The method of examining the respiratory tract and respiratory organs endoscopically is called bronchoscopy. The essence of the method is to insert a flexible hose with a camera at the end into the trachea and then into the bronchi. The image from the camera is transmitted to the screen, thanks to which diagnosticians can identify problem areas, locations of tumors and other pathologies. In terms of making a correct diagnosis, pulmonary bronchoscopy cannot be replaced by MRI, CT, radiography and other studies.
This technique for detecting respiratory diseases is not used for common colds or bronchitis. It is necessary in cases where the patient’s inflammation lasts for several weeks or months and cannot be corrected with medication. In the first Danilovsky multidisciplinary medical center on Avtozavodskaya, bronchoscopy is performed by real professionals using high-quality equipment. No pain or harm for patients during the procedure!
FREE WITH ANNUAL MEMBER
What is bronchoscopy
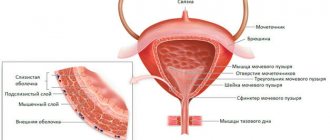
Bronchoscopy is an endoscopic method for examining the respiratory tract: larynx, trachea and bronchi in order to identify diseases of the mucous membranes of these organs.
The procedure is carried out using a bronchoscope - a flexible or rigid tube with a diameter of 3-6 mm, equipped with a lighting lamp and a photo-video camera. Modern devices are based on fiber optic technology, which ensures high diagnostic efficiency. The image is displayed on a computer monitor, so it can be enlarged tens of times and the recording can be saved for subsequent dynamic observation. The optical system of the device allows you to examine the respiratory tract up to the second branch of the bronchi and in 97 percent of cases make an accurate diagnosis. Bronchoscopy is used in the diagnosis of chronic bronchitis, recurrent pneumonia, and lung cancer. If necessary, tissue samples can be taken for biopsy during bronchoscopy. The technique of bronchoscopy provides the possibility of using the procedure for medicinal purposes - for:
- removal of foreign bodies from the bronchi;
- cleansing the trachea and bronchi from pus and mucus;
- washing and administration of medicinal solutions (antibiotics, glucocorticoids, mucolytics, nitrofurans);
- expansion of the narrowed lumen of the bronchi;
- removal of small tumors.
To treat respiratory diseases and take material for histological examination, the bronchoscope is equipped with the necessary surgical instruments.
If necessary, two studies are performed together - bronchoscopy and bronchography. Bronchography is an x-ray method in which a contrast agent is injected into the airways through a catheter or fiberoptic bronchoscope. The study allows us to study in detail the structure of the bronchial tree (especially those parts of it that are inaccessible for endoscopic examination) and evaluate its motor function during breathing.
Diagnostic and therapeutic capabilities of modern bronchoscopy
Today, more than a hundred years after the “father of bronchoscopy” Gustav Killian first inserted an endoscope into the trachea and removed an aspirated meat bone from a patient, bronchoscopy is one of the leading methods for diagnosing and treating respiratory diseases. Most lung diseases are in one way or another associated with bronchial pathology. The airways provide access to any areas of the lung, allow one or another instrument to be passed to them and obtain a variety of information about the state of the respiratory organs, and also represent an additional route for administering medications to pathologically altered areas of the lung.
History of development
The development of bronchoscopy can be divided into three stages. At the first, which began at the end of the 19th century. and continued until the end of the 50s of the twentieth century, bronchoscopy was performed under local anesthesia, usually using rigid bronchoesophagoscopes
, which had a dual purpose - examination of the tracheobronchial tree and esophagus. The progress of bronchoscopy during this period was greatly facilitated by the work of Ch. Jackson, J. Lemoine, A. Soulas, A. Olsen, N. Andersen, and in our country - A. Delens, V. Voyachek, V. Trutnev, A. Likhachev and Chalky. Bronchoscopy during this period was performed mainly for foreign bodies in the respiratory tract and was carried out mainly by otolaryngologists. The procedure was very traumatic, and the patients had a hard time bearing it.
With the advent and improvement of general anesthesia, pulmonary surgery began to actively develop and indications for bronchoscopy expanded significantly. This was facilitated by the creation in the late 50s - early 60s of respiratory bronchoscopes (N. Friedel; R. Hollinger; G.I. Lukomsky), which made it possible to perform bronchoscopy under anesthesia with myoplegia and injection ventilation of the lungs, which significantly alleviated the suffering of patients and made the study safer. The progress of bronchoscopy at this second stage of its development was facilitated by the appearance of lens telescopes with direct, lateral and retrograde optics, various instruments for biopsy, extractors, scissors, and electrocoagulators. At this stage, bronchoscopy passed into the hands of thoracic surgeons.
A true revolution in bronchology and the beginning of the third, modern stage in the development of bronchoscopy was the creation in 1968 of a flexible bronchofiberscope
[1], with the help of which it became possible to examine the lobar, segmental and subsegmental bronchi of all parts of the lung, perform a visually controlled biopsy, and administer medicinal solutions. The fiberoptic bronchoscope has significantly changed the technique of bronchoscopy. It was again performed under local anesthesia, causing almost no discomfort to the patients. Bronchofibroscopy began to be successfully performed on an outpatient basis, in pulmonology hospitals and offices, and in intensive care units. It seemed that the need for rigid bronchoscopes had disappeared forever. However, the creation of high-energy medical lasers determined a new direction in bronchology - surgical endoscopy, and rigid endoscopes were again required for it. Therefore, modern bronchoscopy is equipped with both flexible and rigid endoscopes and instruments that allow performing a wide range of diagnostic and therapeutic manipulations in the trachea and bronchi both under local anesthesia and under general anesthesia.
Indications for bronchoscopy
The main indications for bronchoscopy are shown in Table. 1. They should be divided into diagnostic and therapeutic.
Diagnostic bronchoscopy
Tumors of the bronchi and lungs
Tumors of the bronchi and lungs
Tumors of the bronchi and lungs are one of the main indications for bronchoscopic examination. Currently, verification of centrally located endobronchial cancer reaches almost 100% and is carried out by visually controlled biopsy with wire cutters. Diagnosis of the so-called “early cancer”, which also includes tumors in situ, is more difficult. Fluorescent chromobronchoscopy helps to identify such neoplasms, almost invisible to the naked eye.
with the introduction of special drugs - photosensitizers [2, 3].
Diagnosis of peripherally located tumors, especially small ones, can also be quite difficult, since getting to such tumors through the bronchi is very difficult.
Their biopsy is performed under the control of an X-ray television screen and, in addition to cutters, scarifying brushes and controlled curettes are used. However, even in experienced hands, verification of peripheral lung tumors rarely reaches 60-70% and in complex cases should be combined with percutaneous puncture biopsy under computed tomography (CT) control.
Diagnosis of peribronchial cancer also requires great skill, especially in the early stages. The presence of such a tumor can be suspected based on X-ray and CT data, and to verify it, a puncture biopsy
the bronchial wall in a suspicious place using a special needle. Thus, all darkening or cavitary formations in the lungs, hilar or located on the periphery, suspicious for the oncological process, are direct indications for bronchoscopy and various methods of bronchoscopic biopsy, the choice of which is determined by the doctor performing the study.
Mediastinal neoplasms and lymphadenopathy
Mediastinal neoplasms and lymphadenopathy may also be indications for bronchoscopy. With enlarged paratracheal and bifurcation lymph nodes and mediastinal tumors located in close proximity to the trachea, material for cytological examination can be obtained using transtracheal puncture biopsy
. However, the not very reliable results of such a study have now ceased to meet the requirements of practice and bronchoscopic methods have been replaced by more invasive, but much more informative methods: mediastinoscopy, pleuromediastinoscopy [4, 5] and video thoracoscopy [6]. They should be resorted to in cases where bronchoscopic biopsy methods are ineffective.
Diffuse lung diseases
The same trend can, to a certain extent, be attributed to the diagnosis of diseases accompanied by diffuse changes in the pulmonary pattern (the so-called diffuse lung diseases - DLD), which require morphological research for their verification. Since the early 70s, after the work of N. Andersen, transbronchial pulmonary biopsy
, performed using a bronchoscope, has become the leading method for diagnosing DLD [5]. Over time, however, it became clear that with transbronchial lung biopsy it is not always possible to obtain enough lung tissue to successfully carry out differential diagnosis in a number of DLD, especially those accompanied by fibrosing processes in the pulmonary parenchyma. And although the relatively less invasiveness still allows transbronchial lung biopsy to remain the method of primary endoscopic diagnosis of DLD, it is increasingly complemented by thoracoscopic biopsy, performed using wire cutters or endostapplers, hermetically stitching the lung parenchyma while simultaneously cutting off a section of lung tissue of the required size [6].
Important diagnostic information for many lung diseases, and primarily for DLD, can be obtained by studying material obtained using bronchoalveolar lavage (BAL)
.
The latter today is an almost obligatory study in the diagnosis and treatment of DLD such as cryptogenic fibrosing alveolitis and sarcoidosis. BAL performed repeatedly during the treatment of these diseases makes it possible to monitor the effectiveness of therapy and determine its prognosis. Bronchoscopy and BAL are also indicated for suspected fungal diseases of the bronchi
(bronchomycosis) and some
parasitic diseases of the lungs
(for example, with Pneumocystis pneumonia).
Inflammatory processes in the lungs
A bronchoscope allows you to look deeply into the airways. This makes it possible for patients with descending tracheobronchitis to determine the distal border of the lesion of the bronchial tree and the intensity of inflammation in it. Bronchoscopy is effective in searching for a draining bronchus in acute lung abscesses, as well as in the differential diagnosis of bacterial suppuration and disintegrating cancer in the presence of a cavity in the lung. The difficulties of absolute sterilization of bronchofibroscopes somewhat complicate the microbiological diagnosis of inflammation and require the use of special catheters that protect the material collected in the bronchi from contamination with the contents of the oral and nasal cavities. Our experience in the use of bronchoscopy in patients with acute and chronic inflammatory lung diseases allows us to give preference to the use of a rigid bronchoscope, amenable to thermal sterilization methods, if microbiological diagnosis of pulmonary suppuration is necessary.
Pulmonary hemorrhage and hemoptysis
If we strictly follow the terminological logic, hemoptysis is a manifestation, a symptom of pulmonary hemorrhage. However, in practice, pulmonary hemorrhage (or hemoptoea) refers to the release of pure blood or intensely bloody sputum when coughing, and hemoptysis (hemophthisis) refers to the coughing up of sputum tinted with blood or containing streaks of blood. Thus, there is a quantitative difference between hemoptoea and hemophthisis [4, 5]. Both pulmonary hemorrhage and hemoptysis are direct indications for diagnostic bronchoscopy, since this is the only way to determine the source of bleeding or at least its approximate location.
The causes of pulmonary hemorrhage and hemoptysis are extremely diverse. In addition to the pathology of the tracheobronchial tree and lung parenchyma, among them are diseases of the blood and circulatory system, hemorrhagic diathesis and capillary toxicosis, pulmonary embolism, pulmonary endometriosis, etc. The relative frequency of these causes has changed over time. Thus, in the 30s and 40s, destructive pulmonary tuberculosis was in first place among all causes of pulmonary hemorrhage. Currently, the most common cause of hemoptysis in the pulmonology clinic is chronic bronchitis accompanying bronchiectasis or focal pneumosclerosis, in which in foci of chronic inflammation against the background of decreased blood flow along the branches of the pulmonary artery, excessive vascularization develops due to dilation of the bronchial arteries and multiple anastomoses arise between the large and small circles of blood circulation.
Due to the shunting of blood from the bronchial arteries into the branches of the pulmonary artery, hypertension occurs in the microvasculature of the lungs, which the fragile walls of small vessels cannot withstand, and the blood enters the respiratory tract. Similar mechanisms are observed in the area of foci of destruction of lung tissue of specific and nonspecific etiology. During bronchoscopy in these cases, the source of bleeding, as a rule, cannot be seen, but it is quite possible to determine at least its approximate location, especially if the study is performed at the height of hemoptysis. This is very important for determining treatment tactics for each individual patient.
The causes of hemophthisis and hemoptoea diagnosed in patients in the thoracic surgical department are presented in Table. 2. Undoubtedly, the most serious cause of pulmonary hemorrhage and hemoptysis was and is bronchial tumors and, above all, cancer, which can only be verified using bronchoscopy. This allows us to conclude that in all cases of pulmonary hemorrhage and hemoptysis, bronchoscopy is a mandatory study, the main purpose of which is to identify or exclude a malignant neoplasm of the lungs
.
Chronic cough
Among the indications for diagnostic bronchoscopy, the so-called treatment-resistant cough should also be mentioned, i.e. cough that does not respond to intensive treatment for at least 1 month, the cause of which remains unclear. And although lung tumors, according to R. Irwin et al. [7], are rarely accompanied by an isolated cough syndrome (without any radiological manifestations), our experience in examining persistently coughing patients [4, 5] gives us reason to assert that bronchoscopy is one of the most important studies in the complex diagnosis of the causes of chronic cough.
Broncho-obstructive syndrome
Bronchoscopy plays an important role in the differential diagnosis of chronic obstructive pulmonary diseases and obstruction of the trachea and bronchi, accompanied by broncho-obstructive (asthmoid) syndrome. This primarily applies to tumors, foreign bodies (including those of endogenous origin - broncholitis) and cicatricial strictures of the trachea and large bronchi, in which radiological symptoms may be completely absent, and the clinical picture is very similar to an attack of bronchial asthma [8, 9].
Therefore, in cases where patients have signs of difficulty breathing that are not relieved by modern drug therapy, a bronchoscopic examination is indicated, which often reveals one or another organic pathology in the large respiratory tract.
Therapeutic bronchoscopy
Removal of aspirated foreign bodies
Removal of aspirated foreign bodies
The therapeutic capabilities of bronchoscopy have long been limited to the extraction of aspirated foreign bodies, and even now this is the only bloodless method of removing them from the bronchi.
The development of flexible extractors and the considerable experience accumulated to date suggests that most aspirated foreign bodies in adults can be removed using a bronchofiberscope under local anesthesia and even on an outpatient basis [5]. However, foreign bodies in the respiratory tract sometimes present the bronchologist with the most unpleasant surprises, forcing the use of general anesthesia and hard instruments and requiring maximum concentration of strength and skill, and sometimes inspiration.
Drainage of intrapulmonary purulent foci
The therapeutic effect of bronchoscopy as a method of draining intrapulmonary purulent foci, be it bronchiectasis or lung abscesses, is undeniable. Therapeutic catheterization of the bronchi during bronchoscopy makes it possible to unblock a significant part of the intrapulmonary abscess cavities [5], and long-term transnasal drainage [10] ensures the constant introduction of antibacterial drugs into the cavity and frees patients from repeated bronchoscopy and catheterization. A technique for immunoreplacement therapy has been developed in the form of intracavitary administration of a suspension of autologous macrophages [11], making bronchoscopic treatment even more effective.
Chronic obstructive bronchitis
The therapeutic role of bronchoscopy in chronic obstructive bronchitis (COB) has traditionally been limited to restoring airway patency with stimulation or imitation of impaired bronchial drainage function and local use of antibacterial and secretolytic agents. After the first publications by A. Soulas and P. Mounier-Kuhn, who described the method of treating patients with chronic nonspecific lung diseases using a bronchoscope, many different methods of bronchoscopic treatment of COB were proposed. Some of them were abandoned as having not been tested by practice, others took a strong place in the arsenal of therapeutic agents for patients with diseases of the bronchopulmonary system [5, 12].
Currently, sanitation bronchofibroscopies
, carried out under local anesthesia in a course method with a frequency of 1 time every 2-3 days.
The duration of the course depends on the severity of the pathological process and the effectiveness of treatment and ranges from 3 to 20 sessions. If the sputum is purulent and there is a significant amount of it, 10 ml of a 0.5-1% solution of potassium furagin, warmed to body temperature, is instilled through the channel of the bronchofibroscope into the bronchi with the addition of 1-2 ml of a mucolytic ( ambroxol, acetylcysteine
).
Before removing the bronchofibroscope, antibiotics are injected into the lumen of the bronchi in a daily dose (in accordance with the sensitivity of the bronchial microflora to them). In the presence of purulent sputum with an ichorous odor, instillation of a 1% dioxidine solution in an amount of 5-10 ml is used. At the end of the procedure, the patient is placed alternately on each side for 5-7 minutes, after which he is asked to actively cough.
The emergence of new technical devices is also reflected in the endobronchial therapy of inflammatory lung diseases. The publications of E. Klimanskaya, S. Ovcharenko, V. Sosyura and others describe the use of low-frequency ultrasound and radiation from ultraviolet and helium-neon lasers
during therapeutic bronchoscopy in patients with chronic bronchitis and pulmonary suppuration, including children. The authors have obtained good results from the use of these methods, which, in their opinion, contribute to better sputum production, increased concentration of antibiotics in the bronchi and improved local immune defense of the respiratory tract.
NOT. Chernekhovskaya and I.V. Yaremaya [13] obtained a positive effect from the intrabronchial use of the immunomodulator T-activin, which, according to the authors, contributes to the restoration of the immune reactivity of the bronchial mucosa. In patients with COB, the drug was injected during bronchoscopy using a needle into the mucous membrane of the spurs of the lobar and segmental bronchi in the places of the most visually pronounced inflammation. For severe inflammation in the bronchi, the authors recommended the use of intrabronchial immunotherapy in combination with endolymphatic administration of antibiotics into interbronchial spurs.
In conclusion, we consider it our duty to remind you that sanitary bronchoscopy is a rather crude and traumatic method of treatment and should be performed in patients with COB if there are appropriate indications, which primarily include purulent complications and a pronounced obstructive component of the disease. It is not necessary to expand the indications for therapeutic bronchoscopy in patients with serous forms of endobronchitis without severe bronchial obstruction, where it is quite possible to achieve good results using inhalation, injection or oral methods of administering therapeutic drugs. Bronchoscopy is a “cannon” method of treatment and is hardly worth using when “shooting at sparrows.”
Severe bronchial asthma
If there is a significant accumulation of thick, viscous sputum in the distal parts of the bronchi in cases of ineffective expectoration, which is often observed in severe bronchial asthma, therapeutic bronchial lavage
. For the first time, massive lavage of the bronchi through an endotracheal tube was described by H. Thompson and W. Pryor in patients with alveolar proteinosis and bronchial asthma. By modifying this method, we developed a technique for therapeutic bronchial lavage through a rigid bronchoscope under conditions of pulmonary injection ventilation [5, 12]. Therapeutic bronchial lavage in patients with severe respiratory failure requires highly qualified anesthesiological care and post-anesthesia monitoring in an intensive care unit or intensive care unit. When performed correctly, this procedure effectively helps remove sputum from medium- and small-caliber bronchi that are inaccessible to other methods of endobronchial aspiration. It is important to point out the dangers of using this technique in patients with purulent forms of endobronchitis, since the absorption of liquefied and not completely removed purulent sputum can lead to increased intoxication and worsening of the patients’ condition.
In several particularly severe patients with status asthmaticus and hypoxic coma, we performed bronchial lavage under conditions of extraorgan oxygenation. The experience of using such a resuscitation aid is relatively small, but it deserves attention and can be used in specialized intensive care units.
Early postoperative period
Bronchofibroscopy has proven itself to be an effective treatment procedure for impaired bronchial obstruction in patients in the early postoperative period and, especially, in patients requiring long-term artificial pulmonary ventilation (ALV). A flexible bronchofiberscope can be easily inserted into the patient’s respiratory tract through an endotracheal or tracheostomy tube, which makes it possible to perform sanitary bronchoscopy in patients on mechanical ventilation daily, and, if necessary, several times a day [5].
In addition to the fairly ordinary situations listed above that require the use of bronchoscopy, there are a number of more rarely occurring pathological conditions in which bronchoscopy can also have therapeutic value. These include isolated cases of destructive pneumonia complicated by pyopneumothorax
. In some patients with this disease, wide or multiple bronchopleural fistulas not only do not allow the lung to expand after drainage of the pleural cavity, but also do not allow successful sanitization of the pleural cavity due to the penetration of lavage fluid into the respiratory tract. In such a situation, it is possible to insert an obturator made of foam rubber or collagen sponge through a bronchoscope into the corresponding segmental or lobar bronchus and temporarily block it [5]. This seals the lung and stops the drainage of air. This creates conditions for effective lavage of the pleural cavity and reexpansion of the lung. Such a blockade of the bronchi is possible for a period of several days to 2 weeks. During this time, the pleural moorings manage to fix the lung in an expanded state, and small fistulas can close. Temporary bronchial occlusion is also successfully used for large solitary lung abscesses, helping to reduce and obliterate their cavity [14].
In patients with severe dystonia of the membranous wall of the trachea
, manifested by the clinical picture of expiratory stenosis,
transtracheal sclerotherapy
performed during bronchoscopy can help reduce its symptoms. According to the method proposed by A.T. Alimov and M.I. Perelman [15], using a flexible bronchoscopic needle-injector, a mixture of glucose and blood plasma is injected into the tissue between the walls of the esophagus and trachea through the membranous wall of the latter, which causes the development of retrotracheal sclerosis and fixes the excessively mobile tracheal membrane. In patients, the difficulties of exhalation and expectoration are reduced and the annoying and ineffective cough that torments them is alleviated.
Endotracheal and endobronchial surgical interventions
A description of the therapeutic capabilities of bronchoscopy will be incomplete without mentioning endotracheal and endobronchial surgical interventions. At first, they were performed using high-frequency current, but recently high-energy YAG lasers—neodymium and holmium—have been predominantly used. benign tumors of the trachea and large bronchi are successfully removed during bronchoscopy
, perform recanalization of the trachea with its
tumor, granulation and cicatricial stenoses
[16, 17]. The latter occur quite often, complicating prolonged tracheal intubation or tracheostomy in patients in intensive care units. To prevent re-stenosis of the trachea after its recanalization with a laser, for peribronchial tumors compressing the lumen of the trachea or main bronchi, as well as for collapse of the tracheal walls as a result of tracheomalacia, silicone stents of various designs are used - self-fixing with the help of protrusions, T-shaped or Y-shaped , bifurcation [17].
Such spacer stents can remain in the lumen of the trachea and main bronchi for a long time and provide free patency of large airways, in some cases making it possible to do without tracheostomy.
Contraindications to bronchoscopy
Contraindications to bronchoscopy are usually relative.
These include severe respiratory failure, cardiac arrhythmias, a tendency to bronchospasm, blood clotting disorders, and severe intoxication. In these cases, we are talking mainly about diagnostic studies. Where bronchoscopy is performed for therapeutic purposes, these contraindications often fade into the background and, according to vital indications, bronchoscopy can be justified in the most severe patients, being part of the resuscitation manual.
Complications of bronchoscopy
With the increase in the number and invasiveness of bronchoscopic techniques and the expansion of indications for them, the risk of the procedure has also increased, which, despite the increased level of anesthesia, is still occasionally accompanied by quite serious complications (Table 3).
Their prevention and treatment constitute a separate and very extensive problem that cannot be covered within the limited scope of this review. Our analysis of complications of bronchofibroscopy and the so-called rigid or rigid bronchoscopy in homogeneous groups of patients [5] showed that “flexible” bronchoscopy, performed for diagnostic purposes, is generally accompanied by a significantly smaller number of severe complications, in particular those caused by diagnostic manipulations, because it is associated with less trauma to the bronchi and biopsy objects. This allows us to speak about the comparatively greater safety of diagnostic bronchofibroscopy under local anesthesia, which is especially important in outpatient practice. It is impossible to compare the safety of therapeutic bronchoscopic procedures performed using rigid and flexible endoscopes, since the indications for their use, and therefore the severity of the patients’ condition, differ significantly. It should only be emphasized that bronchofibroscopy, as well as “rigid” bronchoscopy, cannot be considered an absolutely safe method of research and treatment. This procedure requires the endoscopist to not only perform it in different ways and understand endobronchial and pulmonary pathology, but also to be prepared for the development of various, sometimes severe complications, and requires certain knowledge and skills of a resuscitation, therapeutic and surgical nature. The room in which bronchoscopy is performed, whether it is a special room or an intensive care ward, must be appropriately equipped and equipped with all the devices for successful resuscitation or immediate treatment of any complication that is potentially possible during the introduction of a bronchoscope and endobronchial manipulation with its help. Literature
1. Ikeda Sh. Flexible Bronchofiberscope. Ann.Otol., 1970; 79 (5): 916–23.
2. Chissov V.I., Sokolov V.V., Filonenko E.V. and others. Modern possibilities and prospects of endoscopic surgery and photodynamic therapy of malignant tumors. Ross. oncological magazine 1998; 4: 4-12.
3. Lam S., MacAulay C., Palcic B. Detection and Localization of Early Lung. Cancer by Imaging Techniques. Chest, 1993; 103: 1 (Suppl.): 12S—14S.
4. Lukomsky G.I., Shulutko M.L., Winner M.G., Ovchinnikov A.A. Bronchopulmonology. M., Medicine. 1982; 399.
5. Lukomsky G.I., Ovchinnikov A.A. Endoscopy in pulmonology. In the book: Guide to clinical endoscopy. Ed. V.S. Savelyev, V.M. Buyanov and G.I. Lukomsky. M., Medicine. 1985; 348-468.
6. Porkhanov V.A. Thoracoscopic and video-controlled surgery of the lungs, pleura and mediastinum. Abstract of dissertation. Doctor of Medical Sciences M., 1996; 33.
7. Irwin R., Rosen M., Braman S. Cough: A comprehensive review. Arch.Intern.Med., 1977; 137 (9): 1186–91.
8. Danilyak I.G. Bronchoobstructive syndrome. M. Newdiamed. 1996; 34.
9. Perelman M.I., Koroleva N.S. Asthmatic syndrome in diseases of the trachea. Ter. archive 1978; 3:31-5.
10. Ovchinnikov A.A., Filippov M.V., Gerasimova V.D. and others. The use of long-term transnasal catheterization in the treatment of patients with lung abscesses. Gr.hir. 1986; 4:45-9.
11. Chuchalin A.G., Ovchinnikov A.A., Belevsky A.S. et al. The use of a suspension of autologous macrophages in the treatment of lung abscesses. Klin.med. 1985; 2: 85-8.
12. Ovchinnikov A.A. Endoscopic diagnosis and therapy of chronic obstructive bronchitis. In the book: Chronic obstructive pulmonary diseases. Ed. A.G. Chuchalina. Publishing house BINOM, 1998; 423-35.
13. Chernekhovskaya N.E., Yarema I.V. Chronic obstructive pulmonary diseases. M. RMAPO, 1998; 148.
14. Ivanova T.B. Prolonged temporary bronchial occlusion in the complex treatment of acute suppurative diseases of the lungs and pleura. Author's abstract. diss. ...candidate of medical sciences. M., 1987. 22.
15. Alimov A.T., Perelman M.I. Sclerosing endoscopic therapy for expiratory stenosis of the trachea and main bronchi. Gr.hir. 1989; 1:40-3.
16. Rusakov M.A. Endoscopic surgery of tumors and cicatricial stenoses of the trachea and bronchi. M., Russian Research Center of Chemistry, Russian Academy of Medical Sciences. 1999; 92.
17. Dumon J., Meric B. Handbook of endobronchial YAG laser surgery. Hopital Salvator, Marseille, France. 1983; 97.
| Applications to the article |
| All dark spots or cavitary formations in the lungs suspicious for an oncological process are direct indications for bronchoscopy with biopsy |
| The most common cause of hemoptysis in the pulmonology clinic is chronic bronchitis |
| Sanitation bronchoscopy is a rather traumatic method of treatment and in patients with COB should be performed according to indications |
Types of bronchoscopy
Depending on the purposes of the study, two types of procedures are used:
- Flexible bronchoscopy - it is performed using flexible tubes (fiber bronchoscope). Thanks to its small diameter, the fiber bronchoscope can move into the lower sections of the bronchi, practically without injuring their membrane. Flexible bronchoscopy is used to diagnose diseases of the respiratory tract, including its lower sections. High-quality visualization of mucous membranes allows not only to diagnose pathologies, but also to remove small foreign bodies. This type of research can be used in pediatrics. General anesthesia is not required for flexible bronchoscopy.
- Rigid bronchoscopy – for its implementation, a device with a system of rigid hollow tubes is used. Their diameter does not allow examining small bronchi, unlike the fibrobrochosop. A rigid bronchoscope has a wider range of therapeutic capabilities and is used for:
- fight bleeding
- expansion of the lumen of the bronchi,
- removal of large foreign objects from the respiratory tract,
- removing mucus and fluid from the lungs,
- lavage of the bronchi and administration of drug solutions,
- removal of tumors and scars.
General anesthesia during rigid bronchoscopy is performed, so the patient does not feel any discomfort.
Possible complications
Virtual bronchoscopy is an x-ray method of examination. However, modern tomographs expose the patient to minimal radiation, so such computer scanning is safe for humans.
Why can our articles be trusted?
We make health information clear, accessible and relevant.
- All articles are checked by practicing doctors.
- We take scientific literature and the latest research as a basis.
- We publish detailed articles that answer all questions.
At the same time, pregnant women should refrain from this type of diagnosis of the bronchi and lungs, since even the lowest dose of radiation can negatively affect the fetus.
This study method does not use a contrast agent, which sometimes causes allergic or adverse reactions, and this also increases the safety of virtual bronchoscopy.
Indications for bronchoscopy
Bronchoscopy is used for diagnostic purposes in the presence of:
- unmotivated painful cough;
- shortness of breath of unknown origin;
- hemoptysis;
- frequent bronchitis and pneumonia;
- suspicion of a foreign body in the bronchi or tumor;
- cystic fibrosis and tuberculosis;
- bleeding from the respiratory tract.
For therapeutic purposes, bronchoscopy is performed in the following cases:
- entry of a foreign body into the trachea or bronchi;
- coma and other states of respiratory failure;
- bleeding - to stop it;
- the presence of viscous sputum, pus or blood;
- a tumor that has blocked one of the bronchi;
- the need to administer antibiotics and other drugs directly into the respiratory tract.
Bronchoscopy for pneumonia can be prescribed for both diagnostic and therapeutic purposes.
Decoding the results
Scanning allows you to obtain clear images of tissue sections in various planes. While assessing the resulting image, the specialist examines the density of the lungs, examines the tissue structures for the presence of sarcoma granulomas, which, in the acute form of the pathology, turn into a vitreous body and impair the ventilation of the organ.
The area affected by the cancer does not function during breathing, so deterioration in blood circulation is detected in this area.
The patient receives a conclusion with the examination data within 40 minutes after the manipulation, after the images have been analyzed by a radiologist. After this, the patient must consult a doctor who has issued a referral for virtual bronchoscopy.
If there is a suspicion of a serious disease (tuberculosis or cancer), then auxiliary research methods are prescribed. However, in most cases, a CT scan of the bronchi is sufficient to make an accurate diagnosis and select effective therapy.
Virtual bronchoscopy lasts no longer than 15 minutes, in rare cases causes discomfort and is absolutely safe. In addition, this procedure makes it possible to identify an oncological tumor with metastases, tuberculosis and other serious pathologies of the respiratory system.
Contraindications for bronchoscopy
Due to the fact that the bronchoscopy technique is a surgical intervention, this procedure has a number of contraindications.
The following are absolute contraindications:
- Allergic reactions to anesthesia;
- Hypertension;
- Recent heart attack or stroke (less than 6 months);
- Chronic pulmonary or heart failure;
- Severe arrhythmia;
- Mental disorders (epilepsy, schizophrenia, etc.);
- Aortic aneurysm;
- Narrowing of the larynx (stenosis).
In some situations, bronchoscopy should be postponed:
- During pregnancy (after the 20th week);
- During menstruation;
- With exacerbation of bronchial asthma;
- When blood sugar increases in patients with diabetes.
The need for bronchoscopy and the possibility of performing it can only be determined by a pulmonologist or therapist.
Flaws
Despite the presence of multiple advantages, CT of the bronchi also has disadvantages. During virtual bronchoscopy, the specialist is not able to take an element of the organ being examined for biopsy.
Endoscopic manipulation, in addition to examination, also carries out therapeutic measures - it removes foreign bodies, eliminates bleeding, which cannot be said about computed tomography.
A significant disadvantage for many patients is the high cost. Virtual bronchoscopy is several times more expensive than the standard procedure. Using an endoscope for examination does not expose the body to x-rays.
Advantages of bronchoscopy at MEDSI
- MEDSI clinics are equipped with expert-class equipment for performing bronchoscopy;
- The study is carried out by a team of highly qualified experienced specialists: a pulmonologist, a physician assistant and an anesthesiologist;
- The high accuracy of bronchoscopy makes it possible to diagnose respiratory diseases in 97 percent of cases;
- The procedure is painless, as it is carried out using effective anesthetics, and, if necessary, in a state of medicated sleep;
- The patient's condition during bronchoscopy is under the control of doctors using special equipment for this.
Preparation for the procedure

Before starting the procedure, the patient needs to remove dentures, glasses, contact lenses, hearing aids, if any of the above are available. During bronchoscopy, a local anesthetic spray is used, which is applied to the throat and nasal cavity. The patient may also be given a sedative to help them relax.
A patient scheduled for bronchoscopy should not eat or drink 6-12 hours before the procedure, so it is worth undergoing bronchoscopy in the first half of the day. It is worth talking to your doctor about which medications you should stop taking before the procedure.
Before the procedure, you should empty your bladder. You need to remove all or most of your clothing. The procedure is performed by a pulmonologist and an assistant. During the procedure, heart rate, blood pressure and blood saturation levels will be checked. A chest x-ray must be performed before the procedure.
Before performing a bronchoscopy, the doctor may prescribe other tests, such as a complete blood count, coagulogram, and pulmonary function tests.