Pneumonia or pneumonia is a complication of respiratory diseases of the airways caused by viruses, bacteria, and sometimes fungal microorganisms. They are transmitted by airborne droplets or contact and provoke the development of the inflammatory process.
Any pneumonia is dangerous because it can lead to other serious complications: pulmonary edema or abscess, acute respiratory and heart failure, myocarditis, sepsis.
Lung damage due to pneumonia
Pneumonia affects the alveoli, the end portions of the lungs. They fill with fluid or pus. SARS, as well as the new coronavirus infection (COVID-19), is characterized by pulmonary fibrosis . This is a complication in which the lung tissue is replaced by connective tissue, and pathological growth of connective tissue occurs.
Alveoli are small air cells in the lung, when their volume is reduced due to fibrosis or fluid accumulation, critical respiratory failure occurs. A person experiences shortness of breath, coughs with sputum (sometimes with blood), and body temperature rises.
Sometimes the disease is asymptomatic, and this is especially dangerous since the carrier of the virus and pathogens continues to lead a normal and, no less important, social life. Meanwhile, his lungs are gradually collapsing. If pneumonia with focal lung damage is not detected in time and treatment is not undertaken, the consequences can be severe and irreversible.
Pneumonia can be unilateral or bilateral. If the lungs are affected by 10-25% or less, then the disease can be treated outpatiently. Damage to lung tissue of 30-50% is already an indication for hospitalization. If more than 50% of the lungs are affected, this indicates a severe form of pneumonia.
However, signs such as respiratory failure, cough, fever and runny nose are also characteristic of other diseases: ARVI, influenza, bronchitis and even allergies. How to identify pneumonia and distinguish pneumonia from other respiratory diseases?
Let's consider what symptoms are characteristic of pneumonia, who is most susceptible to pneumonia, and how it is diagnosed.
How many times can an x-ray be taken?
If we are talking about analog devices, then experts recommend a break between irradiations of 3 weeks and take one photo per visit.
. However, it happens that it is necessary to increase the number of studies, then they are carried out every couple of days, reducing the negative impact as much as possible. Several x-rays on an analog device in one day can have a bad effect on your health.
The invention of digital equipment has made it possible to greatly reduce risks and allow for more frequent x-ray examinations. There is no longer any need to make compromises between harm and health benefits; doctors prescribe as many procedures as necessary to effectively monitor the progress of treatment.
Pneumonia: who is at risk?
At the turn of the 19th-20th centuries, before the discovery of penicillin and the introduction of universal vaccination, most patients died from pneumonia and other complications of acute respiratory diseases. Assessing statistics on deaths and disability, Sir William Osler, known as the “father of modern medicine,” called pneumonia “Captain of the men’s death”, since by 1918 the number of victims of this disease exceeded mortality from tuberculosis.
However, with the development of radiological diagnostic methods, X-rays, and then modern computed tomography, doctors have a tool for intravital assessment of the patient’s lung condition, determining effective treatment tactics and identifying pneumonia at an early stage - before it becomes severe.
The predisposition to developing pneumonia depends on the patient’s age, heredity, medical history and lifestyle. However, under certain circumstances, even a completely healthy adult is not immune from pneumonia. “Trigger mechanisms” include: contact with a carrier of pathogenic microorganisms (pneumococci, streptococci, mycoplasmas, coronavirus, fungi), systematic stress and lack of sleep, smoking, hypothermia, weakened immunity, some concomitant diseases, pulmonary fibrosis and a history of chronic ENT pathologies with relatives.
It is known that pneumonia is more susceptible to:
- Elderly people and children;
- Patients with diabetes;
- Patients with cardiovascular diseases (heart failure);
- Smokers;
- Patients with congenital pathologies of the respiratory tract or chronic ENT diseases (tonsillitis, bronchial asthma, obstructive pulmonary disease);
- Patients with suppressed immunity;
- Patients with exogenous intoxication (alcohol and other toxic substances);
- Patients with damaged teeth and gums (caries, pulpitis, tartar);
- Patients with Parkinson's disease;
- Workers in production facilities, medical dispensaries, etc.
Such patients need to especially carefully monitor their health and listen carefully to their body.

Types of fluorography
Film FLG is the cheapest diagnostic method, but in 15% of cases there is no accurate result, defects occur, which is why the study has to be repeated. And this is the second dose of radiation. In addition, the picture is obtained only in 1 copy.
Digital FLG does not have these disadvantages and the radiation dose is lower. With modern software, the doctor can examine the image even after the examination is completed.

The data is saved, and if necessary, after digital fluorography of the lungs, the patient can ask to print the number of images he needs. This may be necessary in complex diagnostic cases, when it is necessary to contact several doctors.
Fluorography remains today a preventive diagnostic method. Every year, the population of the Russian Federation who has reached 18 years of age undergoes fluorography.
Signs of pneumonia
The most common viral pneumonia (or rather “pneumonia”) is characterized by the following symptoms:
- Cough of any nature: dry, wet, with sputum, purulent discharge, blood.
- Temperature - the patient may have a fever (39-40 degrees) and a slightly elevated body temperature.
- Chest pain and discomfort.
- Shortness of breath and wheezing in the chest, which can be heard when listening to the lung.
- Feeling of lack of air.
- Confusion.
- Prostration.
- A sore throat.
- Pain in muscles and joints.
Important! Pneumonia can be completely asymptomatic, and sometimes the presence of even 1-2 signs indicates lung damage.
Methods for treating bronchitis
Regardless of whether bronchitis can be seen on an x-ray, treatment is prescribed by a doctor and depends on the type of pathogen. For bronchitis of bacterial origin, antibiotics are prescribed, for viral bronchitis, antiviral agents, and for fungal bronchitis, antifungal agents. Symptomatic treatments are used to relieve sore throat and nasal congestion, if necessary. In addition to basic medications, massage and exercise therapy are prescribed to facilitate and accelerate the release of mucus from the bronchi.
With chronic bronchitis, it is very important to eliminate the factors that provoke it. Otherwise, no treatment will help, and there is no doubt whether an x-ray will show bronchitis at the next examination.
Symptoms of SARS and COVID-19
What does the term “atypical pneumonia” mean? It is used when they want to emphasize that pneumonia is caused by microorganisms or causes that give a complex and unpredictable clinical picture. In this case, an atypical course of the disease is observed, relapses and complications are possible, which will require long-term rehabilitation.
SARS refers to pneumonia caused by mycoplasma and chlamydia. In this case, as with COVID-19, adults experience symptoms:
- Shortness of breath and shortness of breath;
- Loss of smell;
- Severe dry cough, which eventually turns into a wet cough with discharge;
- General poor health: even a temperature of 37 degrees is difficult to tolerate and lasts a long time;
- Pain in muscles and joints;
- Chest pain.
Just as in the case of ordinary pneumonia, some people experience an asymptomatic course of the disease. With coronavirus, the patient may have a runny nose with loss of smell, but there is no sneezing (unlike colds and flu).
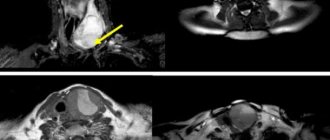
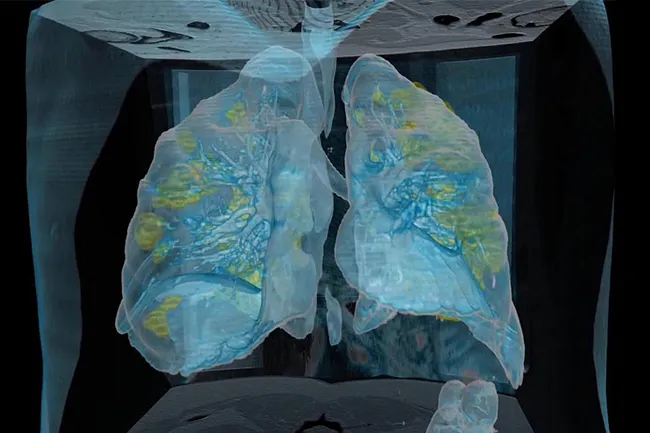
Pneumonia can only be reliably identified or excluded using computed tomography of the lungs. A tomogram of the lungs shows lesions in the respiratory tract (“ground glass”). Laboratory tests will help identify specific pathogens of pneumonia based on the response of the immune system.
Reasons for the development of the disease
In most cases, the nature of bronchitis is viral; this disease accompanies adenovirus infection, pneumonia, and influenza. However, in some cases, the development of bronchitis can be caused by bacteria: staphylococci, streptococci and others. They often accompany viral diseases. Smoking and prolonged inhalation of dust and pollutants can contribute to the development of bronchitis. Less common are cases of bronchitis of a fungal nature, as well as due to anomalies in the structure of the bronchopulmonary system. Bronchitis is more common in adults than in children.
How to identify pneumonia: examination algorithm
1. Consult your doctor - after studying your case, the doctor will draw up an examination plan. Pneumonia is classified according to a number of characteristics (pathogen, location). Pneumonia can be bilateral, focal (bronchopneumonia), viral-bacterial - and the treatment regimen depends on this. Be prepared for the fact that if there is a suspicion of pneumonia, you will be prescribed tests and radiation diagnostics.
2. Get tested - laboratory PCR diagnostics will help differentiate pneumonia. This is important because viral and bacterial infections are treated differently. However, under certain circumstances, tests can give false positive or false negative results. For example, it is known that with the COVID-19 coronavirus, primary tests have an error of about 30%.
3. Check the lungs using reliable X-ray diagnostic methods - a chest scan will show lesions in the lungs, if any. Today, computed tomography (CT) of the lungs is recognized as the most informative and accurate way to diagnose pneumonia.
Unlike fluorography and x-rays, CT scan of the lungs will reliably show areas of lung damage even at the early stages of pneumonia (1 and 2), when the percentage of destruction of lung tissue may not exceed 10%. On tomograms, such areas of the lungs look like “frosted glass” or highlights. In this case, the patient will have time to start treatment on time, and there is no need for fluorography or x-rays. When the disease progresses to a more severe form 3 or 4 (a regular x-ray will show such pneumonia), it is no longer possible to cope with pneumonia at home and without subsequent special rehabilitation.
If the patient really has pneumonia, CT scans will visualize foci of destructive changes (swelling of the alveolar walls, fluid accumulations), and there will be several “ground glass” spots on the images. For example, with coronavirus they are usually located peripherally on both sides - in the posterior and lower parts of the lungs. One “frosted glass” may indicate other diseases (allergy, bronchial asthma) or an oncogenic process.
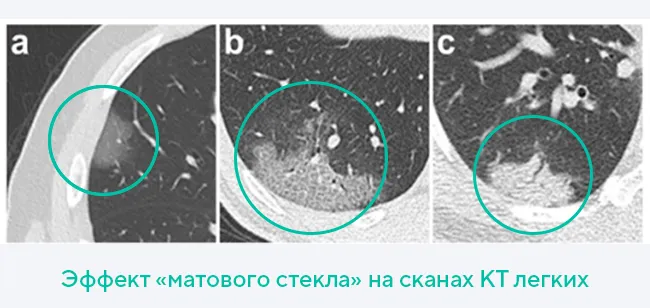
Thus, based on the presence of “ground glass” on a tomogram of the lungs and their location, doctors diagnose pneumonia. Additional examination methods (pulse oximetry, blood and sputum tests) are needed to determine treatment tactics.
Diagnosing pneumonia is a complex process in which doctors compare data and key markers to make an accurate diagnosis. The success of therapy and rehabilitation after pneumonia will depend on this, since it is also important to minimize the consequences of the disease.
Contraindications
X-ray is an informative study that has almost no contraindications or age restrictions. But pictures cannot be taken if the patient is in serious condition. Sometimes minimal exposure causes severe consequences.
X-ray examination is prohibited during pregnancy. Radiation disrupts the development of the fetus and causes its death. For infants after 2-3 months of life, x-rays are not contraindicated and help prevent serious illness and its consequences. X-rays are considered cutting-edge technology in medicine.
With a low dose of radiation, it provides a clear image of organs and pathological changes in them. But only a doctor knows what bronchitis looks like in a picture, so you should not try to diagnose the disease yourself.
Author: Glushko Raisa Therapist, pulmonologist, immunologist
CT scan of the lungs for SARS and COVID-19
Today, CT scan of the lungs is considered the “gold standard” for diagnosing pneumonia, since it accurately shows the extent of lung damage even in the early stages. The sensitivity of fluorography and x-rays is significantly lower. For example, on an x-ray, the doctor will see areas of heterogeneous darkening, which can be interpreted as pneumonia, when pneumonia has already reached stages 3 and 4. Errors cannot be excluded in laboratory tests. Therefore, the most optimal type of radiation diagnosis for pneumonia will be modern computed tomography, eliminating the need for other radiographic studies.
During the SARS (2002) and MERS (2012) epidemics of atypical coronavirus pneumonia, doctors were faced with a problem - the inaccuracy of laboratory tests. In the case of the new coronavirus infection COVID-19, approximately 30 out of 100 patients who had their blood and sputum tested had false negative results. Only when the patients' condition worsened did CT scans reveal clinically significant areas of lung tissue destruction. It turned out that coronavirus pneumonia is best visualized on a CT scan of the lungs. Areas of damage to the alveoli correspond to “ground glass”—light areas of the lungs that are clearly visible on CT scans.
A CT scan of the lungs is done according to a doctor’s indications or independently if there are symptoms of pneumonia. If ARVI or atypical viral pneumonia caused by COVID-19 is suspected, it is recommended to do a CT scan of the lungs. In this case, the study will allow us to determine the specifics of the changes, and therefore will be the most informative. If necessary, the patient may be prescribed other examination methods in a medical institution.
Indications for use
Fluorographic examination is mainly used for preventive purposes to detect tuberculosis and malignant tumors. Helps in diagnosing pneumonia and bronchitis. It is carried out annually during medical examinations, routine medical examinations, and when applying for a job.

The examination does not take much time, the device is mobile, and is easy to disinfect.
Therefore, since the beginning of the pandemic, scientists have been exploring the possibility of using this method in diagnosing Covid-19.
It was found that fluorography cannot detect the presence of coronavirus in the body; it only detects changes in lung tissue. But due to its accessibility and ease of implementation, this method continues to be used. Doctors recommend undergoing a fluorographic examination if the patient has breathing problems:
- dyspnea;

- dry cough;
- chest congestion;
- pain in the lungs when inhaling;
- respiratory rate is more than 22.
The diagnosis is made based on examination data taking into account these symptoms. But fluorography is recommended for mild infections, when there is no breathing problem.

The examination should be carried out 2-3 weeks after contact with patients or 8-10 days after the onset of ARVI symptoms. If signs of pneumonia are detected on a fluorographic image, an additional CT scan or x-ray in two projections is prescribed.