Traditional methods of examining the internal structures of the abdominal cavity often bring discomfort to patients. Most of them are carried out using the method of invasion (penetration). This not only causes discomfort, but also causes additional injuries. Patients with a low pain threshold experience severe pain, which makes procedures difficult.
Nuclear resonance screening falls into the category of non-invasive technologies. The research is carried out “remotely”. It is enough for a person to be in the field of action of a magnetic installation. Contrary to popular belief, there is no harmful radiation exposure during MRI. The technique is based on the generation of a natural magnetic field. The waves do not accumulate in living tissues and do not destroy the cellular structure. The immune and nervous systems do not undergo changes.
The diagnostic method is relevant when studying all areas of the body. It is also used to identify diseases occurring in the peritoneal area. An MRI of the abdominal cavity can be performed at any diagnostic center equipped with a highly powerful hardware installation.
The website contains a detailed list of clinics providing diagnostic services. Medical institutions are distributed by rating and popularity. You can get tested in any area of the city. Operators of the unified consultation center will help you sign up for a session and answer questions. Call center contacts are located at the top of the page.
Types of abdominal MRI
Diagnosis of diseases of internal structures is carried out in different modes. The standard protocol involves a survey study. In case of vague symptoms or the impossibility of making a correct diagnosis, a primary MRI of the abdominal organs is prescribed. During the procedure, diagnosticians look at:
- soft fibers;
- urinary system;
- glandular tissue of the adrenal glands;
- vascular channels;
- liver;
- pipes that remove bile;
- gastrointestinal tract;
- lymphatic collections;
- spleen
There is no targeted examination for this type of MRI. Radiologists record the object’s location, configuration, size, density, tissue permeability, and “power” of the blood supply.
If a complex pathology is suspected, a procedure with additional enhancement—contrast—is prescribed. Most often, the coloring agent is introduced into the bloodstream using a manual injection or an automatic injector. Before the session begins, the patient must notify the doctor on duty about the presence of allergies to pharmaceuticals. Modern coloring solutions are hypoallergenic. But there is no need to take risks; it is advisable to undergo testing in advance for immune rejection to the drug.
Contrast helps you take clear, high-resolution photographs. Without preliminary staining, areas with focal inflammation are difficult to distinguish. Small tumor formations may also not manifest themselves. With enhanced contrast, even microscopic deviations from the norm become noticeable.
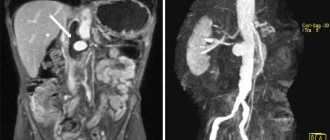
If there are problems with vascular channels, MRI of the venous tracts and arteries is prescribed. A targeted study of the circulatory system allows adjacent tissues and objects to be relegated to the background. Only the vasculature is clearly visible on the images. MR angiography has a similar effect.
During the process, the patient does not feel pain, discomfort or mechanical impact. The only exception is scanning in contrast mode, which requires minor damage to the skin during catheter insertion.
MRI of the gallbladder
An excellent complement to magnetic resonance imaging of the liver is non-contrast magnetic resonance cholangiopancreatography—that is, magnetic resonance imaging (MRI) of the gallbladder and bile ducts (MRCP). MR cholangiography is a study of the bile ducts for stones, obstruction and other pathologies. This type of diagnosis is relevant before operations or in case of acute pain, when there is a suspicion of “stones” in the gall bladder. It provides a bright signal only from free fluid (bile) and is non-invasive, unlike diagnostic endoscopic retrograde cholangiopancreatography (ERCP), which is associated with a high complication rate. Magnetic resonance (MRI) cholangiography allows reliably diagnosing lesions of the gallbladder and biliary tract. It is also successfully used in the diagnosis of anomalies and strictures of the bile ducts, sclerosing cholangitis, choledocholithiasis, that is, the detection of stones in the gallbladder and bile ducts.
What can be seen on an abdominal MRI
The full-scale study is based on the principle of recording signals emitted by cellular particles of biological fibers. When living tissue is placed in the field of a strong magnet, the hydrogen atoms in it begin to resonate. During resonance, certain signals are emitted, which are recorded by sensitive sensors. The patient does not feel such an effect, but the computer system picks up the signature, processes it and transmits it to the monitor. Functional diagnosticians not only see the general condition of the patient’s internal structures, but have the ability to maximize the problem area.
Modern machines are capable of not only producing static photos, but also combining them into multidimensional projections. The radiologist can rotate such models at different angles and bring them closer to the required depth. MRI takes pictures in a cross section. Photographs are taken at a minimum distance from each other. Obvious and microscopic abnormalities are determined in one procedure. This allows you to detect the disease as quickly as possible and begin timely treatment.
An MRI scan of the abdomen provides the following information:
- configuration, dimensional data;
- genetic changes, congenital developmental disorders;
- foci of infection, spread of inflammatory processes;
- cystic capsules, obstruction, tissue degeneration;
- tumor formations of various nature;
- blood flow disturbance;
- destruction of vascular walls;
- death of neurons;
- solid objects in the outlet channels;
- migration of cancerous processes.
During the study, regeneration processes after surgery and relapses of the disease are clearly visible. The procedure is required to be completed during the preparatory period before the operation. Neurosurgeons often use hardware visualization during instrumental manipulations.
When is it necessary to undergo an MRI of the abdominal organs?
Due to the high cost of the procedure, MRI is rarely prescribed as a primary research method. The main reason for issuing a referral for screening is the impossibility of making a diagnosis and the low effectiveness of other diagnostic methods. For patients registered at the oncology clinic, diagnostics are required in multiple quantities. Over a certain period of time, the attending physician is obliged to observe the dynamics of the development of the tumor and the effectiveness of the treatment.
The main reasons for prescribing abdominal screening are:
- unreliability of results provided by ultrasound, x-rays, computed tomography, etc.;
- post-traumatic condition of the patient requiring emergency diagnosis;
- symptoms of internal bleeding;
- ischemia of internal structures;
- infection of unknown nature;
- accumulation of a liquid substance in the retroperitoneal space;
- palpable enlargement of the spleen or liver;
- icteric manifestations, blockage of bile ducts;
- identified genetic disorders, congenital injuries;
- signs of cancer;
- proliferation of benign objects;
- complications in the postoperative period;
- contraindications to alternative procedures and diagnostic methods.
The patient cannot independently diagnose the anomaly that appears on the images. Radiologists are also not involved in making a final diagnosis. Their area of responsibility includes only high-quality MRI and description of the results obtained. After the tomography, you need to go for a consultation with your doctor or consult with the radiologist on duty about further actions.
MRI of the liver and gallbladder
Currently, magnetic resonance imaging (MRI) of the liver is the most informative method in the diagnosis and differential diagnosis of focal liver lesions. MRI of the liver allows you to accurately determine the presence of hemangiomas, adenomas, focal nodular hyperplasia, hepatocellular carcinoma and other tumors. MRI of the liver can be performed for certain indications with the introduction of paramagnetic contrast agents. When using contrast enhancement (based on gadolinium salts), for example, it is possible to differentiate the most common focal pathology of the liver (cysts, hemangiomas, metastases), the diameter of which exceeds 1 cm. A carbohydrate-free diet can be prescribed 2-3 days before an MRI of the liver.
Are there any prohibitions on MRI of the abdominal organs?
Any medical procedure has a list of absolute and variable restrictions. Nuclear resonance imaging is completely contraindicated in the following cases:
- The presence of implanted ferromagnetic or electronic devices, stimulators. If the patient does not have the opportunity to temporarily remove foreign elements, the procedure is prohibited. When approaching a powerful magnetic field, metal “reacts” strongly. Implant parts can become very hot, deform, and shift inside the body. In addition to critical consequences for the patient, equipment may be damaged.
- Pregnancy in the early stages of development. Due to little knowledge of the influence of magnetic fields on the intrauterine fetus, doctors prohibit exposing the unborn child to any external influence. The contraindication applies only to the first trimester. From 13-14 weeks the restriction is lifted, but only according to the testimony of the attending physician.
- Allergic rejection of components included in contrast solutions. A study in enhanced mode is not prescribed if the patient has an immune reaction to the dye. Intravenous administration of the dye can lead to the development of anaphylactic shock, Quincke's edema and other allergic manifestations.
- Urinary dysfunction during the planned administration of contrast. If a patient has chronic diseases of the CF system, the use of contrast staining can lead to intoxication of the body. In a normal situation, the dye is excreted naturally through the kidneys within 1-2 days. When retained in body tissues, the substance begins to poison them.
- Body weight exceeding 120-200 kg. MRI hardware units are manufactured in standard sizes. It is difficult for an obese person to fit inside the car. In this case, it is recommended to use the services of an open tomograph.
- Unstable mental state. With neurological disorders, the patient is unable to control motor skills. The quality of the projected images depends on how calmly the client behaves during the MRI.
- Severe, shock state, unbearable pain. These pathologies are an obstacle to scanning for the same reason as neurological disorders.
Contraindications
For standard tomography, contraindications are minimal:
- The presence of metal structures in the body. Plates, clips, insulin pump.
- Having electronic devices in the body, such as a pacemaker.
- Body weight over 120-130 kilograms. The contraindication is relative; you can undergo the procedure at the doctor’s discretion and with his permission.
- Pregnancy in the first trimester. Also subsequent stages of gestation. An exception is if the study is authorized by the gynecologist who is caring for the expectant mother.
- Fear of confined spaces. The issue is resolved by using a closed-type tomograph with a wide tunnel. If high detail is not required, you can get by with a low-field device rather than a high-field one.
- Hyperkinesis, which does not allow you to lie quietly.
- Mental inadequacy.
Many contraindications are relative and temporary.
How to prepare for an MRI of the abdominal organs?
The biological components included in the structure of the abdominal cavity have a dynamic state. Many objects are “hidden” behind the LCD path, which is in constant motion. If you do not undergo thorough preparation, the effectiveness of the study is reduced by 60-70%.
You should start preparing for an MRI a few days before the procedure. To unload and “calm” the intestines, you will have to turn to dietary recommendations. Your doctor will provide you with a list of prohibited foods that cause increased gas production. There is no need to limit your water intake, but you must come to the procedure on an empty stomach.
It is advisable to schedule the scan in the morning, since it is easier for the patient to skip breakfast and come for diagnosis after a night's rest. If there is no natural bowel movement on the day of the tomography, you should resort to cleansing enemas or laxatives. If necessary, the doctor may prescribe a course of medications that reduce flatulence.
Before sending a patient for an MRI, a medical specialist conducts rapid testing to determine whether the immune system is resistant to gadolinium. A woman is required to undergo pregnancy testing, even if she is sure there is no pregnancy. Before starting the examination, it is advisable to take antispasmodics and visit the toilet.
Don’t forget about the necessary documentation (medical record, referral, previous images). It is better to come to the session in comfortable clothes, as you will have to take a lying position. If clothing does not fit, the clinic will provide the patient with a hospital gown or disposable underwear.
Sequence of actions for MRI of the abdominal cavity
The screening process is divided into several stages:
- Preparatory stage. At this stage, the patient is registered and instructed. The laboratory assistant accompanies the client to the room with the equipment and tells how the procedure will take place. Next, the patient is placed on a retractable conveyor and fastened with belts to avoid mixing the body during the examination. Sensors are attached to the area of the abdominal cavity.
- MRI scan. The couch with the patient's body is placed inside the unit. Screening begins. The device slowly moves along the couch, producing booming sounds. The clinic staff is located in the next room. The doctor monitors the progress of the procedure through a transparent partition and a computer monitor. If complaints or discomfort arise during the session, you can report this through the public address system. The doctor will pause the diagnosis.
- Interpretation of research results. After completing the tomography, the client is escorted to the rest room, where he must wait for the results to be deciphered and a final description of the images obtained to be prepared.
The duration of an MRI does not exceed 30-90 minutes. Preparing a conclusion takes time from an hour to a day. At the request of the person, the finished documentation can be sent digitally to an email address.
How is the procedure done?
On average, the study lasts from 30 to 50 minutes, depending on which organs need to be checked. There is a table inside the device; you need to lie down on it. In order to give the patient's body the desired position and ensure immobility, special bolsters and belts are used.
If the study is carried out with contrast, a solution of the drug is administered intravenously or given to drink.
Sometimes, so that the patient can lie motionless inside the device, light anesthesia - sedation - is used.
While the device takes pictures, the patient must lie still, and the doctor is in the next room and gives commands through a microphone. Periodically, he asks you to hold your breath - this is necessary so that the internal organs do not move during the movements of the diaphragm, and the pictures turn out clearer.
Then the MRI of the abdominal cavity is deciphered. With the result, you need to visit your doctor, he will establish an accurate diagnosis and give further recommendations.
To perform a magnetic resonance imaging of the abdomen, it is not necessary to be hospitalized in a hospital; this procedure can be performed on an outpatient basis.
We will call you back, leave your phone number
Message sent!
expect a call, we will contact you shortly

Complications after MRI of the abdominal cavity
Over a long period of clinical use of the hardware research method, no negative effects have been recorded. Most installations have a declared power not exceeding a magnetic field frequency of 1.5 Tesla. This power does not cause harm to the patient's body. Radiation is not used, tissues and organs do not lose their integrity. Contrast agents are developed on the principle of hypoallergenicity.
After the procedure, the patient does not require rehabilitation. A person can go about his business immediately after the MRI. The hardware test does not affect his well-being or performance in any way.
Next steps after an abdominal MRI
Highly focused specialists from various fields of medicine use MRI as a research technology. When receiving the results, you should not expect a final diagnosis from the diagnostician on duty. With a description of the pathologies and printed photographs, you need to go to the doctor who referred the patient for the study.
If the procedure was performed at the client’s own request, and he does not know what to do next with the documentation received, he should consult with a radiologist. Diagnostic centers often see medical specialists of various specialties. It is possible to use their services.
MRI of the pancreas
The role of magnetic resonance imaging (MRI) in diseases of the pancreas is increasing. Experts note that this method is effective in diagnosing pancreatic tumors. An MRI of the pancreas is performed to identify the most common diseases of this organ:
- malignant tumors of the pancreas,
- benign tumors and cysts,
- acute and chronic pancreatitis
A low-carbohydrate diet may be prescribed 2-3 days before an MRI of the pancreas.