What does the lymphatic system of the neck consist of?
The lymphatic system of the neck includes vessels and nodes.
Vessels:
Lymphatic capillaries are thin-walled structures consisting of a single layer of endothelial cells. They are found in all tissues of the body and, combining with each other, promote the outflow of lymphatic fluid into larger lymphatic vessels.
The wall of lymphatic vessels consists of three layers: an inner layer of endothelial cells, a middle muscle layer and an outer layer of connective tissue. Lymphatic vessels have many more valves than venous vessels, and the circulation of lymph is entirely dependent on the compression of the vessels by the surrounding muscles. Lymphatic vessels drain lymph to the lymph nodes.
Nodes:
On average, there are up to 75 lymph nodes on each side of the neck. The outside of the node is covered by a capsule, under which there are subcapsular sinuses - the place where lymphatic fluid enters from the afferent lymphatic vessels. The fluid passes through the lymph node tissue, which consists of the cortex and medulla, and then exits through the hilum of the lymph node and enters the draining lymphatic vessels. As a result, lymph enters the venous system at the junction of the internal jugular and subclavian veins.
Anatomical structure of the lymph node (Alila Medical Media/ Shutterstock ©)
Contraindications for MRI with contrast:
- history of polyvalent drug allergies;
- any previous adverse reactions to MRI contrast agent;
- acute and chronic renal failure (decrease in glomerular filtration from 30 ml/min/1.73 m and below);
- severe liver failure;
- severe form of bronchial asthma;
- undergoing a previous study with contrast (MRI, CT, radiography, etc.) earlier than 36 hours.
Preparation for MRI of soft tissues of the neck
No preparation is required for MRI of the soft tissues of the neck. True, in some sources you can find recommendations according to which you need to come for a contrast study on an empty stomach, but our experts consider this unnecessary.
Classification of lymph nodes of the neck
Currently, the classification of the American Joint Committee on Cancer (AJCC) 8th edition of 2018 is recommended for use worldwide:
- Level I (IA and IB): submental and submandibular lymph nodes;
- Level II (IIA and IIB): superior jugular group (divided into 2 sublevels, the border between which is the accessory nerve);
- Level III: middle jugular group;
- Level IV: lower jugular group;
- Level V (VA and VB): lymph nodes of the posterior triangle of the neck;
- Level VI: anterior cervical lymph nodes;
- Level VII: upper mediastinal lymph nodes.
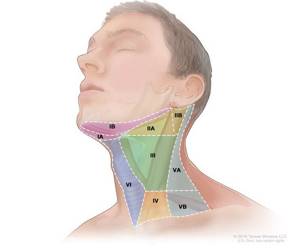
Levels of lymph nodes of the neck (Tenese Winslow LLC ©)
Diagnostics
Inspection
When palpating the neck, the doctor pays attention to the location, size, density and mobility of each node. Particular attention is paid to nodes that appear to be fixed to underlying neurovascular structures and internal organs. The description of each node becomes an important part of the medical documentation, which can later be used to evaluate the effect of treatment.
Radiation methods
- Ultrasonography
The advantages of ultrasound over other imaging methods are price, speed of examination and low radiation exposure to the patient.
Ultrasound signs of metastatic lesions of the lymph nodes can be the formation of a spherical shape, a violation of the structure, unclear boundaries, the presence of central necrosis, etc.
Since it is not always possible to say with certainty from ultrasound whether a lymph node is affected or not, sometimes a fine-needle aspiration biopsy under ultrasound guidance is simultaneously performed, followed by a cytological examination of the material from this node. The result of a cytological examination depends on the skill of the sonographer and the quality of the sample (ie, the presence of a sufficient number of representative cells).
- CT scan
With the advent of high-resolution systems and special contrast agents, CT makes it possible to detect lymph nodes that may have been missed by other diagnostic methods.
- Magnetic resonance imaging
The value of MRI is its excellent detail of soft tissue. MRI is superior to CT as the study of choice in the evaluation of a number of head and neck neoplasms, such as the base of the tongue and salivary glands. Size, the presence of several enlarged nodes and central necrosis are criteria common to CT and MRI examination protocols.
- Positron emission tomography
This new imaging technique is increasingly being used to stage head and neck tumors. The method is based on the uptake of 2-fluoro-2-deoxy-D-glucose (FDG) by metabolically active tissues. The test can also be combined with a CT scan to improve image resolution and more accurately determine the location of the lesion.
Biopsy
A biopsy is the removal of a small piece of tissue to be examined under a microscope or tested in a laboratory for signs of cancer. In the vast majority of cases, a fine needle aspiration biopsy is performed. The doctor performing the biopsy may use an ultrasound or CT scan to perform the procedure. Sometimes fine needle aspiration biopsy does not provide a definitive diagnosis and other types of biopsy such as core biopsy or excisional biopsy are required.
| |
| The process of preparing slides for cytological examination. The material is the contents of the syringe after performing a fine-needle aspiration biopsy. | |
How is a CT scan of the mediastinum performed?
Computed tomography uses sophisticated equipment. The CT machine consists of a movable table and a ring part, inside of which there are emitters and sensors.

Computed tomography of the lungs and mediastinal organs
The patient lies face up on the conveyor. To improve image quality, you must remain still throughout the entire session. Changing the position of the body leads to distortion of the picture and the appearance of artifacts in the images.
The table with the patient moves inside the tomograph ring. The scanning elements move in a circle, taking several pictures per full revolution. The procedure is called multislice computed tomography. MSCT provides:
- reduction of radiation exposure;
- reduction of scanning time;
- improving image quality.
As a result, photographs of axial sections are obtained, with the help of which sagittal and frontal projections are completed. To clarify the localization of the pathological focus and assess the relative position of the anatomical structures of the mediastinum, a 3D model of the area under consideration is reconstructed.
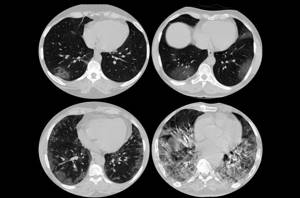
Viral (Covid) pneumonia on a tomogram
A CT scan of the mediastinum and lungs takes 5 to 10 minutes. When using contrast enhancement, the duration of the diagnostic procedure increases. The injection is done after a series of native photographs. The scan is paused and a “staining” solution is injected into the patient through an intravenous catheter. Within 10-15 minutes, the drug fills the lumen of the vessels of the chest cavity, after which scanning is continued.
A CT scan of the mediastinum with contrast takes no more than half an hour. After 1-2 days, the body is completely cleansed of traces of the iodine-containing solution.
Treatment plan
After determining the diagnosis and conducting all diagnostic studies, the doctor will recommend the optimal course of treatment for the patient. Ultimately, treatment for lymph node metastasis depends on the type and location of the primary tumor.
There are three different treatment options that can be used alone or in combination:
- surgical intervention,
- radiation therapy,
- chemotherapy.
Surgery
Surgical treatment usually involves removal of the lymph nodes in the neck (lymph node dissection) and subsequent histological examination to accurately determine the stage, as this can significantly influence further treatment. Although not always, most often lymph node dissection is performed simultaneously with removal of the primary tumor.
There are different types of lymph node dissections:
- radical lymph node dissection: removal of all lymph nodes, removal of the internal jugular vein, removal of muscles and nerves;
- modified radical lymph node dissection: removal of all lymph nodes while preserving muscle. The nerves and/or internal jugular vein may be removed;
- selective lymph node dissection: removal of only certain groups of lymph nodes.
Radiation therapy
Radiation therapy may be given as a stand-alone treatment in the postoperative period to reduce the likelihood of relapse, or in combination with chemotherapy as a stand-alone or adjuvant treatment. Adjuvant radiotherapy is usually necessary if histological examination reveals multiple involved lymph nodes.
Chemotherapy
Chemotherapy is usually added to radiation therapy as a stand-alone or adjuvant (post-surgery) treatment. In some cases, induction chemotherapy may be used to reduce the size of the lesion and subsequent surgery.
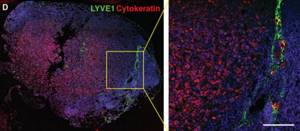
Immunofluorescence visualization of a metastatic lymph node stained for Cytokeratin (red), a marker characteristic of tumor cells of epithelial origin. Scale bar: 50 µm (Science Advances/Michael Detmar Group ©)
Forecast
Metastases to the lymph nodes of the neck can occur in cancer of various locations, so prognostic assessments for this group of patients should be made only after identifying the primary tumor.
Factors influencing the forecast:
- stage of the disease
- localization of the primary tumor,
- histological subtype and degree of differentiation,
- number and size of affected lymph nodes,
- characteristics of the tumor resection margin.
Why do an MRI of soft tissues and organs of the neck?
In the neck area there are many important structures that are in close proximity to each other, which is why disorders in different organs can manifest themselves with similar clinical symptoms. Therefore, it is very important to be able to conduct a single study that can simultaneously identify the status of each of them. MRI of the thyroid gland, larynx or cervical lymph nodes is always in demand and is performed for a variety of indications:
- fresh injuries (to accurately determine damaged structures);
- non-metallic foreign bodies of soft tissues and organs of the neck (larynx, esophagus);
- previous injuries and their consequences (compression of the neck arteries by scar cords, impaired flexion and extension of the head);
- inflammatory diseases (soft tissues - abscess or phlegmon, thyroid gland - thyroiditis, salivary glands - mumps);
- malignant and benign neoplasms;
- suspicion of metastases to the cervical lymph nodes, determining the stage of cancer by the degree of tumor invasion into surrounding organs;
- abnormalities of the neck organs (low location of the thyroid gland);
- vascular diseases (atherosclerosis of the carotid arteries, aneurysms, etc.);
- endocrine pathology (hyper- or hypothyroidism).
Observation after treatment
Patients should see their head and neck tumor specialist regularly to be assessed for any signs of disease recurrence.
Standard observation schedule
In the first 1–2 years, inspection and collection of complaints are recommended to be carried out every 3–6 months, for a period of 3–5 years – once every 6–12 months. After 5 years from the date of surgery, you must visit the doctor once a year or when complaints arise. In patients at high risk of relapse, the interval between examinations can be shortened.
Bibliography:
- RUSSCO Practical recommendations for the treatment of malignant tumors of the head and neck. 2021
- NCCN Clinical Practice Guidelines in Head and Neck Cancers Version 1.2021 — November 9, 2020
- DeVita, Hellman, and Rosenberg's Cancer: Principles & Practice of Oncology (Cancer Principles and Practice of Oncology) 11th Edition 2019
- AJCC (American Joint Committee on Cancer). Cancer Staging Manual – 8th Edition. New York, NY: Springer; 2018
- Pisani, Paolo et al. “Metastatic disease in head & neck oncology.” Acta otorhinolaryngologica Italica 2020
- Van den Brekel MW. Lymph node metastases: CT and MRI. Eur J Radiol. 2000
- Chen ZW, Zhu LJ, Hou QY, Wang QP, Jiang S, Feng H. Clinical application of positron-emission tomography for the identification of cervical nodal metastases of head and neck cancer compared with CT or MRI and clinical palpation. Chinese journal of dentistry. 2008
- Qiaoli Ma et al. Unexpected contribution of lymphatic vessels to promotion of distant metastatic tumor spread. Science Advances 08 Aug 2018
- Sun, J et al. Computed tomography versus magnetic resonance imaging for diagnosing cervical lymph node metastasis of head and neck cancer: a systematic review and meta-analysis. OncoTargets and therapy. 2015
- Robbins KT, Shaha AR, Medina JE, et al. Consensus statement on the classification and terminology of neck dissection. Arch Otolaryngol Head Neck Surg. 2008
- López, Fernando et al. Cervical lymph node metastases from remote primary tumor sites. Head & neck 2016