Osteocalcin is a protein and hormone produced by osteoblasts, the cells that create bone tissue. It is released by osteoblast cells during bone formation and partially enters the blood. Osteocalcin is considered the most informative marker for assessing bone formation. It binds calcium in bones, participates in the formation of bone tissue and its regeneration.
As a hormone in the blood, osteocalcin is capable of:
- Increase insulin production by the pancreas (, )
- Change blood glucose levels ()
- Stimulate testosterone ()
- Improve brain function ()
Norms of osteocalcin
Approximately 95% of healthy adults have osteocalcin levels in their blood within the normal range of 11 – 48 ng/ml. But these indicators are typical for adults aged 30 to 50 years.
During the period of intensive growth of children and their puberty, osteocalcin values increase significantly within the range of 77 – 269 ng/ml. And with aging, the values of this protein seriously decrease and range from 14 to 46 ng/ml.
Osteocalcin production follows a circadian rhythm and varies throughout the day, reaching its peak in the early morning and its nadir at midday.()
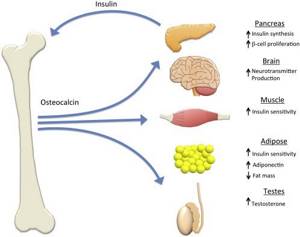
HORMONAL INFLUENCE OF OSTEOCALCIN ON METABOLISM IN THE BODY (https://www.sciencedirect.com/science/article/pii/S8756328215002355)
Action and effects of osteocalcin
Osteocalcin helps build strong bones
Osteocalcin is responsible for capturing and binding calcium in bone tissue, which gives bones their strength and flexibility. In order for this process to begin, osteocalcin must first be activated by vitamin K. () For example, mice with low levels of osteocalcin were found to have significantly weaker bones, which even led to bone fractures.()
However, elevated osteocalcin levels are not always a sign of bone strength. In older people, such a high level of this protein is, on the contrary, an indicator of decreased bone density (especially the femoral neck and spine), which can lead to serious fractures. These elevated osteocalcin levels are associated with numerous abnormalities in bone formation.(, , , , )
Osteocalcin regulates insulin and glucose levels
When osteocalcin works as a hormone, it is able to control the balance between insulin and glucose in the body.(And) In the pancreas, this protein increases insulin production by activating the GPRC6A receptors . This increases the production of beta cells in the pancreas, which then begin to produce, store and release more insulin.(, )
Osteocalcin also acts on muscles and other tissues to help maintain glucose levels in balance. It does this by increasing the production of adiponectin in fat cells (adipocytes). Adiponectin, in turn, increases glucose uptake in fat and muscle cells. ()
Low osteocalcin levels can impair the body's ability to use insulin to manage glucose. ()
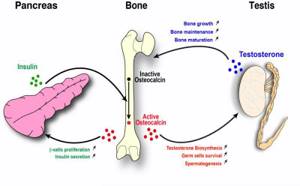
Osteocalcin stimulates testosterone production
Osteocalcin is associated with male reproductive function. When it acts as a hormone in the blood, it interacts with testicular cells through the GPRC6A receptors. This interaction stimulates an increase in testosterone .()
Blood levels of osteocalcin tend to rise during boys' puberty, while low levels are associated with delayed or delayed puberty. However, since osteocalcin levels can vary greatly from person to person, these levels are not necessarily a reliable marker of pubertal development in an individual.()
Osteocalcin improves muscle strength
Osteocalcin has a direct effect on muscle strength, especially in the arms and legs. Signals in muscle tissue received from osteocalcin help muscles adapt to physical activity. Together, these features help osteocalcin prevent the decline in exercise capacity with age.()
Adequate levels of this protein are known to be positively associated with muscle strength in women aged 70 years and older, reducing the risks of falls and fractures. Higher osteocalcin levels are also associated with increased muscle mass and with the prevention of muscle mass loss with age.()
Osteocalcin improves brain function
Osteocalcin helps increase the production of neurotransmitters - dopamine , norepinephrine , serotonin in the brain (experiments were on mice). These neurotransmitters play an important role in motivation, learning and memory.()
One study looked at 44 people with low osteocalcin levels. All of them were diagnosed with negative changes in the microstructure of the brain (in the hypothalamus, thalamus and subcortical white matter). Such changes can lead to decreased brain efficiency.()
Another study of 117 women aged 71-78 years found that cognitive function improved when osteocalcin levels in the brain increased. Other studies in mice showed impairments in learning and memory when osteocalcin levels decreased.
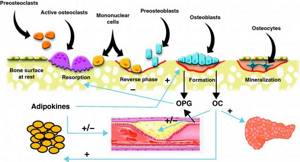
SCHEME OF RELATIONSHIP BETWEEN CELLS OF BONE TISSUE, VASCULAR SYSTEM, FAT TISSUE AND METABOLISM (https://www.elsevier.es/en-revista-endocrinologia-nutricion-english-edition–412-articulo-cardiovascular-disease-bone-metabolism- S2173509311000080)
Osteocalcin
Material for research: blood serum.
Research method: IECHL.
Osteocalcin is a non-collagenous calcium-binding protein that is produced by mature osteoblasts during bone formation.
Preparation for the study: blood is taken on an empty stomach. At least 8 hours (preferably 12 hours) must pass between the last meal and the test. Juice, tea, coffee (especially with sugar) are not allowed. You can drink water.
The synthesis of Osteocalcin requires vitamin K. The protein is localized in the extracellular matrix and plays an important role in the processes of bone mineralization. Osteocalcin is a sensitive marker of bone tissue formation; changes in its concentration in the blood reflect the metabolic activity of osteoblasts.
Osteocalcin is removed from the bloodstream by the kidneys through glomerular filtration and degradation in the renal tubules, therefore, with a pronounced decrease in glomerular filtration (CRF), its level may be overestimated.
There is a close mutual regulation between the processes of bone resorption and bone formation.
High levels of parathyroid hormone, thyroxine, and growth hormone have an inhibitory effect on the activity of osteoblasts producing osteocalcin and reduce its content in bone tissue and blood.
Calcitonin, estrogens and glucocorticoids. stimulate the synthesis of osteocalcin in osteoblasts and increase its level.
BRIGHT-Bio Osteocalcin content in blood serum is normal 2.0 – 22.0 ng/ml
Rickets in young children is accompanied by a decrease in the content of osteocalcin in the blood; the degree of decrease in its concentration depends on the severity of the rickets process and is most pronounced in grade II rickets. The content of osteocalcin in the blood of children with rickets is inversely related to the concentration of parathyroid hormone and directly related to the level of total and ionized calcium and calcitonin.
In patients with hypercortisolism and patients receiving prednisolone, the content of osteocalcin in the blood is significantly reduced, i.e. There is a close relationship between the severity of hypercortisolism and a decrease in bone formation; the process is reflected in a decrease in the content of osteocalcin in the blood. Successful treatment of these categories of patients is accompanied by an increase in the concentration of osteocalcin in the blood.
The level of osteocalcin in patients with hypoparathyroidism is low.
The level of osteocalcin in the blood increases in diseases characterized by increased bone turnover: Paget's disease, primary hyperparathyroidism, renal osteodystrophy, diffuse toxic goiter.
Attention to the Patient
- the concept of norm is not absolute and has no clear boundaries
- Normal reference values often vary significantly among people of different sexes and age groups.
Remember that only your attending physician, who knows your medical history well, can provide a clear interpretation of the test results.
To the attention of the DoctorReference limits for healthy and sick people are often largely the same. You can contact your BRIGHT-Bio consultant for more information. |
See also: β-CrossLaps, Vitamin D total (25-hydroxyvitamin D), Parathyroid hormone
Low osteocalcin levels
Reduced osteocalcin levels are associated with insulin resistance and diabetes
A recent study of 98 healthy people found that low osteocalcin levels led to the body not using insulin effectively (the development of so-called insulin resistance), reducing insulin production and increasing glucose levels. ()
Another meta-analysis of 39 studies involving 23,381 people found that lower osteocalcin levels were associated with higher values of glycated hemoglobin (Hba1c), which indicates average glucose levels over the next 3 months.()
Another study with 128 participants found that increasing osteocalcin levels improved blood glucose levels in type 1 diabetes (an autoimmune disease).()
As it turned out, osteocalcin protects pancreatic beta cells (insulin producers) from damage by high glucose levels (the experiment was carried out on mice). And in an experiment on human beta cells, osteocalcin improved their functioning.()
However, there are other researchers who dispute the existence of a link between osteocalcin and glucose levels. They argue that even if a connection exists, it is not clear whether osteocalcin affects glucose levels or vice versa .()
A similar situation exists with type 2 diabetes. Low levels of osteocalcin in the blood have been shown to be associated with type 2 diabetes in men, women and children. () And daily injections of osteocalcin were able to restore insulin sensitivity and reduce glucose tolerance, as well as protect against the development of obesity and diabetes in mice that were fed a high-fat diet. ()
However, sex differences may also influence how osteocalcin affects insulin resistance. One study showed that long-term use of osteocalcin tablets was able to significantly improve the uptake of glucose into cells, and testosterone levels also increased.()
It appears that larger studies are needed to clarify whether and what kind of association exists between osteocalcin and the risk of developing type 2 diabetes. The difficulty in elucidating these relationships may be due to differences in physiology between mice and humans: for example, mice have three osteocalcin genes, while humans have only one gene. ()
Reduced osteocalcin levels may indicate risk of heart disease
Some studies have found that low osteocalcin levels may indicate possible heart disease. This relationship is not yet clear because there are many other different factors (age, gender, physical activity, etc.). However, research suggests that there is a relationship between osteocalcin and overall heart and vascular health.()
A recent study of 247 older adults with heart disease found a link between low osteocalcin levels and increased risks of developing cardiovascular problems. () Additionally, lower osteocalcin levels were also associated with an increased risk of cardiovascular disease in two studies with 3,384 and 140 participants who had not previously been diagnosed with heart disease.()
Low osteocalcin levels are associated with hardening of the arteries (calcification)
There is a complex relationship between osteocalcin and hardening of the arteries. The meta-analysis identified 26 studies with a positive relationship, 17 studies with a negative relationship, and 29 with a neutral relationship. ()
, higher osteocalcin levels showed reduced hardening (calcification) of the arteries and a reduced risk of heart disease )
Finally, one study of 1,691 men and 1,913 women found that osteocalcin levels and arterial calcification were associated in an “inverse J-curve.” This means that both low and high levels of osteocalcin can increase the risk of hardening of the arteries (calcification), although low levels increase the risk more .()
Low osteocalcin levels are associated with the development of metabolic syndrome
A meta-analysis of 55 studies involving a total of 46,998 people showed that low blood levels of osteocalcin were associated with an increased risk of metabolic syndrome . A similar conclusion was reached in another study involving 798 older men, where low levels of osteocalcin in the blood Osteocalcin level was an indicator of the development of metabolic syndrome.(I)
Additionally, in a study of more than 2,000 people, low levels of osteocalcin were associated with higher levels of C-reactive protein, which led to increased levels of chronic inflammation in patients with metabolic syndrome.()
Finally, when obese female mice were given osteocalcin during pregnancy, their offspring were protected from metabolic disorders caused by their mothers' obesity.()
Low osteocalcin levels indicate obesity
According to a meta-analysis, low blood levels of osteocalcin are associated with high body mass index (BMI) in humans. Many other studies have also supported this link between obesity and low blood osteocalcin in children, adolescents and menopausal women.
A recent study of 132 participants who were either normal weight or obese found that obesity was associated with low levels of osteocalcin in the blood, which could lead to insulin resistance and chronic inflammation.()
Low osteocalcin levels are associated with the development of non-alcoholic fatty liver disease (NAFLD)
Osteocalcin blood tests can help predict the activity of non-alcoholic fatty liver disease (NAFLD). A study of 120 children aged 7 to 13 years (60 diagnosed with NAFLD and 60 healthy) found that low osteocalcin levels in the blood predicted the severity of NAFLD very well.()
Low osteocalcin blood levels are also an indicator of NAFLD in 4 studies involving a total of 8,834 men and women. ()
Animal studies suggest that osteocalcin may reduce the risk of developing NAFLD by activating the nrf2 (master regulator of antioxidant and detoxification enzymes) protein to reduce oxidative stress in the liver.()
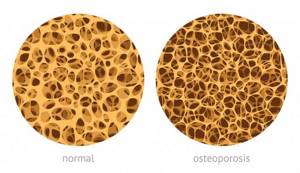
DISCHARGE OF BONE DENSITY IN OSTEOPOROSIS
High osteocalcin levels
Elevated osteocalcin levels may indicate osteoporosis
Elevated blood levels of osteocalcin have been associated with decreased bone mineral density (low bone mass) and osteoporosis . These findings were obtained in 4 studies with a total of 417 postmenopausal women participants. () Tests to determine the level of osteocalcin in the blood can be used to diagnose and monitor the condition of patients with osteoporosis. This can be done with a routine bone mineral density scan.
Other studies have shown that high levels of osteocalcin in the blood are an indicator of bone loss and, in older people, an indicator of decreased bone density and increased risk of fractures . Animal studies suggest that this is due to bone reabsorption (breakdown of bones resulting from the transfer of minerals into the blood), which is accompanied by increased release of osteocalcin into the blood.()
Vitamin K, vitamin D, and calcium supplements lowered blood osteocalcin levels and increased bone density in a study of 78 postmenopausal women.()
High Osteocalcin Levels Linked to Diabetes in Pregnancy
A study of 130 pregnant women indicated a link between high levels of osteocalcin in the blood and the risk of increased insulin resistance during pregnancy, which can lead to the development of a condition called gestational diabetes (a temporary form of diabetes associated with pregnancy and childbirth).()
Osteocalcin blood levels were higher throughout pregnancy in 48 women with gestational diabetes compared to the other 48 healthy pregnant women.()
Elevated osteocalcin levels are associated with breast density in women
Diagnosed obesity in postmenopausal women, together with increased levels of osteocalcin in the blood, showed a greater likelihood of increased breast density. This increase in breast density represents a significant risk factor for the development of breast cancer . This relationship was found in a study of 239 premenopausal and postmenopausal women aged 40-60 years.()
High osteocalcin levels may indicate anemia
Osteocalcin levels can affect the formation of red blood cells, which carry oxygen in the blood. A study of 939 older men aged 72-79 showed high levels of osteocalcin, which was associated with low red blood cell counts. However, the mechanism of this relationship is not yet known.()
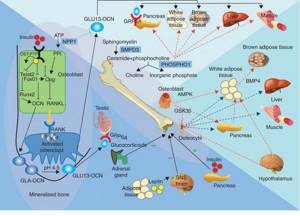
ENDOCRINE ROLE OF OSTEOCALCIN (https://joe.endocrinology-journals.org/content/225/1/R1/F1.expansion.html)
The test will allow your doctor to:
- Diagnose osteoporosis;
- Assess the risk of developing osteoporosis in women during menopause and postmenopause;
- Monitor bone metabolism disorders in women during menopause and postmenopause;
- Identify disorders of bone metabolism in individuals with growth hormone deficiency, hypo- or hyperthyroidism, chronic renal failure;
- To evaluate the effectiveness of antiresorptive therapy.
The study is recommended for:
- Women during pre- and postmenopause;
- Hormone replacement therapy;
- Therapy with gonadotropin-releasing hormone agonists;
- Growth hormone deficiency;
- Hypothyroidism;
- Hyperthyroidism;
- Chronic kidney diseases;
- Hypercalcemic syndrome;
- Treatment with glucocorticoids.
Method:
Enzyme-linked immunosorbent assay (ELISA).
Material for research:
Blood serum.
What increases osteocalcin
Vitamin K
Vitamin K is necessary for the activation of osteocalcin in the body . A lack of vitamin K leads to a lack of osteocalcin in the bones. Vitamin K deficiency is also associated with low bone mineral density and an increased risk of fractures. ()
A placebo-controlled study in 40 healthy young men found that vitamin K supplementation increased osteocalcin levels only after taking it for 4 weeks. This has improved the body's use of insulin (by reducing insulin resistance) and maintaining healthy glucose levels. These results are consistent with other clinical studies of vitamin K supplementation in young men and older women and men. ()
An analysis of blood samples from 896 people found that most people do not get enough vitamin K from their diet, but vitamin K can be obtained as a supplement. The best type of vitamin K to take is vitamin K2, specifically the MK-7 form.()
However, people who take certain types of blood thinning medications (anticoagulants), such as warfarin, should be careful. There is a significant risk that some of these medications will become less effective if vitamin K2 in the form of MK-7 is taken at the same time. Therefore, this combination is not recommended.
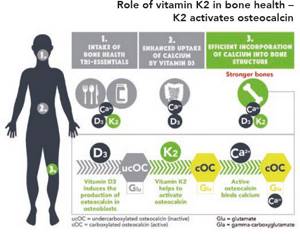
VITAMIN K2 ACTIVATES OSTEOCALCIN
Exercise stress
Osteocalcin levels are higher in people who are more physically active .() An association between physical activity and higher osteocalcin levels was found in a study of 54 adolescents.()
One hour of exercise per day, 3 times per week for 12 weeks, increased osteocalcin levels and increased bone mineral density in 29 women with osteoporosis (age range: 71-78 years).
A study of 11 middle-aged men found that osteocalcin levels increased and remained at that level for several hours after a short period of high-intensity exercise (4 sets of 4 minutes of near-maximal exercise cycling). This same type of training also resulted in an increase in insulin sensitivity .()
There is also evidence that longer periods of less intense exercise may increase osteocalcin levels. A study of 31 middle-aged people found a significant increase in osteocalcin levels after cycling for an hour, 3-4 days a week.()
Another study of 39 obese but otherwise healthy young adults showed that an 8-week exercise program with 4 bouts per week increased blood levels of osteocalcin and leptin.
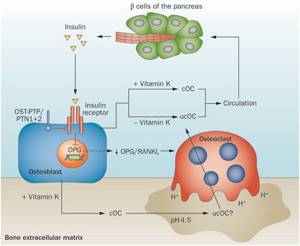
DIAGRAM OF THE RELATIONSHIP OF BONE CELLS OF OSTEOCLASTS AND B-CELLS OF THE PANCREAS WITH THE HELP OF INSULIN AND OSTEOCALCIN
Losing weight and restricting calories
In a study of 107 older adults, osteocalcin increased in the blood with the transition to a calorie-restricted . () In another study of 49 obese men, osteocalcin values increased after weight loss. ()
However, in a weight loss study of 71 postmenopausal women, no association was found between weight loss and changes in osteocalcin levels. Finally, in 178 obese people, increased blood levels of osteocalcin were associated with decreased body fat. However, after losing weight, osteocalcin levels did decrease.()
Vitamin D
Vitamin D directly stimulates the production of osteocalcin .(I) In a study of 76 obese menopausal women aged 51-63 years, vitamin D supplementation combined with a low-calorie diet resulted in increased osteocalcin levels and some improvement in insulin sensitivity.()
Zinc and manganese
Zinc supplementation increased osteocalcin levels in 22 short adolescents. However, these supplements did not change height itself when observed over 6-12 months.()
Manganese supplementation has also been shown to increase blood osteocalcin, bone mineral density, and bone formation in a mouse model.()
Olive oil
A 12-month study of postmenopausal women with reduced bone mass but no diagnosis of osteoporosis found that taking olive leaf extract resulted in increased blood levels of osteocalcin and increased bone density in the spine. ()
Consistent consumption of olive oil as part of the Mediterranean diet increases osteocalcin levels. This conclusion was reached in a study of 42 older men at high risk of heart disease.()
Omega-3 fatty acids
Omega-3 fatty acid supplementation increased osteocalcin levels in rats. But this study requires certain additional evidence from further research.()
Ellagic acid
Ellagic acid is found in many fruits and vegetables, such as pecans, walnuts, pomegranates, raspberries, strawberries and cranberries. This substance works as an antioxidant that prevents cell damage. Ellagic acid promotes an increase in osteocalcin in rats after tooth extraction.()
Milk thistle
The main beneficial substance in milk thistle is silymarin . It promotes the growth of osteocalcin, helps bone healing, and increases bone density in mice with bone fractures.()
Icariin
Icariin is a flavonoid from the Korean Horny Goat Weed plant. A long-term 24-month study suggests that icariin may help prevent bone loss in postmenopausal women. Icariin maintains osteocalcin levels and prevents bone loss.()
Insulin therapy
Type 1 diabetes can cause changes in the skeleton, especially when glucose levels are poorly controlled. Some studies have shown that insulin treatment increases osteocalcin content, which leads to improved bone structure and bone flexibility in people with existing diagnosis of type 1 diabetes.()
Alendronate
Alendronate is a drug used to treat osteoporosis and Paget's disease. Use of alendronate in low doses is associated with increased osteocalcin and improved bone turnover.()
Teriparatide
Teriparatide is a parathyroid hormone used to treat osteoporosis. In a study of elderly women with rheumatoid arthritis, long-term treatment (48 weeks) with teriparatide increased osteocalcin levels in the blood.()
Since people with rheumatoid arthritis have a higher risk of osteoporosis , treatment with teriparatide may be beneficial.()
The information on this site has not been evaluated by any medical organization. We do not seek to diagnose or treat any disease. The information on the site is provided for educational purposes only. You should consult your physician before acting on information from this site, especially if you are pregnant, nursing, taking medications, or have any medical condition.
Rate this article
Average 5 Total votes (7)
Preparing for the study
No special preparation is required for the study.
It is necessary to follow the general requirements for preparation for research. GENERAL RULES FOR PREPARATION FOR RESEARCH:
1. For most studies, it is recommended to donate blood in the morning, from 8 to 11 o’clock, on an empty stomach (at least 8 hours must pass between the last meal and blood collection, you can drink water as usual), on the eve of the study, a light dinner with a restriction eating fatty foods. For tests for infections and emergency studies, it is acceptable to donate blood 4-6 hours after the last meal.
2. ATTENTION! Special preparation rules for a number of tests: strictly on an empty stomach, after a 12-14 hour fast, you should donate blood for gastrin-17, lipid profile (total cholesterol, HDL cholesterol, LDL cholesterol, VLDL cholesterol, triglycerides, lipoprotein (a), apolipo-protene A1, apolipoprotein B); The glucose tolerance test is performed in the morning on an empty stomach after 12-16 hours of fasting.
3. On the eve of the study (within 24 hours), avoid alcohol, intense physical activity, and taking medications (in consultation with your doctor).
4. 1-2 hours before donating blood, refrain from smoking, do not drink juice, tea, coffee, you can drink still water. Avoid physical stress (running, quickly climbing stairs), emotional excitement. It is recommended to rest and calm down 15 minutes before donating blood.
5. You should not donate blood for laboratory testing immediately after physiotherapeutic procedures, instrumental examination, X-ray and ultrasound examinations, massage and other medical procedures.
6. When monitoring laboratory parameters over time, it is recommended to conduct repeated tests under the same conditions - in the same laboratory, donate blood at the same time of day, etc.
7. Blood for research must be donated before starting to take medications or no earlier than 10–14 days after they are discontinued. To assess the control of the effectiveness of treatment with any drugs, a study should be conducted 7-14 days after the last dose of the drug.
If you are taking medications, be sure to notify your doctor.






