor wound.
A decrease in the concentration of the first coagulation factor on the study may occur as a result of:
- massive blood loss;
- liver failure, hepatosis, cirrhosis;
- hypovitaminosis C and B12;
- intoxication with poisons;
- DIC syndrome;
- toxicosis during pregnancy;
- malignant blood diseases;
- congenital fibrinogen deficiency;
- polycythemia;
- heart failure;
- alcoholism;
- vegetarian diet.
Most causes of low fibrinogen levels pose serious health risks.
What to do if fibrinogen is low?
As in the reverse situation, the primary task for the doctor is to promptly detect the cause of reduced fibrinogen and prescribe the necessary treatment. At the same time, therapy can be carried out aimed at raising the amount of fibrinogen to an acceptable norm, including taking:
- aminocaproic acid;
- Tranescam;
- Dicinona;
- Vikasola.
You should also adjust your diet, focusing on protein-rich foods, including eggs, dietary meat, and legumes.
Medical doctors will help you quickly find out your fibrinogen level and eliminate the causes of its violation. To make an appointment, call the phone numbers: +7 or. Take a step towards good health!
Additional facts about fibrinogen
- The fibrinogen index, as a rule, is deciphered in conjunction with other tests, for example, PT and APTT.
- In the absence of a superficial reason for a decrease in the fibrinogen index and in the presence of some general clinical or medical history data, an immunological analysis of colorless protein is used to determine the basis of the disorders.
- To avoid incorrect results, blood testing for fibrinogen levels should not be performed on old specimens collected within 4 hours after administration of therapeutic doses of unfractionated heparin.
- High concentrations of unfractionated heparin may result in incorrect measurements of true fibrinogen levels.