Arthroscopy is an operation that involves taking an image from inside a joint using a special camera called an arthroscope. The arthroscope allows you to obtain high-quality magnified images from the inside of the joint through a small skin incision of only 7-8 mm in length, which avoids open surgery. Under the control of an arthroscope, other approaches to the knee joint are made, through which special instruments are introduced, with the help of which it is possible to solve many problems inside the joint.
Although small incisions are used, the volume of operations during arthroscopy can be very large, and often those operations performed arthroscopically cannot be adequately performed openly.
Arthroscopic interventions do not require long-term hospitalization; in the vast majority of cases, 1-2 days in hospital is sufficient.

The main indications for knee surgery are the following diseases and symptoms:
Meniscus tear
Osteoarthritis of the knee joint
A torn meniscus is the most common reason for arthroscopic knee surgery. Menisci are cushions made of cartilage-like tissue that help the knee better absorb stress during walking, running, jumping and other activities. If the meniscus ruptures, its fragments can injure the articular cartilage and cause episodes of joint locking. Traumatization of the articular cartilage over time leads to the development of arthrosis of the knee joint. In 95% of cases, partial resection of the damaged meniscal fragment is required. In 5% of young active patients with certain types of tears, a meniscus suture may be performed. Recovery from meniscus surgery varies depending on the size of the tear and can range from 2-3 weeks to 5-6 months.

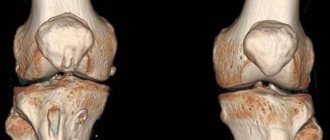
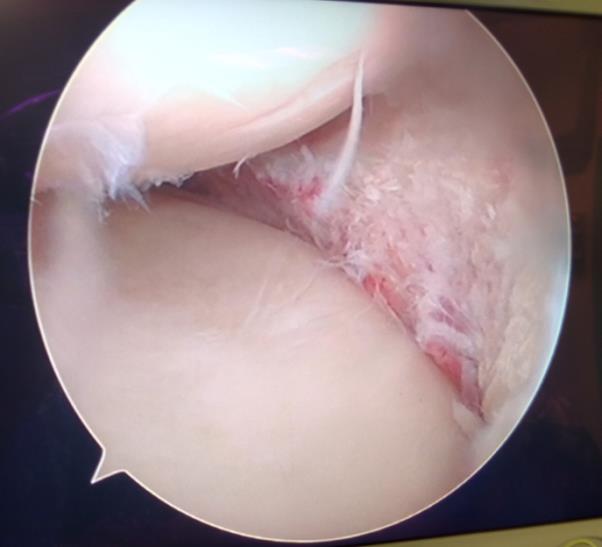
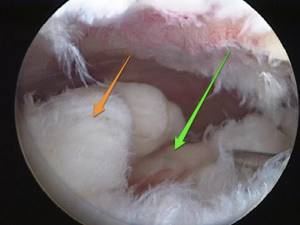
A “watering can handle” tear of the internal meniscus with a block of the knee joint (inability to fully straighten the knee joint). The photograph clearly shows a large fragment of the meniscus tightly sandwiched between the articular surfaces of the femur and tibia.

Degenerative combined rupture of the body and posterior horn of the internal meniscus of the knee joint.

Longitudinal rupture of the posterior horn of the external meniscus, accompanied by its hypermobility. With such a rupture, the meniscus can significantly shift inside the joint creating a sensation of a mechanical block, a foreign body, instability in the joint, jamming, or clicking.
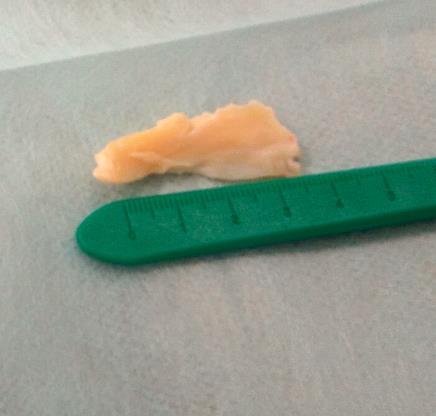
A removed fragment of the internal meniscus with a rupture similar to a watering can handle with a block of the knee joint.
Meniscus after treatment for a paracapsular subtotal watering can handle tear.
Do I need special preparation for arthroscopy?
At your first appointment with your orthopedist, you will be told how to prepare for the procedure. The doctor will ask what medications you are taking and may make adjustments to them.
- It is recommended to stop taking aspirin and ibuprofen for several days or weeks before the procedure.
- You should not eat or drink for 6-12 hours the day before.
- If necessary, you will be prescribed additional pain medications.
How is arthroscopy used to determine the cause of knee pain? A practicing orthopedic surgeon-traumatologist tells and shows:
Changes in the articular cartilage of the knee joint.
Articular cartilage is a smooth, elastic and strong connective tissue covering the bones that form a joint. This allows the bones to slide freely against each other at the articular joint. In cases of injury, increased wear and tear, or certain metabolic disorders, cartilage can wear away, causing pain and limited range of motion. Arthroscopy does not cure arthritis or arthrosis, but it can reduce pain and allow partial restoration of the cartilage covering of the bones in the joint through interventions such as chondroplasty, debridement and microfracture, and a number of others.

Longitudinal cracks in the tibial cartilage following an episode of buckling following a rupture of the anterior cruciate ligament of the knee.

Degenerative changes in the articular cartilage of the knee joint appear against the background of damage from a torn meniscus.
Preparatory stage
Before undergoing arthroscopy, the patient must be properly prepared. First of all, a general examination is carried out to assess the patient's condition. It includes general urine and blood tests, ECG, fluorography, coagulogram. Tests are also carried out to identify possible severe infections (viral hepatitis, HIV, syphilis).
Preparation for surgery includes compliance with the following rules:
- stop taking any medications for two weeks (except for vital ones, but you must inform your doctor about this);
- the last meal should occur no later than 8-12 hours;
- Before the procedure, the patient needs to buy crutches, since it will be impossible to walk without them at first (doctors recommend learning how to use these devices in advance and understanding the principle of their operation).
The day before the operation, the doctor conducts a conversation with the patient, explaining what the intervention is, how it will happen, and enlightens about the possible consequences. The specialist also gives recommendations on rules of conduct during the recovery period.
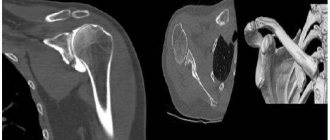
Free intra-articular body of the knee joint.
Loose intra-articular bodies are most often formed as a result of detachment of cartilage or osteochondral fragments, large fragments of the menisci. Moving freely inside the joint, they can cause jamming of the joint, pain, clicking, sensation of a foreign body in the joint, and episodes of instability. In addition, when the articular bodies jam, they injure the articular cartilage and can lead to the development of arthrosis. Arthroscopically, it is not difficult to quickly and effectively remove the loose articular body, while simultaneously understanding the cause of its formation.

Free intra-articular body of the knee joint, consisting of a detached section of the cartilage of the internal femoral condyle against the background of its constant traumatization by fragments of a torn meniscus.

The free intra-articular body of the knee joint after removal, consisting of a detached section of the cartilage of the internal femoral condyle and the cause of the detachment is the degeneratively changed posterior horn of the internal meniscus.
Description of the microsurgical process
In reviews, patients tell how quickly and painlessly they underwent the procedure, without general anesthesia. This is quite likely, but do not forget that clinical cases are not the same for everyone, and the physiological status of each patient is different. Therefore, it would be more correct to say that pain, thanks to strong local anesthesia, is almost impossible. However, post-operative discomfort in the area of the operated area will most likely bother you a little for some time.
Disintegration of ligaments when they rupture.
The video allows you to understand all the intricacies of the process. There are plenty of them on the Internet. But due to the fact that not everyone will be able to watch specific stories to the end, we suggest that you simply and calmly read about the important points.

Positioning of the patient on the operating table.
Based on the etiology and degree of pathological changes, the patient’s condition and concomitant diseases, the anesthetic agent is selected individually. Most often, local anesthesia is used, that is, regional anesthesia (epidural or conduction). The regional anesthetic contains lidocaine, ropivacaine or bupivacaine. To enhance the anesthetic effect, a medicine from the opiate category can be added to the main solution in a mini-dose. In some situations, however, general intravenous anesthesia is appropriate.
First, regardless of the surgeon's plans, a diagnostic arthroscopy will be performed. It involves inserting an endoscopic probe in the form of a rod into the cavity of the bone joint. When anesthesia takes effect, then diagnostic surgery begins. To do this, the limb, half bent at the knee, closer to the thigh, is twisted to reduce blood flow, after which a puncture (6 mm) is made, through which a contrast agent is injected to enhance the visibility of the articular and periarticular structures. Next, a tube is inserted through this operating port. The specialist thoroughly examines every millimeter of the problem organ.

The surgical field, you can see a glow inside.
The video is broadcast in real time on the screen and reveals any existing defects in the diseased joint. If the doctor considers it necessary to perform regeneration of pathological elements, he will create an additional incision (6-8 mm), through which he will eliminate the detected defect using the necessary instrument from the microsurgical set. He can perform partial resection of osteochondral tissues, plastic surgery of ligaments and tendons, suturing or removal (partial, complete) of the meniscus, expropriate chondromic bodies, extract effusion and pus, administer anti-inflammatory drugs, take a fragment of tissue or synovium to study their composition, etc.
At the end of the surgery, the surgical field is washed and all instruments are removed. The doctor treats the wound with disinfectant compounds, installs drainage and makes a small suture, which he closes with a sterile adhesive plaster. On the operated knee, in order to give it maximum immobility, a tight fixing bandage is applied from the foot to the middle of the thigh.
The entire session takes an average of 1 hour, in some cases up to 3 hours. Restorative measures are simple, but they must be strictly followed so as not to provoke dangerous complications. Negative phenomena that can develop will be discussed further.
Damage to the cartilage of the knee joint.
The patella (or kneecap) can cause severe pain that is difficult to treat conservatively. Most often it occurs against the background of functional overload during sports or as a consequence of quadriceps muscle rigidity. Other causes of pain in this localization may be an outward displacement of the patella as a result of congenital features of the formation of the knee joint or as a consequence of its traumatic dislocation. Arthroscopy allows you to treat cartilage defects on the inner surface of the patella, reduce the degree of tension of its ligamentous apparatus, and fix the patella in an inwardly displaced position.
What are the benefits of treatment?
Compared to other methods that require full opening of the knee joint, arthroscopy is relatively less invasive, which is a great advantage for the patient. The incisions made during the procedure are painless, and the scars after them are small. After such a procedure, the patient can be discharged from the hospital within 1-2 days. Orthopedists choose to perform arthroscopy because it is more accurate than other imaging methods. In addition, arthroscopy allows you to evaluate the functioning of the joints during movement.
Arthroscopic restoration of the ligamentous apparatus of the knee joint.
After an injury, instability of the knee joint may occur as a result of rupture of one or more ligaments. The most common surgical intervention is performed for a torn anterior cruciate ligament. But in a number of cases, rupture of the posterior cruciate ligament, external and internal collateral ligament, ligamentous apparatus of the posterolateral part of the knee joint, ligamentous apparatus supporting the patella and a number of other injuries occur. Ligament reconstruction is performed using one's own allografts (for example, one's own semitendinosus and gracilis muscles), as well as cadaveric ligaments and synthetic analogues. The operations themselves are technically quite complex interventions, for this reason they will be discussed in separate articles.

Preparation of an autograft for plastic surgery of the anterior cruciate ligament due to its rupture.
How does the procedure work?
First, a special tube is inserted into the joint cavity. It is synchronized with ultra-strong lenses. A powerful light source is connected. Next comes a direct study with visualization of the picture on the display. The picture is displayed on the monitor in an enlarged size, so you can recognize the pathology and choose the right treatment. According to scientists, arthroscopy is a progressive technique in terms of diagnosis. So far there is no alternative to it in terms of information. The device clearly visualizes the condition of the joint down to the smallest detail. Moreover, they may not be noticed when doing CT and MRI.
The fact that the procedure is used not only for diagnostic purposes is also positive. It is good to use in the treatment and restoration of joints. Having discovered a violation, the doctor is able to immediately act on the affected areas using surgical manipulations. However, as with any operation, there are indications and contraindications.
Make an appointment
NEARMEDIC is a network of clinics throughout Moscow, equipped with operating rooms and hospitals, and provided with highly qualified specialists. Find the clinic that is most convenient for you on the map in the “Contacts” section and make an appointment with a surgeon. Below on the page you will find cards of surgeons and anesthesiologists with appointment addresses, photographs, short biographies, and reviews. Here you can make an appointment with your chosen doctor.
You can also make an appointment with a doctor through the appointment form on the website, by calling the general telephone number of the control room or by calling the clinic that you have chosen. Need some advice? Call us and we will be happy to answer your questions.
Possible contraindications and complications
It is important to note that arthroscopy is not performed for the following concomitant pathologies:
- skin rashes of the pustular type in the shoulder area;
- infectious diseases with localization of the focus in the shoulder joint;
- elevated body temperature, regardless of cause;
- previously diagnosed ankylosis;
- intolerance to painkillers/anesthetics.
Any surgical intervention comes with a risk of complications. But the degree of this risk is important. With the artoscopy method, these are minor complications that can only cause some discomfort to the patient. After joint arthroscopy, swelling and redness of the soft tissues may be observed in the areas where punctures and incisions were made. However, they disappear literally after 3-5 days.
It is extremely rare that deep veins may be damaged during surgery, but this is not dangerous for the patient. We are always able to quickly provide the necessary assistance.