Polycystic ovary syndrome (PCOS) is a serious pathology that leads to disruption of the ovulation process and the inability to conceive. Laparoscopy for PCOS is prescribed if there is no improvement in the condition within 4-5 months of conservative treatment.
During the operation, the volume of luteal tissue is surgically reduced. After this, the synthesis of androgen hormones in the female body is significantly reduced, which increases the chances of conception and pregnancy.
Laparoscopy for PCOS in our clinic is performed by experienced doctors using modern equipment, which guarantees high efficiency of treatment.
Indications and contraindications for surgery
Laparoscopy is prescribed in the following cases:
- inability to conceive as a result of the development of polycystic ovary syndrome;
- precancerous condition;
- rapid increase in the size of cysts, which can provoke their rupture with subsequent peritonitis;
- frequent and severe pain in the lower abdomen, characteristic of compression of neighboring organs by a cyst;
- hormonal disorders (hair loss, excessive sweating, hirsutism);
- menstrual irregularities.
Laparoscopy is not performed in the following conditions:
- pregnancy;
- chronic pathologies in the acute stage;
- oncology;
- blood clotting disorder;
- infectious or inflammatory processes in the acute stage;
- previous abdominal surgeries or serious illnesses within several months before laparoscopy.
Indications for surgery for fibroids
- Uterine bleeding or menstrual dysfunction;
- Rapid growth of nodes or the presence of a large tumor;
- Pain syndrome;
- Submucosal, subserous nodes, centripetal growth, as well as atypical location (intraligamentary, cervical, isthmus);
- Development of anemia;
- Dysuric manifestations;
- Infertility or miscarriage.
For a written consultation, in order to choose treatment tactics in your case, you can send me a complete description of the ultrasound of the pelvic organs, indicate your age and main complaints [email protected] [email protected] Then I will be able to give a more accurate answer to your situation.
How is laparoscopy performed for PCOS?
Laparoscopy is performed under general anesthesia. Special devices (laparoscope, instruments for manipulation) are inserted into the abdominal cavity through small punctures. To lift the walls of the peritoneum, providing a high-quality view and unobstructed manipulation, gas is pumped inside.
During the examination, the doctor sees all violations on the monitor and immediately removes them. After examining and sanitizing the cavity, sutures are applied. Depending on the extent of the pathology, the duration of the operation ranges from 30 to 60 minutes.
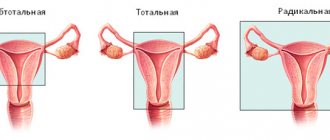
Laparoscopic hysterectomy (hysterectomy)
The first laparoscopic hysterectomy was performed by H. Reich in 1988. After this, many surgeons began to perform hysterectomy using a laparoscopic approach and create their own modifications of the operation. The laparoscopic approach began to gain widespread popularity and compete with other surgical approaches for removing the uterus - open abdominal (laparotomy) and vaginal. Currently, most hysterectomies can be performed laparoscopically, followed by removal of the uterus en bloc through the vagina or in separate fragments using a special surgical instrument - a morcellator. To date, the world has accumulated extensive experience in performing laparoscopic hysterectomy, demonstrating the effectiveness of the minimally invasive endoscopic approach.
Advantages of laparoscopic approach:
- Low traumatic surgical approach. Laparoscopic hysterectomy is not performed through a large incision on the anterior abdominal wall, but using 4 incisions up to 1 cm. One incision is made in the navel area. Through it, carbon dioxide is pumped into the abdominal cavity to create a working space and an optical camera is inserted, transmitting the image to the monitor. Two more incisions are made in the iliac regions, and the fourth is above the pubis. Through these three incisions, thin instruments are inserted into the abdominal cavity to perform surgery.
- Reducing the incidence of postoperative wound complications. Due to the fact that the operation is performed not through a large incision on the anterior abdominal wall, but through small incisions of 1 cm, the frequency of postoperative complications such as suppuration and hematomas is much lower during laparoscopic operations. Postoperative hernias in the area of trocar incisions after laparoscopic operations are generally extremely rare.
- Reducing postoperative pain. Low-traumatic laparoscopic approach requires significantly less painkillers in the postoperative period. Usually only non-steroidal analgesics are used, and there is no need to use narcotic painkillers. Typically, pain relief is necessary during the first 2 to 3 days of the postoperative period.
- Good cosmetic effect. After laparoscopic hysterectomy, 4 incisions of 1–1.5 cm each remain on the skin of the anterior abdominal wall. One of the incisions is hidden in the natural folds of the navel, and the other three are hidden under underwear. At the end of laparoscopic surgery, these skin incisions are usually closed with intradermal sutures using absorbable suture material, which creates maximum cosmetic effect.
- Early activation and discharge from hospital. After laparoscopic hysterectomy, patients usually become active (stand up, walk) from the first day of the postoperative period. Early activation is the prevention of a number of general surgical complications such as dynamic intestinal obstruction, bronchopneumonia, deep vein thrombosis of the lower extremities. Discharge from the hospital and return to the usual work and rest schedule occurs earlier than after traditional open abdominal operations.
Indications for laparoscopic hysterectomy:
1.Uterine fibroids. Indications for hysterectomy for fibroids are heavy menstruation leading to anemia, rapid growth of fibroids, large size of uterine fibroids, dysfunction of the bladder and rectum due to fibroids, malnutrition of fibroid nodes. The limits of the size and weight of the uterus at which laparoscopic hysterectomy is possible are arbitrary and are limited mainly by the experience of a particular surgeon. But laparoscopic hysterectomy is usually performed when the size of uterine fibroids is more than 24 weeks. rarely performed.
2. Adenomyosis.
3. Recurrent endometrial hyperplasia
4.Atypical endometrial hyperplasia
5. Malignant diseases of the internal genital organs
Contraindications to laparoscopic hysterectomy.
Laparoscopic hysterectomy, like other laparoscopic operations in gynecology, is performed under general anesthesia (anesthesia) in the Trendelenburg position. This is a position with the legs apart and bent and the head end of the operating table tilted 15 - 20º down. This position of the patient on the operating table promotes the displacement of the intestinal loops and greater omentum under the influence of gravity towards the diaphragm, revealing the pelvic cavity with the uterus and appendages. Another feature of laparoscopic operations is pneumoperitoneum, that is, the introduction of carbon dioxide into the abdominal cavity, which lifts the anterior abdominal wall from the internal organs, creating a safe working space. At the same time, a pressure of 12–15 mm Hg is created in the abdominal cavity. Art.
A prolonged position with the head down and increased intra-abdominal pressure during surgery may be contraindicated in some patients.
There are absolute and relative contraindications to laparoscopic hysterectomy.
Absolute contraindications:
- Acute myocardial infarction
- Acute cerebrovascular accident
- Uncorrectable coagulopathy (reduced blood clotting)
Relative contraindications:
- Chronic diseases of the cardiovascular, respiratory and central nervous systems in the stage of decompensation, which are a contraindication to anesthesia, Trendelenburg position and pneumoperitoneum
- Previous operations and adhesions in the pelvis and abdominal cavity
- Large uterus (more than 24 weeks)
- Atypical location of fibroid nodes (cervical, isthmus, intraligamentary)
Operation technique.
The operation begins with a puncture of the abdominal cavity with a special needle and the injection of several liters of carbon dioxide into it. In this case, a pressure of about 12–15 mmHg is usually created in the abdominal cavity. Art. This allows you to lift the abdominal wall away from the internal organs and work safely in the abdominal cavity. Carbon dioxide is used because it is non-flammable, which is important because laparoscopic surgery always uses electrosurgical instruments to stop bleeding and cut tissue. Next, an optical camera is inserted into the abdominal cavity through an incision in the navel area, which transmits the image to a video monitor. Thin working instruments are inserted through incisions in the lower anterior abdominal wall. After examining the abdominal and pelvic organs, the planned scope of the operation is finally confirmed. The second assistant surgeon inserts a special instrument into the uterine cavity from the vaginal side - a uterine manipulator, with the help of which the uterus moves during the operation. The uterine manipulator increases the safety of the operation by improving tissue tension, visualization of the vaginal vaults and moving the ureters away from the surgical site. Further stages of hysterectomy do not differ from those with open abdominal access. Technical difficulties during surgery can occur with large uterine sizes, low location of fibroid nodes, widespread external genital endometriosis, and adhesions in the pelvis. After cutting off the uterus from the vagina, it can be removed entirely through the vagina if its size does not exceed 9 weeks. Larger uteri have to be crushed in the abdominal cavity using a special tool - a morcellator, and then removed in parts. At the end of the operation, the instruments are removed, gas is removed from the abdominal cavity, and intradermal cosmetic sutures are placed on the skin incisions.
In addition to the classic total laparoscopic hysterectomy described above, there is the so-called laparoscopic-assisted vaginal hysterectomy. With this technique, some stages are performed through laparoscopic access, and some through vaginal access.
With laparoscopic hysterectomy there is always a risk of conversion to an open abdominal approach. This situation can occur with uncontrolled bleeding, injury to adjacent organs, or severe adhesions after other operations.
Postoperative period.
Patients are activated 1 day after surgery. During the normal course of the postoperative period, there are no restrictions on food and fluid intake from the 1st day after surgery. All patients undergo prolonged antibacterial prophylaxis with a broad-spectrum antibiotic for 48 hours after surgery. Prevention of thromboembolic complications is carried out with drugs of low molecular weight heparins (Fraxiparin, Clexane, Cibor, etc.), begins 12 hours before surgery and continues 12 hours after surgery until the patients are fully activated. Patients are discharged from the hospital 2–5 days after surgery.
Benefits of laparoscopy
Laparoscopy for polycystic ovary syndrome has a significant advantage compared to other surgical treatment methods:
- Minimally invasive. The doctor uses small incisions to access the pathological area. Due to the fact that tissue damage is minimal, the risk of bleeding is reduced to zero.
- High accuracy. During the operation, the doctor has the opportunity to act with pinpoint precision. As a result, all pathological areas must be removed. In this case, healthy tissues are not damaged.
- Safety. Due to the fact that there is no contact of the organ with any materials used during abdominal surgery, the likelihood of infection or complications is almost zero.
- The scars that remain after laparoscopy are almost invisible.
- Rapid healing of the scar and restoration of the body.
- The ability to remove during the operation any other pathologies that were identified directly during laparoscopy.
- Fast recovery. With hormonal therapy for polycystic disease, a woman is forced to take medications for months or even years. After laparoscopy, her body’s hormonal levels are immediately restored.
A few days after laparoscopy, the woman begins menstruation, and a few weeks later ovulation occurs. In rare cases, it may not occur for several cycles. In such a situation, the patient is additionally prescribed drug therapy.
According to statistics, within 6-12 months, 70-90% of women experience a long-awaited pregnancy.
If you have been diagnosed with PCOS, contact ImageLab for help. Our specialists will conduct an examination, select the optimal treatment methods and help you restore reproductive function.