Liver diseases occur at any age. They can be congenital or acquired during life. It is very important to diagnose them at an early stage. Computed tomography of the liver is a very reliable and reliable method for diagnosing diseases of the organ.
Indications for CT scan of the liver are:
- Preoperative study.
- Suspicion of tumor formations, as well as their diagnosis.
- Identifying the consequences of injury.
- Diagnosis of complications after surgery: hematomas, abscesses and others.
- Suspicion of vascular damage to the organ.
- If it is not possible to perform an ultrasound if there is excess fat in the area to be examined.
What is liver ultrasound - a brief description
Ultrasound
Liver examination is a study of the organ using ultrasonic waves emitted and perceived by special devices called ultrasound scanners. The essence of the study is that an ultrasonic wave with an oscillation frequency of more than 20,000 Hz is capable of penetrating into tissues to a small depth, passing through them, and then part of the waves is absorbed by cells, and the other part is reflected with or without refraction. It is these reflected waves that come back to the ultrasound scanner sensor, are captured by it, converted into electrical impulses and create a picture on the monitor. The doctor sees on the monitor an image of the organ created by reflected and refracted ultrasonic waves passing through the thickness of the tissue.
To obtain an ultrasound image, the monitor uses a single sensor that simultaneously emits and detects ultrasound waves. To assess the condition of various organs, it is necessary to use sensors that emit waves of different frequencies, penetrating to different depths.
For the purpose of performing an ultrasound of the liver
they use sensors with different frequencies of emitted ultrasonic waves, as this is necessary for the best visualization of the organ and the detection of its pathology. Thus, currently for liver ultrasound they use 3.5 - 5 MHz sensors, which make it possible to see objects with a diameter of 1 - 3 mm. Sensors with a frequency of 3.5 MHz allow you to obtain images of tissues and organs located at a depth of 12 - 28 cm from the surface of the sensor. That is why such sensors (3.5 MHz) are used to examine adult patients of normal and obese physique. And sensors with a frequency of 5 MHz provide images of objects located at a depth of 4 - 15 cm from the sensor surface. Therefore, 5 MHz sensors are used to perform liver ultrasound in adolescents and thin patients.
The image obtained using reflected ultrasonic waves on the monitor allows you to evaluate the size, structure, location of the liver and its parts, identify the presence of various additional formations (cysts, tumors, etc.), inflammatory changes, etc. Based on the appearance, size, structure of the organ, the presence of inflammation or additional formations in the liver, as well as the condition of the surrounding tissues, lymphatic and blood vessels, the doctor can diagnose various pathologies, such as hepatitis, cirrhosis, hepatosis, cysts, hemangiomas, adenomas, cancer, liver metastases.
Ultrasound of the liver is a painless, safe, non-comfortable, but informative study that is easily tolerated by patients, since to carry it out the doctor does not have to insert any instruments into various parts of the body. Since ultrasound is a safe, non-discomforting and well-tolerated examination method, it can be performed without any restrictions on pregnant women, children and the elderly.
Ultrasound of the liver can also be performed for diagnosis
existing pathology of the organ, and as one of the methods of preventive examination. For diagnostic purposes, liver ultrasound is prescribed when a person has any symptoms indicating liver pathology, such as pain in the epigastric region (in the middle of the abdomen, between the ribs), on the right or left under the ribs, yellowness of the skin or sclera of the eyes, unexplained itching of the skin, elevated body temperature, and high levels of amylase and bilirubin in the blood. In addition, to diagnose liver damage, ultrasound is prescribed when there has been an abdominal injury. It is mandatory that liver ultrasound be performed at certain intervals for already identified liver diseases to assess the condition of the organ and monitor the course of the disease, as well as to determine the effectiveness of the therapy.
As one of the methods of preventive examination, ultrasound is usually performed once a year. For preventive purposes, ultrasound is especially recommended for people who have a high risk of developing liver diseases, for example, due to alcohol abuse, taking toxic medications, etc.
Some aspects of the diagnosis of focal nodular hyperplasia of the liver (fibronodular hyperplasia)
Ultrasound scanner HS50
Affordable efficiency.
A versatile ultrasound scanner with compact design and innovative capabilities.
Until relatively recently, focal nodular hyperplasia of the liver (FNH) was considered a rare (3%) space-occupying tumor of the liver. However, taking into account the use of modern imaging methods, FNH currently ranks 3rd among benign liver tumors after hemangioma and adenoma [8, 10, 14].
According to the morphological classification of liver tumors, FNH refers to tumor-like processes and is characterized by hyperplasia of the liver parenchyma, divided into nodes by fibrous layers in the form of a stellate scar [14]. Hyperplastic nodes without clear boundaries pass into the surrounding tissue without squeezing it. The tumor consists of hepatocytes, elements of the bile ducts, Kupffer cells and fibrous tissue.
The origin of hyperplastic nodes is not entirely clear. It is possible that their component is a benign tumor - an adenoma, which is characterized by the presence of a connective tissue capsule. Similar nodes of a regenerative-reparative nature can also be found in a dense, cirrhotic liver that has undergone submassive necrosis. According to some authors, the essence of the process lies in the fact that at the site of complete death of the parenchyma, desolation of the vascular system is noted with the disappearance of the network of argyrophilic fibers and the development of fibrous connective tissue. Along with this, new nodes with their characteristic features can form from the remaining parenchyma remains [8, 10, 14]. FNH is believed to be a response of hepatocytes to local vascular malformations (congenital or acquired). Local changes in blood flow lead to the appearance of areas of parenchyma with increased arterial blood supply and hyperplasia of liver cells.
FNH develops at any age, equally often in people of different sexes. At the same time, there is evidence that such neoplasms are more often diagnosed in women (in 82.2% of cases) [10, 17].
FNH occurs in 66.7% of patients under 40 years of age, in the liver without hepatitis and cirrhosis - in 83.3% [8, 9, 14, 17], in 57.7% of cases, FNH is located subcapsularly, in 33.7% - intrahepatically [9, 10, 17].
Macroscopically, focal nodular hyperplasia is a soft-elastic, clearly circumscribed, sometimes encapsulated grayish-brown node measuring from 0.5 to 6 cm. The nodes can be either single or multiple and located in the peripheral parts of the right (usually) and left lobe. Sometimes the nodes bulge noticeably on the surface of the liver, in rare cases they have a stalk. The nodes have a lobular structure with the presence of fibrous layers, usually extending from a centrally located scar.
Microscopic examination of the nodes reveals normal hepatocytes containing glycogen and forming trabecular structures. In some places, polymorphism in the size and shape of mature hepatocytes is observed; they form a syncytium. In the center of the hepatic lobe, as a rule, there is a central vein; there are sinusoids lined with Kupffer cells (stellate reticuloendotheliocytes). The portal layers are formed correctly and are quite delicate. Vessels are located in the area of the stellate scar and along the stroma. The vascular component is very diverse both in content (venous, thick-walled arterial vessels with myxomatous degeneration of the middle layer) and in form (hemangiomatosis). Along the portal septa, proliferating bile ducts, single small regeneration nodes and lymphoplasmacytic infiltrates are identified. These signs serve as the main differential diagnostic criteria to distinguish FNH from hepatocellular adenoma [17].
There are 2 types of FNH: classical and non-classical. In the classic type, all 3 signs are distinguished: abnormal nodular structure, tortuous thick-walled vessels, hyperplasia of the bile ducts. A central scar is present in 65% of cases. It always contains altered vessels of different sizes: large tortuous arteries with hypertrophy of the intima and media, large and small veins, capillaries. With the non-classical type, one of two signs is absent (nodular structure or altered vessels), but ductal hyperplasia is always present. There is no central scar. In turn, the non-classical type is divided into 3 subtypes: telangiectatic (prone to bleeding), adenomatous and FNH with cellular atypia.
The tumor in most cases (66.7-80.8% of patients) does not manifest itself clinically and can be accidentally discovered during an ultrasound examination for another reason [18]. There are no specific laboratory symptoms. FNH does not become malignant and the edge often causes complications in the form of intra-abdominal bleeding.
Ultrasound picture of FNH
Thus, with B-mode ultrasound, the appearance of FNH is nonspecific and variable. Most often, FNH of the liver looks like a single focal formation with fuzzy or clear, even or uneven contours, somewhat heterogeneous in its internal structure, without a capsule. In 80% of cases (Fig. 1), the lesion is isoechoic or hypoechoic [3, 8, 9, 11-14].
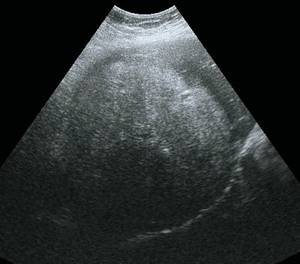
Rice. 1.
Ultrasound picture of FNH of the liver.

A)
B-mode. In the IV segment of the liver, reaching the contour of the liver, deforming it, a tissue density hypoechoic formation, somewhat heterogeneous in echostructure, measuring 50 x 40 mm, irregular in shape, with clear, even contours, is visualized.

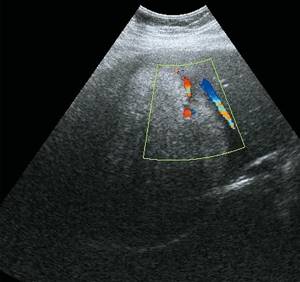
b)
In the Color Doppler mode, the blood flow is expressed in the form of a “basketball basket”; the “feeding” artery is determined.
The use of color Doppler mapping (CDC) mode reveals a high degree of blood supply to the formation (hypervascular, with active pulsating internal blood flow). A typical sign of FNH is the “feeder” artery. Multiple vessels are identified in the lesion, which have a typical “basketball basket” or “spoked wheel” pattern, characteristic of FNH, caused by arteries diverging from the center to the periphery. Dopplerography identifies arterial vessels in the center of the tumor (with high speed: systolic speed 0.71 m/s, average systolic speed 0.33 m/s (20.0 ± 11.3 cm/s), high diastolic speed, low index Doppler liver perfusion, low pulsation index 0.9 ± 0.35) and venous along the periphery [1, 2, 5 10, 14, 15]. The ratio of veins and arteries inside the formations is 33 and 44%, respectively.
FNH is characterized by the absence of arteriovenous shunting within the tumor; usually the blood supply is from a single artery.
In biphasic dynamic contrast echography, typical features are pronounced vascularization of the mass and rapid contrast enhancement in the early arterial phase. In the venous parenchymal phase of contrast enhancement, the structure of the formation becomes iso- or hyperechoic. The central scar remains hypoechoic during the arterial and portal phases. The persistence of enhancement in the portal and parenchymal phases is not typical for metastases and adenomas, which is an important point in differential diagnosis [3, 11, 16].
According to some authors, the sensitivity of ultrasound in the gray scale mode in diagnosing FNH is 93.5%, the sensitivity of ultrasound with contrast in diagnosing FNH reaches 96% [11].
CT scan of focal nodular hyperplasia
On native computed tomograms, FNH is represented by an inhomogeneous (sometimes homogeneous) formation of hypodense (reduced) density (according to some authors, hypodense in 69% of patients) or isodense with a zone of very low density in the center (the central scar is detected in 80% of patients, as a zone of very low density in the center) [9,10, 12, 14].
In a native study, FNH may be indistinguishable from liver hemangioma: FNH is hypodense, like a hemangioma, and the area of low density in the node may have a stellate appearance and be mistakenly interpreted as a “hyaline cleft” [9, 10, 17].
After contrasting, the formation actively accumulates contrast in the arterial phase (in 71-96% of patients) and becomes hyperdense when compared with the surrounding tissue.
Contrasting is uniform, with the exception of the central scar area; after contrast “enhancement,” the scar becomes more hyperdense. Unlike hemangioma, the hypercontrast lacunae of which, although they can have a high intensity comparable to the aorta, the FNH node literally “floods” the entire area with contrast, although not quite evenly, except for the central scar. In the venous phase, hypercontrast remains [9, 12, 14, 17, 18]. According to other authors, in the venous phase in 53.3% of cases the formation becomes homogeneous and in 73.3% - isodense [18].
In the late (delayed) phase of contrast, 4-5 minutes after the administration of contrast, the central scar of the FNH intensively accumulates the contrast agent and becomes especially clearly visible. The FNH node itself becomes hypodense in relation to the liver parenchyma (in contrast to the hemangioma, which is hyperdense on delayed scans) [9, 12, 14, 17, 18].
The sensitivity of CT with contrast in the diagnosis of nodular hyperplasia reaches 80-100% [17, 18].
MRI of focal nodular hyperplasia
On MRI on T1- and T2-weighted images, this tumor appears as a homogeneous (in 66.7-94% of patients), sometimes irregularly shaped, with unclear uneven contours, an isointense formation compared with unchanged parenchyma. In the center of this formation, a low-intensity linear structure—a connective tissue scar—is visualized. On T1-weighted images, the central scar is hypointense, but on T2-weighted images, the central scar gives a strong signal - this is because the scar consists of richly vascularized young connective tissue [7-10, 12, 14, 17, 18].
Contrast “enhancement” in MRI has the same mechanism of contrast accumulation as in CT. When contrasting, a homogeneous enhancement of the formation is noted in the early phase (25 s), except for the connective tissue scar, and only later, after 45 s, does the central scar give a strong signal on T1-weighted images. During a delayed study with contrast, the signal intensity from the formation decreases with increasing contrast of the connective tissue scar. A central scar is pathognomonic for FNH. The accuracy of MRI with contrast in diagnosing hyperplasia is 80-100% [7-10, 12, 14, 17, 18].
Angiography of nodular hyperplasia
The formation is hypervascular, homogeneous, contrasting, expressed in the arterial phase [1, 2, 14]. The sensitivity of angiography in diagnosing nodular hyperplasia is in the range of 82-97.3% [1, 2, 14].
Differential diagnosis is carried out with liver adenoma (Fig. 2), as well as with liver metastases (Fig. 3).
Rice. 2.
Ultrasound picture of liver adenoma.
A)
B-mode. Space-occupying formation of the VI-VII segment of the right lobe of the liver, heterogeneous, predominantly of increased echogenicity, with small hypoechoic zones, with smooth, clear contours, and a hypoechoic rim.
b)
Color flow mode. The formation is poorly vascular, with a lack of internal blood flow.
Rice. 3.
Ultrasound picture of liver metastasis.

A)
B-mode. In the posterior diaphragmatic parts of the liver, a volumetric formation measuring 50 x 37 mm, tissue density, isoechoic, heterogeneous in echostructure, with a pronounced hypoechoic rim is visualized.
b)
Color flow mode. The formation is avascular.
Treatment of nodular hyperplasia
FNH requires dynamic monitoring using radiological methods [8]. Considering nodular hyperplasia a hypervascular formation, some authors consider chemoembolization of the hepatic artery to be an effective treatment for this pathology [1, 2, 5], while others recommend surgical treatment [4, 6].
Clinical observation 1
Patient G. was admitted with a diagnosis of chronic gastroduodenitis.
Ultrasound revealed a formation in the liver (Fig. 4).
Rice. 4.
Ultrasound picture of FNH of the liver in patient G.

A)
B-mode. In the left lobe of the liver, in segment III, a hypoechoic formation measuring 28 x 16 mm, with clear, even contours, is visualized subcapsularly.

b)
Color flow mode. The “feeding” artery is determined.
A CT scan (Fig. 5) confirmed the diagnosis of FNH.
Rice. 5.
Computed tomograms of FNH of the liver in patient G.

A)
Native phase. In the CII-III projection of the left lobe of the liver, a focal formation of low density is determined, with a fairly dense contour, measuring 27 x 15 mm.
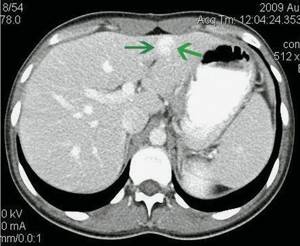
b)
Arterial phase. During intravenous contrast, the contrast agent accumulates diffusely and intensely “in the form of a flash” in the arterial phase.
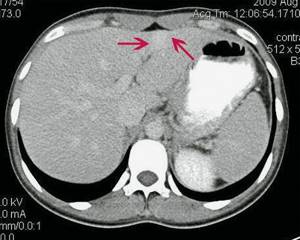
V)
Excretory phase. In the delayed phase, there is a slow washout of the contrast.
Clinical observation 2
Patient R. was admitted with a diagnosis of axial cardiofundal hernia of the esophageal diaphragm.
Ultrasound revealed a formation in the liver (Fig. 6), which was assessed as FNH by CT scan of the liver (Fig. 7).
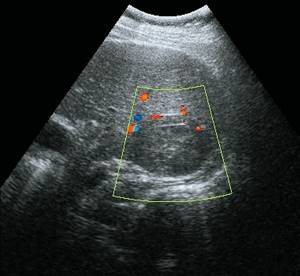
Rice. 6.
Ultrasound picture of FNH of the liver in patient R.

A)
B-mode. In the right lobe of the liver, a hypoechoic formation up to 20 mm in size, with clear, even contours, is visualized.

b)
Color flow mode. The “feeding” artery is determined.
Rice. 7.
Computed tomograms of FNH of the liver in patient R.
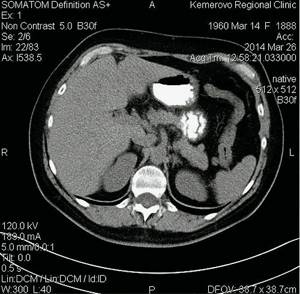
A)
Native phase.

b)
Arterial phase.

V)
Excretory phase.
At the CVIII/VII border there is a rounded formation measuring 15 x 15 x 18 mm, visualized only in the arterial phase. Conclusion: hypervascular formation of the right lobe of the liver. CT image of FNG.
In the described clinical observations, diagnostic puncture of the formations was performed under ultrasound guidance. Histological verification: FNH of the liver. Dynamic observation is recommended.
Conclusion
Thus, FNH is a rare liver disease that is detected incidentally during ultrasound. A CT scan of the abdominal cavity should be mandatory in the differential diagnostic search. The combined use of ultrasound and CT in some cases makes it possible to make the correct diagnosis and avoid the need for a puncture biopsy or diagnostic laparotomy. In doubtful cases, in our opinion, it is necessary to perform a biopsy of the formation followed by histological verification.
Literature
- Akinfeev V.V., Dudarev V.S., Dzyuban V.P., Khoruzhik S.A., Karman A.V., Rebeko I.V., Zharkov V.V., Dorosh D.D., Rusinovich V. M., Shavlikova L.A. // Materials of the 5th Congress of Radiation Diagnosticians of Belarus. November 3-4, 2005 Minsk, 2005: 316-319.
- Dudarev V.S., Anikfeev V.V., Dzyuban V.P., Fradkin S.Z., Mashevsky A.A., Zharkov V.V., Kokhnyuk V.T., Rebeko I.V., Dorosh D. .D. Diagnostic and interventional radiology for tumor diseases of the liver // Materials of the 5th Congress of Radiation Diagnosticians of Belarus. November 3-4, 2005 Minsk, 2005: 327-329.
- Zubarev A.V. New possibilities of ultrasound in the diagnosis of space-occupying lesions of the liver and pancreas // Echography. 2000; 2: 140-146.
- Ivashkin V.G. Diseases of the liver and biliary tract. M.: M-Vesti, 2005. 536 p.
- Kuntsevich G.I., Gavrilin A.V., Vishnevsky V.A., Burtseva E.A. Complex ultrasound diagnostics of metastatic liver disease // Ultrasound diagnostics. 2004; 3: 13-20.
- Kovalenko Yu.A., Zhao A.V., Chugunov A.O. Choosing the scope of surgical intervention for focal liver diseases // Annals of Surgical Hepatology. 2009; 14 (4): 79-87.
- Ratnikov V.A., Lubashev Ya.A. Difficulties and errors in diagnosing liver diseases using complex MRI // Proceedings of the 9th Russian conference “Hepatology today”. March 22-24, 2004 Moscow // Russian Journal of Gastroenterology, Hepatology, Coloproctology. 2004; 1 (Appendix No. 12): 59.
- Shakhijanova S.V., Shariya M.A. Diagnosis of focal nodular hyperplasia of the liver (data from a comprehensive examination - magnetic resonance imaging, computed tomography, ultrasound // Bulletin of Radiology and Radiology. 2001; 1: 43-45.
- Attal P., Vilgrain V., Brancatelli G., Paradis V., Terris B., Belghiti J., Taouli B., Menu Y. Telangiectatic focal nodular hyperplasia: US, CT, and MR imaging findings with histopathologic correlation in 13 cases // Radiology. 2003; 228 (2): 465-472.
- Buscarini E., Danesino C., Plauchu H., de Fazio C., Olivieri C., Brambilla G., Menozzi F., Reduzzi L., Blotta P., Gazzaniga P., Pagella F., Grosso M., Pongiglione G., Cappiello J., Zambelli A. High prevalence of hepatic focal nodular hyperplasia in subjects with hereditary hemorrhagic telangiectasia // Ultrasound Med Biol. 2004; 30 (9): 1089-1097.
- Bleuzen A., Tranquart F. Incidental liver lesions: diagnostic value of cadence contrast pulse sequencing (CPS) and SonoVue // Eur Radiol. 2004; 14 (Suppl. 8): 53-62.
- Fabre A., Audet P., Vilgrain V., Nguyen BN, Valla D., Belghiti J., Degott C. Histologic scoring of liver biopsy in focal nodular hyperplasia with atypical presentation // Hepatology. 2002; 35 (2): 414-420.
- Harvey CJ, Albrecht T. Ultrasound of focal liver lesions // Eur Radiol. 2001; 11: 1578-1593.
- Kehagias D., Moulopoulos L., Antoniou A., Hatziioannou A., Smyrniotis V., Trakadas S., Lahanis S., Vlahos L. Focal nodular hyperplasia: imaging findings // Eur Radiol. 2001; 11 (2): 202-212.
- Kudo M., Tochio H., Zhou P. Differentiation of hepatic tumors by color Doppler imaging: role of the maximum velocity and the pulsatility index of the intratumoral blood flow signal // Intervirology. 2004; 47 (3-5): 154-161.
- Leen E., Moug SJ, Horgan P. Potential impact and utilization of ultrasound contrast media // Eur Radiol. 2004; 14: 16-24.
- Schmitz D., Kohler HH, Heussel CP, Lohr HF, Galle PR Lymphoma-simulating presentation of focal nodular hyperplasia (FNH) of the liver // Z Gastroenterol. 2001; 39 (3): 219-224.
- Ye Q., Tang Z., Ma Z., Wu Z., Fan J., Qin L., Wang W. Differential diagnosis between hepatic focal nodular hyperplasia and hepatocellular carcinoma with negative alhpa-fetoprotein // Zhonghua Gan Zang Bing Za Zhi . 2000; 8 (3): 136-138.
Ultrasound scanner HS50
Affordable efficiency.
A versatile ultrasound scanner with compact design and innovative capabilities.
What does an ultrasound of the liver show?
Ultrasound of the liver allows you to evaluate the size, structure, location of the organ and its parts, the presence of any formations (cysts, tumors, metastases, etc.), inflammatory changes, pathological foci, traumatic injuries. In addition, an ultrasound of the liver makes it possible to evaluate the surrounding tissues, lymphatics and blood vessels.
Ultrasound results can detect the following liver pathologies:
- Hepatitis (acute and chronic);
- Cirrhosis of the liver;
- Hepatosis (fatty liver);
- Pathological foci in the liver (abscess, echinococcosis);
- Benign neoplasms in the liver (cysts, tumors, foci of nodular hyperplasia);
- Malignant neoplasms in the liver (cancer or metastases);
- Changes in the structure and condition of the liver caused by heart disease and heart failure.
Indications
An X-ray of the liver and biliary system helps to see the structure and size of the organs being examined. There are many computer diagnostic methods, such as MRI, ultrasound, CT, but X-ray studies using contrast are the most informative. The examination method is chosen by the doctor. Indications are the diagnosis of such diseases:
- cirrhosis;
- malignant and benign tumors;
- dysfunction of the liver and gallbladder;
- disruption of the biliary tract.
Contraindications for liver ultrasound
In principle, there are no absolute contraindications to performing an ultrasound scan of the liver, since this study is safe and non-invasive (that is, it does not involve the introduction of instruments into any parts of the body). However, if there are burns, wounds, pustular rashes or any damage to the integrity of the skin on the skin of the abdomen and sides, then ultrasound is not recommended, since pressure and sliding of the sensor can provoke the spread of the existing pathological process over a large area. Therefore, if you have wounds or skin diseases in the abdominal area, it is recommended to postpone a routine liver ultrasound until the skin is clear. If an ultrasound of the liver needs to be done on an emergency basis, it is performed despite the damage and pathological rashes of the skin of the abdomen.
In addition, liver ultrasound may be contraindicated for women in the third trimester of pregnancy (from the 27th week until childbirth), since during this period the significantly increased size and weight of the uterus puts strong pressure on all abdominal organs and, as it were, “ “closes” them from the ultrasound scanner, located directly under the abdominal wall.
In cases where a person is bothered by sharp abdominal pain, due to which he cannot take the position necessary for the study, liver ultrasound is also contraindicated.
It is advisable to postpone ultrasound of the liver for several days (3–5 days) after fibrogastroduodenoscopy (FGDS), X-ray of the stomach with contrast, or laparoscopic surgery.
Contraindications for the study
Due to some limitations in the study, computed tomography of the abdominal organs cannot be recommended for a number of patients. Thus, it is absolutely prohibited for pregnant women, for whom it poses a threat due to the possible teratogenic effect of X-rays on the fetus.
Also, this diagnostic method is not used in people suffering from obvious obesity. If the subject's body weight is more than 200 kg, the procedure cannot be performed even on the most modern and powerful CT machines. This contraindication is not exclusive to CT scanning; other studies also include restrictions on weight or fat pad thickness. For example, ultrasound is most often impossible for patients weighing about 150 kg, and “average” models of radiography machines are not intended for diagnostics in people weighing over 100-120 kg.
Preparing for diagnosis
Special preparation for liver CT is not required unless the procedure is supplemented with contrast. Preparing for a liver CT scan with contrast is not difficult. It consists in the fact that you should not eat food before the examination.
Preparation for liver ultrasound
It is advisable to carry out a routine liver ultrasound after preparation, which consists of abstaining from food for 8–10 hours and preventing intestinal flatulence.
Ultrasound of the liver is optimally performed on an empty stomach after an 8-10 hour fast. To ensure such an 8-10 hour period of fasting, you should subtract these 8-10 hours from the time for which the liver ultrasound is scheduled, and from this calculated moment you should not eat. It is acceptable to perform an ultrasound of the liver after at least a 6-hour fast. If the study is carried out not in the morning, but in the afternoon or evening, then in order to avoid too long a fasting period, on the day of the study you can eat dried white bread (crackers without additives, salt, flavor enhancers, flavorings, seasonings, etc.) and drink unsweetened tea .
To eliminate and prevent flatulence, it is necessary for two to three days before the study to stop consuming foods that promote increased gas formation in the intestines, such as carbonated water, whipped cream, nuts, pasta, honey, mustard, fatty meats and fish, alcohol. , vegetables (cabbage, radish, onion, garlic, bell pepper, etc.), fruits (melon, bananas, sweet apples, etc.), brown bread, dairy products, legumes (peas, beans, lentils, etc.) and other types of food containing large amounts of fiber. During the day before the study, you must also stop drinking plant juices.
If a person suffers from diseases of the intestines or other organs of the digestive system, then to exclude flatulence, in preparation for an ultrasound scan of the liver, in addition to following a diet, it is recommended to take medications for two to three days before the study that eliminate excess gas formation in the intestines (Carbolen 3 – 9 tablets per day and enzyme agents (Creon, Panzinorm, Mezim, etc.) 3 – 6 tablets per day). In addition to Carbolen and enzyme preparations, to prepare for an ultrasound of the liver in order to eliminate gas formation in the intestines, you can also take products with simethicone (Espumizan, Disflatil, etc.) 2 capsules 3 times a day, or activated carbon 2 tablets 3 times a day. Products containing simethicone and activated carbon to eliminate flatulence are taken for 2 to 3 days before an ultrasound scan of the liver.
Since an ultrasound of the liver is optimally carried out against the background of a non-bloated and empty bowel, then on the evening before the study you need to drink a mild laxative (for example, Duphalac, Mucofalk) or in the morning on the day of the ultrasound, give an enema or use glycerin suppositories.
When an ultrasound of the liver needs to be performed on an emergency basis, it is done without any preliminary preparation. But if inaccurate data were obtained during an emergency ultrasound, then after some time the study should be repeated as planned with the necessary preliminary preparation.
You need to take paper napkins, toilet paper or a towel with you to the clinic, which can be used to wipe off the gel from the abdomen, which is applied to improve the quality of the image obtained on the monitor of the ultrasound machine. In addition, if hunger is poorly tolerated by a person, then you can take a packed lunch with you to have breakfast immediately after the ultrasound.
If a person is constantly taking any medications, then there is no need to stop them before performing an ultrasound of the liver.
In children, preparation for a liver ultrasound consists of abstaining from eating and drinking any food (including water) for three hours before the examination. Of course, such preparation of children is carried out only in cases where they can easily tolerate fasting and lack of water.
How is a liver ultrasound performed?
An ultrasound of the liver is performed in a specially equipped room, in which an ultrasound machine, a couch and curtains are installed.
For the examination, the patient must expose his stomach by removing or lifting up his upper part of clothing, and then sit on the couch in the position indicated by the doctor. Typically, an ultrasound of the liver is performed in the supine position, less often - lying on the left side. In some cases, when the patient cannot lie on his back or left side, an ultrasound of the liver is performed in a standing or sitting position. After taking the required position, the doctor applies a special gel to the skin of the abdomen, which is necessary to obtain the best quality image. Next, the doctor moves the ultrasound machine sensor over the surface of the abdomen, obtaining an image of the liver from different angles, which is necessary for a detailed study of the condition of all parts and departments of the organ. During the examination, the doctor will definitely ask the patient to breathe at a normal rhythm, and also to inhale and exhale as much as possible. Images of the liver in different phases of breathing and against the background of different intensities of respiratory movements allow us to obtain the most detailed information about the state of the organ and its structures. In addition, during the ultrasound, the doctor may ask you to take a certain position, which is also necessary for a comprehensive assessment of the condition of the liver or identification of detected pathological changes.
After completing the study of the condition of the liver and taking all the necessary measurements, the ultrasound examination is considered complete. The doctor removes the sensor from the surface of the abdomen, and the patient can get dressed and leave.
The procedure for ultrasound examination of the liver is usually short and takes 10–20 minutes, depending on the qualifications of the doctor, the type of ultrasound machine and the patient’s body weight. The thinner the patient, the faster the doctor can assess all parameters of the liver’s condition. In obese patients, on the contrary, the study may take longer, since the subcutaneous fat layer makes it difficult to visualize the organ and forces one to examine the same area several times.
After completing the ultrasound examination, the doctor writes a protocol with a mandatory conclusion, which he hands over to the patient.
Normal liver ultrasound
Liver ultrasound indicators
During the ultrasound examination, it is necessary to determine the size and contours of the liver, assess the condition of the echo structure (homogeneous, heterogeneous), intrahepatic bile ducts, and large vessels.
In addition, the presence of any inclusions and formations that are uncharacteristic of the normal echostructure of the liver is detected. In more detail, based on the results of an ultrasound scan of the liver, the following parameters must be assessed:
- Shape, contours and anatomical structure of the organ;
- The dimensions of the entire liver and each of its lobes;
- Structure and echogenicity of the liver;
- The state of the vascular pattern of the organ as a whole;
- Assessment of the condition of large vessels and intrahepatic bile ducts;
- Identification of focal changes and pathogenic formations;
- Distinguishing various pathological changes from each other with the assumption of which pathological process is taking place in a particular case.
Normally, the main indicators assessed during ultrasound should be as follows:
- The angle of the lower edge of the left lobe of the liver is less than 45 o;
- The angle of the lower edge of the right lobe of the liver is less than 75 o;
- The oblique vertical size of the right lobe of the liver is up to 150 mm;
- The thickness of the right lobe of the liver is up to 140 mm;
- The craniocaudal size of the left lobe of the liver is up to 100 mm;
- The thickness of the left lobe of the liver is up to 80 mm;
- Liver width – 230 – 270 mm (23 – 27 cm);
- Liver length – 140 – 200 mm (14 – 20 cm);
- The transverse size of the liver is 200 – 225 mm (20 – 22.5 cm);
- Portal vein (measured at a distance of 20 mm from the confluence of the mesenteric and splenic veins) – 10 – 14 mm;
- Hepatic veins (measured at a distance of 20 mm from the mouth) – 6 – 10 mm;
- Inferior vena cava (measured at the level of the caudate lobe of the liver) – 15 – 25 mm;
- Hepatic artery (measured at 20 mm from the porta hepatis) – 4 – 6 mm;
- Lobar bile ducts – 2 – 3 mm;
- Common bile (hepatic) duct – 4 – 6 mm;
- The edges of the liver are normally smooth and clear;
- The structure of the parenchyma is normally fine-grained, homogeneous, consisting of many evenly distributed small point and linear structures;
- Echogenicity is normally the same or slightly higher than the echogenicity of the renal cortex;
- Sound conductivity is normally high (deteriorates with diffuse changes in liver tissue, for example, with fibrosis, fatty inclusions with hepatosis, etc.).
Liver size by ultrasound
Normally, the total width of the liver is 23 - 27 cm, length - 14 - 20 cm, and diameter - 20 - 22.5 cm. The thickness of the left lobe of the liver should not exceed 8 cm, and the right lobe - 14 cm. If the size of the liver is increased, then such an enlargement of the organ is called hepatomegaly, which indicates pathology. It is possible to understand what kind of pathology we are talking about in a particular case by taking into account the results of other parameters of liver ultrasound.
Normal ultrasound picture of the liver
The echogenicity of the liver is normally uniform, and is somewhere between the echogenicity of the pancreas (which is higher) and the echogenicity of the spleen (which is lower). In addition, the echogenicity of the liver is normally the same as or slightly higher than the echogenicity of the renal cortex.
Interpretation of liver ultrasound
What do changes in various liver ultrasound parameters indicate?
Below we will look at which pathologies are characterized by changes in one or another liver ultrasound parameter.
Increased size with a homogeneous fine-grained echo structure.
When the liver is large, but its structure is normal and homogeneous, this may indicate the following pathologies:
- Heart failure. In addition, ultrasound will reveal dilated hepatic veins, which are not normally visible. The diameter of the inferior vena cava does not change depending on inhalation and exhalation.
- Acute hepatitis. Usually, no other specific changes other than an increase in the size of the organ are detected on ultrasound during acute hepatitis. The overall picture is quite normal.
- Tropical hepatomegaly. Additionally, ultrasound also reveals a significantly enlarged spleen (splenomegaly).
- Schistosomiasis. In addition to an increase in the size of the liver, with this disease, ultrasound shows a thickening of the portal vein and its large branches, and their walls and surrounding tissue are very bright. In some cases, an enlarged splenic vein and the spleen itself are also visible. When infected with Schistosoma mansoni or Schistosoma japonicum, ultrasound may also show fibrosis of the tissue around the portal vein.
Increased size with heterogeneous echo structure.
An enlarged liver with a heterogeneous structure may indicate the following pathologies:
- If the liver is enlarged, has a heterogeneous structure, but no focal formations are identified in it, then this may be a sign of cirrhosis, chronic hepatitis or fatty hepatosis. With these pathologies, ultrasound, in addition to an increase in the size and heterogeneous structure of the liver, shows an increase in its echogenicity (hyperechoic parenchyma) and a decrease in the number of visible branches of the portal vein. In some cases, sound conductivity is significantly reduced, as a result of which the deep-lying parts of the liver are not visible at all.
- If the liver is enlarged, has a heterogeneous echogenic structure and multiple or single focal formations of any shape, size and echostructure are visible in it, then this is a sign of macronodular cirrhosis, abscesses, metastases, lymphoma or hematoma. In macronodular cirrhosis, an altered vascular pattern, normal stroma and numerous formations of different sizes are additionally visible on ultrasound. In case of abscesses, ultrasound additionally detects increased echogenicity and multiple or single formations with unclear contours are visible. With metastases, ultrasound additionally shows formations of various shapes, sizes and echostructures. In lymphoma, multiple hypoechoic (light-colored) structures with unclear contours and without distal acoustic enhancement are additionally visible. With hematomas, ultrasound shows formations with unclear contours and distal acoustic enhancement.
Reduction in liver size
may be characteristic of micronodular cirrhosis. At the same time, ultrasound additionally records an increase in echogenicity and deformation of the organ due to scarring (overgrowth) of the portal and hepatic veins. In this case, the portal vein is usually normal or collapsed inside the liver and enlarged outside the liver. Sometimes numerous structures representing blood clots are visible inside the portal vein. Micronodular cirrhosis may be associated with ascites (fluid in the abdominal cavity), portal hypertension (increased pressure in the portal vein of the liver), dilatation and varicose veins of the splenic vein, and splenomegaly (enlarged spleen).
Cystic formations in the liver
can be different, as they are provoked by different reasons.
Thus, in the liver, ultrasound may show a solitary cyst, which is an anechoic (light) round formation with clear or uneven contours and a diameter of less than 30 mm. Such cysts usually do not cause any clinical manifestations and are congenital, and therefore harmless. But, unfortunately, a solitary cyst cannot always be distinguished from a parasitic cyst, therefore, if such a formation is detected in the liver, it is recommended to perform a biopsy.
Also, ultrasound can reveal multiple liver cysts, which usually have the appearance of anechoic (light) formations of various diameters with a clear contour and acoustic enhancement. Typically, such multiple cysts are a manifestation of congenital polycystic disease, and are often combined with cysts in the kidneys, spleen and pancreas.
If the cysts become complicated, hemorrhages or suppuration occur in them, then on ultrasound such formations are visible as abscesses or disintegrating tumors.
Finally, one of the most difficult from a diagnostic point of view are parasitic (echinococcal) cysts, which are formed due to the penetration of parasites into the liver. Any parasitic cyst on ultrasound may have various echogenic signs, depending on the stage of development of the parasite and the condition of the cystic walls and cavities. Thus, a parasitic cyst may look like a simple light-colored formation with a clear contour and distal acoustic enhancement, similar to a solitary cyst. In other cases, the cyst may have a double wall contour. In the third variants, “parasitic sand” or a septum is visible inside the cystic formation, freely moving in the cavity of the cyst. In fourth cases, multiple small cysts and blisters are visible inside the large cyst, which usually indicates the presence of a living parasite in the liver. When the parasite has already died, the cyst may acquire a clear outline due to calcification (calcification) of its walls.
Single solid mass in the liver
may be a hemangioma, abscess, festering cyst, metastasis, hepatoma. Unfortunately, it is very difficult to distinguish these formations based on ultrasound results, therefore, if a serious disease is suspected, a biopsy is recommended. Most often, single solid formations in the liver are represented by hemangiomas (up to 75% of cases).
Ultrasound picture characteristic of various liver diseases
In this section we will look at what ultrasound signs of various liver pathologies.
Cirrhosis. With this pathology, the size of the entire liver or only its left lobe is increased, the echogenicity of the organ is increased, sound conductivity is reduced, its structure is heterogeneous, mosaic, the edges are lumpy and uneven, the vascular pattern is disrupted due to the increased diameter of the portal vein.
Hepatitis. With this pathology, the entire liver or only one lobe of it (right or left) is enlarged, the contours are smooth and clear, the edges are rounded, echogenicity is reduced, sound conductivity is increased, the structure is heterogeneous, mottled, the vascular pattern is changed due to the expansion of the portal and splenic veins, as well as contrasting other vessels.
Fatty hepatosis.
With this pathology, the size of the liver is increased, the angle of the lower lobe is more than 45 o, the structure is heterogeneous, possibly variegated, echogenicity is increased, sound conductivity is reduced, the contours are smooth but unclear, the edges are rounded, and the portal vein is not visible.
Liver tumors.
Ultrasound shows areas with unclear contours that are more or less echogenic compared to the rest of the liver tissue. Less echogenic (hypoechoic) tumors are sarcomas, lymphomas, hemangiomas, adenomas, hepatocellular cancer, low-grade cancer. More echogenic (hyperechoic) tumors are hepatomas and cancer metastases to the liver. Also, with tumors, ultrasound shows enlargement of the lymph nodes and displacement of the gallbladder from its normal position.
Liver cysts.
With these pathological formations, ultrasound shows single or multiple structures with clear edges, which lead to an increase in size or bulges in certain areas of the liver.
Giardiasis.
Ultrasound shows areas of calcium salt deposition and zones of reduced echogenicity, which are areas of parasite accumulation. Secondary diffuse changes with
heart diseases. On ultrasound, the contours of the liver are smooth and clear, the size of the organ is increased, the edge is rounded, the structure is heterogeneous, echogenicity is increased, sound conductivity is reduced, the inferior vena cava and hepatic veins are dilated.
Abscess. Ultrasound shows round or irregularly shaped formations with a clear wall, varying echogenicity and moving contents.
How is the procedure carried out?
The tomograph is a ring to which a movable diagnostic table is attached. The patient is placed on the table lying on his back. They warn you to remain still. Slide the table inside the device. During the scan, the upper abdominal cavity is irradiated. The absorption of rays by tissues is recorded by sensors. The image is obtained as the computer processes all received pulses.
In most cases, a CT scan of the liver with contrast is performed. The patient is given a contrast agent intravenously. It allows you to clearly visualize the boundaries of all organs in the studied area and separate them from each other. In the presence of neoplasms and anomalies, contrast helps to accurately determine their size and density. Before this test, the doctor should ask the patient about an allergy to iodine.
Normal picture
Normally, liver tissue is homogeneous and has a slightly higher density than tissue of the pancreas, kidneys and spleen. Areas of lower density, linear or rounded, against the background of homogeneous parenchyma correspond to liver vessels. The portal vein is usually visualized, but the hepatic artery is not. Intravenous administration of a contrast agent reduces the difference in density between the vessels and the parenchyma.
Intrahepatic bile ducts are usually not visible on tomograms, but the common hepatic and common bile ducts are often visualized as low-density structures. Due to the fact that bile is close in density to water, intravenous administration of a contrast agent leads to a clearer distinction of the bile ducts from the surrounding parenchyma and liver vessels.
The gallbladder is visualized as a round or elliptical formation, which, like the bile ducts, has low density. The contracted gallbladder may not be visualized (therefore, studies must be performed on an empty stomach).
Deviation from the norm
Pathological formations of the liver in most cases have a lower density than its unchanged parenchyma. CT can distinguish fairly small lesions. Using intravenous contrast scanning, it is possible to better distinguish pathological lesions from normal parenchyma due to increased parenchymal density.
Primary liver tumors or metastases have the appearance of rounded formations with a density slightly less than the density of unchanged parenchyma, and with clear or blurred boundaries. However, sometimes the tumor cannot be detected, since it does not differ in density from the surrounding parenchyma. Sometimes a large tumor deforms the contours of the liver. Liver abscesses have the appearance of homogeneous hypoechoic foci, usually with clear boundaries. Liver cysts are round or oval in shape, have sharply defined boundaries, and are less dense than abscesses and tumors.
The density of liver cancer depends on its stage. A fresh thrombus is denser than normal parenchyma; the density of an organizing thrombus is less than the density of liver parenchyma. Intrahepatic hematomas have different shapes; subcapsular hematomas are shaped like a sickle and push the liver parenchyma away from the capsule.
In the differential diagnosis of obstructive jaundice and other types of jaundice, attention is paid to the condition of the bile ducts; expansion of the latter is a sign of obstructive jaundice, while their normal diameter indicates non-obstructive jaundice. Dilated intrahepatic bile ducts look like branching linear and round structures of low density against the background of homogeneous liver parenchyma. Depending on the level of obstruction, dilation of the common hepatic duct, common bile duct and gallbladder may also be observed. Mild dilatation of the bile ducts is easier to detect by contrast.
CT scans can usually identify the cause of biliary obstruction, such as gallstones or cancer of the head of the pancreas. However, if it is necessary to know the location of the obstruction before surgery, percutaneous transhepatic cholangiography or endoscopic retrograde cholangiopancreatography (less frequently) is also used.










