Bronchoscopy is a diagnostic and treatment procedure that involves examining and performing certain manipulations in the upper respiratory tract. For these purposes, a special optical device is used - a bronchoscope, which has the form of a flexible tube with a diameter of 3-6 mm, equipped with a special cold lamp, a video camera and a channel for bringing in manipulation instruments.
- Types of bronchoscopy
- Indications for testing
- Contraindications
- Possible complications
- How is bronchoscopy performed?
- Advantages and disadvantages of bronchoscopy
Types of bronchoscopy
Depending on the purpose of the procedure, bronchoscopy can be diagnostic or therapeutic:
- Diagnostic bronchoscopy involves examining the respiratory tract and taking material for further research (biopsy, bronchial lavages). It is prescribed for the diagnosis of malformations of the respiratory system, inflammatory and infectious diseases, detection of neoplasms, and identification of the causes of hemoptysis.
- Therapeutic bronchoscopy, in addition to examining the respiratory tract, involves performing therapeutic manipulations, for example, removing foreign bodies, stopping bleeding, removing sputum, neoplasms and various types of obstructions. In addition, with its help it is possible to target the introduction of drugs into the bronchial tree and sanitize the respiratory tract (removal of viscous sputum, pus, etc.).
Inflate a balloon
Tatyana Shapovalenko proposed this test to Sergei Trofimov, better known as Trofim. Trofim is a heavy smoker with many years of experience, and the doctor had to convince the musician that smoking does not leave its mark on the body. Tatyana Shapovalenko asked Sergei to take a deep breath and try to inflate the balloon with one exhalation
. The resulting ball is the volume of his lungs. With a normal lung capacity of 3.5 liters, Trofim was able to pump only 2.4 liters of air into the balloon. This is very little - and it means that the lungs are no longer working at full capacity. Sergei urgently needs to quit smoking. Try to inflate the balloon too. And know that quitting smoking will change the situation pretty soon.
Indications for testing
Bronchoscopy for diagnostic purposes is prescribed in the following cases:
- Frequent persistent bronchitis and pneumonia, which are difficult to treat.
- Hemoptysis and bleeding.
- Dyspnea of unknown etiology.
- Differential diagnosis of tuberculosis, sarcoidosis, cystic fibrosis, etc.
- Purulent processes - abscess, gangrene of the lungs.
- The presence of foreign bodies in the lumen of the respiratory tract or suspicion of them according to radiography.
- The presence of radiologically detectable neoplasms with endo- or peribrochial/tracheal growth.
- Assess the extent of airway injury in patients with respiratory burns or chest trauma.
When is therapeutic bronchoscopy performed:
- The need to remove viscous secretions or sputum.
- The need for endobronchial administration of therapeutic drugs.
- Stop bleeding.
- Removal of small benign endobronchial or endotracheal neoplasms.
- Removing foreign objects.
- Installation of a stent to ensure patency of the airway when it is strictured or blocked by a tumor.
- Treatment of fistulas.
What about the old people?
There may be some peculiarities here. As the Russian Ministry of Health writes in its recommendations on COVID, “elderly patients may experience an atypical picture of the disease without fever, cough, or shortness of breath. Symptoms of COVID‑19 may be mild and may not be consistent with the severity of the disease or prognosis. Atypical symptoms of COVID‑19 in elderly and senile patients include delirium, falls, functional decline, and conjunctivitis. Delirium, tachycardia, or decreased blood pressure may occur."
Therefore, if a grandmother or grandfather suddenly began to answer questions confusedly, become delirious, fall, or their blood pressure dropped sharply, this is a reason to call an ambulance.
Contraindications
Basically, contraindications to bronchoscopy are associated with the general serious condition of the patient. As a rule, in these cases the procedure is postponed. Absolute contraindications to bronchoscopy are:
- Severe arrhythmia that cannot be corrected.
- Inability to provide adequate oxygenation during bronchoscopy.
- The presence of acute respiratory failure with hypercapnia, except when the patient is on mechanical ventilation (intubated).
- With extreme caution, bronchoscopy is performed in patients with vena cava syndrome, pulmonary hypertension, severe coagulopathies and uremia. Such patients have an increased risk of developing severe bleeding and pneumothorax (collapsed lung), but with the correct technique, the procedure is safe.
Reliable way
A more reliable and reliable way to check lung function, which even doctors recommend, is pulse oximetry. It is also quite possible to do it at home.
“If possible, it is worth purchasing a pulse oximeter - this is a pocket-sized, portable household device. It is placed on the tip of the finger; most often the middle or ring finger is used. You press the button, it turns on, and all you have to do is wait for the numbers to appear steadily on the screen. It shows heart rate and oxygen content SPO2. Normally, a person should have a pulse of 60-90 beats per minute. The oxygen indicator is 94-99% tissue saturation. If less is already one degree or another of respiratory dysfunction, we need to understand this.
Article on the topic
Chief pulmonologist of the Ministry of Health: pneumonia can occur without symptoms It is worth considering that there are no strict indicators of the norm for a person, everyone can deviate in one direction or another. And this will not necessarily be a pathology. As for oximetry, we attach importance when this indicator drops below 90% - this is already some kind of pathology. But even then, you need to measure more than once and draw conclusions, but take several measurements per day. If the indicator is lower all the time, it means the condition is pathological and you need to see a doctor.
At the same time, the person will also have other symptoms - breathing discomfort, fatigue, drowsiness, shortness of breath. In response to this, the pulse will begin to increase. When a person lacks oxygen, the heart begins to work harder, the heart rate increases to more than 90 beats per minute,” notes Doctor of Medical Sciences, Professor of the Russian National Research Medical University named after. N.I. Pirogova, pulmonologist, therapist Alexander Karabinenko .
How is bronchoscopy performed?
Before the procedure, the patient must not eat or drink for at least 6 hours. Premedication is also carried out - sedatives, local anesthetics and, if necessary, anesthesia are administered. The goal of this stage is to minimize the patient’s discomfort during the study, reduce the cough reflex and the secretory function of the bronchi.
Before bronchoscopy begins, the vocal cords and pharyngeal surface are irrigated with an aerosol or inhalational anesthetic, such as lidocaine. The bronchoscope is lubricated and inserted through the nostrils, through the mouth, or through a tracheostomy. Consistently moving along the respiratory tract, the doctor examines the nasopharynx and larynx. During inspiration, the bronchoscope is passed through the vocal cords and then the subglottic larynx, trachea and surface of the bronchi are examined. When reaching the latter, the patient will feel a pronounced urge to cough. There may also be a fear of suffocation, but the patient must be warned that the diameter of the bronchoscope tube is much smaller than the diameter of the bronchi, so there is no risk of asphyxia. In addition, during the procedure, oxygenation (oxygen saturation in the blood), blood pressure, pulse and cardiac activity are monitored.
During the examination, the doctor pays attention to the condition of the mucous membrane of the respiratory tract, its color, the nature of the folds, and the severity of the vascular pattern. Normally, it should have a pale pink color, but a slightly yellowish color is allowed. Its surface is matte with moderately pronounced folds. In large bronchi and trachea, the pattern of blood vessels and the contours of cartilaginous rings are clearly visible. When breathing, the walls of the bronchi and trachea must be mobile.
During inflammatory processes, hyperemic, edematous mucosa will be noticeable on bronchoscopy. The folds will be erased, and mucus or purulent secretion will be found in the lumen of the bronchi. During atrophic processes, on the contrary, folding intensifies, the mucous membrane becomes thinner, and blood vessels become visible through it. The lumens of the bronchi are dilated or gaping.
Also, during bronchoscopy, foreign bodies and endobronchial neoplasms are visualized (they grow inside the lumen of the bronchi). Peribronchial neoplasms can be detected by indirect signs:
- Deformation of the lumen of the bronchus.
- Changes in the mobility of the bronchial wall during respiratory movements.
- Local change in folding.
- Local change in vascular pattern.
In addition, bronchoscopy involves additional diagnostic and therapeutic procedures:
- Brush biopsy - a special brush is inserted through the manipulation channel of the bronchoscope, with the help of which cells are scraped off the surface of suspicious areas.
- Transbronchial biopsy - performed using forceps, which are brought to a suspicious area in the lung parenchyma. To increase diagnostic value and reduce the risk of complications, this procedure is recommended to be performed under X-ray control.
- Washing the lumen of the bronchi. Using a special channel, a sterile saline solution is injected into the lumen of the bronchi through a bronchoscope, which is then aspirated.
- Bronchoalveolar lavage. 50-200 ml of sterile saline solution is injected into the terminal bronchioles. After it fills the distal part of the bronchial tree, the fluid is aspirated and sent to the laboratory for testing for the presence of pathogenic microflora, cells and proteins that can arise from pathology of the alveolar tissue.
- Removal of foreign bodies and small tumors (polyps). This manipulation is carried out using special forceps or a loop. The wound surface is coagulated.
- Stop bleeding. Bronchoscopy can be used to visualize the damaged blood vessel, ligate or coagulate it, and remove blood clots to prevent infection or aspiration.
After all manipulations are completed, the brochnoscope is removed, and the patient remains under the supervision of medical staff for some time. If necessary, additional oxygenation is provided using oxygen therapy. After the pharyngeal reflex is restored and saturation is normalized without oxygen support, the patient can leave the clinic.
How is pulmochek performed?
According to the recommendations of the Russian Respiratory Society (RRO), the European Respiratory Society (ERS) and the American Thoracic Society (ATS), when examining the lungs, it is necessary to pay attention to the patient’s life history, his habits, occupation, living conditions, and childhood.

A separate part is laboratory and instrumental methods. Blood and sputum studies are aimed at assessing the body’s immune defense, tumor markers of lung cancer, main markers of inflammation, and allergies. The spectrum of atypical pathogens of diseases of the lungs and bronchi is also assessed.
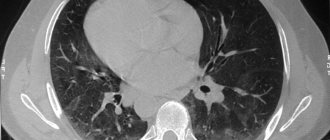
The use of high-resolution CT scans of the lungs allows one to evaluate the picture inside the chest, the location and size of the mediastinal lymph nodes, the thickness and defects of the pleura, the lung tissue and bronchial walls are clearly visible. The pulmonary artery, the main large vessels of the heart and the cavities of the heart are clearly visible. Today, it is chest CT that is recommended by world experts for the early diagnosis of lung cancer. Neither radiography nor chest fluoroscopy, much less fluorography, are such methods.
Functional tests (spirometry) can detect broncho-obstructive syndrome - this is especially important for smoking patients. How to diagnose COPD early.
Spirometry consists of several stages; our doctor asks you to make several forced exhalations into a special sensor - a spirometer. Next, from several attempts, the best indicators are selected and the patient is given inhalation of a bronchodilator drug. This helps differentiate asthma from COPD. The purpose of the study is to assess the ventilation capacity of the lungs and identify bronchial obstruction.
Question: Will it hurt me when examining the lungs and bronchi?
If you are not afraid to take a blood test, then the entire examination is absolutely painless. It’s impossible to say bloodless, because... We still take blood tests.
How many days do you need to stay in the clinic to fully undergo a complete lung diagnosis?
All studies can be completed in 2-3 hours. Laboratory results are usually available in 1-2 days. Thus, within 1-3 days we can give an opinion on the health of your respiratory system.
In conclusion, I would like to say why it makes sense to choose our pulmonology center to conduct this examination
Our doctors have extensive clinical experience in treating and diagnosing various diseases. Many of us are leading specialists in certain areas of pulmonology. The equipment we use is modern and most importantly, we know how to use it. In complex cases, with clinical findings, we can always approach the resolution of your problem by convening a council of specialists. Ultimately, we will definitely figure out the identified problem or confidently state that your lungs are healthy.
Advantages and disadvantages of bronchoscopy
Bronchoscopy is an important diagnostic and therapeutic procedure, with which you can obtain information that is crucial for making a diagnosis and determining further treatment tactics. There are no analogues to it today. However, bronchoscopy comes with certain risks, which we discussed above. According to statistics, very rarely (1/10,000 studies) severe complications leading to death can occur (usually in severe patients).
Clear selection of patients, taking into account indications and contraindications for bronchoscopy, as well as strict adherence to the procedure technique, helps to minimize such risks. The risks are also reduced when the examination is carried out by an experienced doctor. In our clinic, bronchoscopy is performed by Mikhail Sergeevich Burdyukov, Doctor of Medical Sciences, expert physician.
Book a consultation 24 hours a day
+7+7+78
About control CT scans
Objectively, for outpatients in our region, CT is now a dream, as the doctors themselves admit. The capacity of computed tomography scanners is overloaded with inpatients and primary patients.
According to the recommendations of the Russian Ministry of Health, the frequency of CT scans depends on the clinical indications that dictate the need to assess the dynamics of pneumonia. At the same time, an objective assessment of dynamics is possible only by comparing data from one type of study.
That is, if the patient was given a CT scan at the very beginning, then CT scan should be used for control later on - unless, of course, by that time the person is no longer in intensive care in a non-transportable state. For example, CT or RG.
Raids on passengers without masks have been resumed in Yekaterinburg
Who is the examination indicated for?
A low-dose CT scan of the chest is required:
- adults aged 55 to 80 years with a smoking history of 30 packs/years;
- smokers over 50 years of age with a smoking history of 20 packs/years;
— people who have professional contact with asbestos, chromium, arsenic or coal;
- those who have a hereditary predisposition to the tumor;
- people with chronic obstructive pulmonary diseases.
The smoking index (SI) is the number of cigarettes smoked per day, multiplied by the smoking experience in years and divided by 20 (the number of cigarettes in a pack). For example, 10 years of experience with 20 cigarettes (1 pack) per day = IR = 20X10/20 = 200/20 = 10. IR more than 10 packs\years is a reliable risk factor. CT Smokers over 50 years old are recommended to undergo a study every two years .
Breath-hold test
Tatyana Shapovalenko proposed this test to Alexander Polovtsev, the hero of the television series “Streets of Broken Lights” and a smoker with thirty years of experience. You need to hold your breath
and try to hold out for as long as possible. And to check whether you are breathing through your nose unnoticed, ask someone to hold a mirror or glass plate to your face. If it fogs up, it means the body is cheating. A healthy person can hold their breath for at least a minute. Alexander managed to do this for only 23 seconds. Therefore, he had to carry out a long and difficult struggle with himself to quit smoking. But after eight weeks, the artist was able to hold his breath for as much as 67 seconds. This means his lungs have begun to recover.