A tank culture from the urethra in men is a microbiological study of the composition of the microflora of the urethral canal. Normally, in men, the urethra may contain a small number of gram-positive cocci and rods, and the seminiferous tubules and prostate should be sterile.
The results of this study are necessary for the diagnosis of infectious diseases of the genitourinary system and for identifying the causative agent of infectious inflammation, as well as for determining the level of fertility.
In healthy males, the distal parts of the urethra are contaminated with cocci and gram-positive rods in small volumes. The proximal urethra, vas deferens and prostate are sterile.
Isolated pathogens (opportunistic bacteria): non-fermenting gram-negative bacteria, enterobacteria, streptococci, coryneform bacteria, enterococci, staphylococci, hemophils and yeast-like fungi.
The basis of radical and effective treatment is the use of antibiotic drugs, determined using the latest research method - microbiological diagnostics.
general characteristics
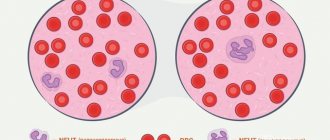
Discharge from the urethra is examined to diagnose the inflammatory process in urethritis of various etiologies (bacterial urethritis, gonorrhea, trichomoniasis, chlamydia, etc.). When examining discharge from the urethra, the number and composition of cellular elements depend on the severity and duration of the inflammatory process. The inflammatory state of the mucous membrane of the urethra (urethra) is expressed by the presence of more than 4 polynuclear neutrophils in the field of view. The depth of the pathological process in the urethra is evidenced by the predominance of columnar and parabasal epithelium in the preparations.
Non-gonococcal urethritis in men: etiology and rationale for etiotropic therapy
The term nongonococcal urethritis (NGU) was first coined in 1954 to describe cases of inflammation of the urethral canal caused by an infection other than gonococcus. Before this, the origin of any urethritis was considered gonococcal, and cases of absence of gonococcus in the material from the urethra were explained by diagnostic difficulties.
Statistical data indicate that NGU is a widespread disease, both in the Russian Federation and abroad. If in 1996 in the USA the incidence of NGU detection was 2 million cases per year (SO Aral et al., 1999), then by 2000 it had already increased to 3 million cases per year (CDC, 2000). In the world, according to a total estimate, about 50 million cases of NGU are registered annually (SO Aral et al., 1999). According to official data alone, about 350 thousand people in Russia fall ill with NGU every year, but these figures are clearly underestimated due to insufficient registration of infections causing NGU.
Etiological factors of NSU
Nongonococcal urethritis in men can be caused by a wide variety of pathogens, including obligate pathogens such as Chlamydia (C.) trachomatis or Mycoplasma (M.) genitalium, and opportunistic pathogens such as other mycoplasmas, particularly Ureaplasma (U.) urealyticum. NGU can also be caused by viruses and protozoa.
The role of chlamydia in the occurrence of NGU. In the 70–80s. In the last century, it was believed that about 50% or more of NGU cases were caused by chlamydial infection. Studies over subsequent decades have demonstrated a significant reduction in the incidence of urethritis in men caused by C. trachomatis - up to 20% or less (M. Shahmanesh, 2001; M. A. Gomberg et al., 2002; CS Bradshaw et al., 2006). At the same time, in recent years in the Russian Federation, the incidence of urogenital chlamydial infection has taken first place among all bacterial sexually transmitted infections (STIs). In our country, since 2004, this is the second most common registered STI after trichomoniasis.
Urethritis caused by C. trachomatis usually manifests itself with scant clinical symptoms, but can be accompanied, although this is atypical, by signs of acute inflammation, similar to those characteristic of gonorrhea.
The role of genital mycoplasmas in the occurrence of NGU. It has been established that humans are the natural host of 13 species of mycoplasmas, of which M. hominis, M. genitalium and U. urealyticum may be possible causative agents of NGU. In addition to these types of mycoplasmas, M. fermentans, M. primatum, M. pirum, M. spermatophilum, M. penetrans, M. pneumoniae are also found in the urogenital tract. Their role and interaction with the human body is being actively studied today, but so far their significance in the occurrence of urethritis in men is not entirely clear. Thus, S. Sharma et al (1998), using polymerase chain reaction (PCR) in addition to bacteriological research, identified M. pneumoniae in men who suffered from recurrent urethritis and complained of pain in the urethra and prostate gland.
The question of the role of genital mycoplasmas in the etiology of NGU remains unresolved due to the widespread distribution of these microorganisms and their frequent detection in individuals without clinical symptoms. Researchers have differing opinions on this issue. Some authors tend to classify mycoplasmas as obligate pathogens that cause urethritis, cervicitis, prostatitis, postpartum endometritis, pyelonephritis, infertility, and various pathologies of pregnancy and the fetus. Accordingly, according to these authors, eradication of mycoplasmas should be achieved if they are detected. Others believe that mycoplasmas are opportunistic flora of the urogenital tract, and only under certain conditions can cause infectious and inflammatory diseases of the genitourinary organs. Most foreign authors classify all mycoplasmas, with the exception of M. genitalium, as opportunistic flora. That is why diseases such as “mycoplasmosis”, “ureaplasmosis” or “ureaplasma infection” are not registered in ICD-10. According to many researchers, among mycoplasmas, without any reservations, only M. genitalium can be classified as a pathogen capable of causing urethritis. However, experiments on experimental models, experiments on autoinoculation of U. urealyticum culture, as well as studies of the immune response of the macroorganism prove the participation of these prokaryotes in the occurrence of NGU. Statistical studies have established a significant correlation between the presence of ureaplasma in urethral smears and chronic NGU, while at the same time, no reliable relationship between U. urealyticum and acute NGU has been identified (P. Horner, 2001). The role of U. parvum in the occurrence of urethritis has also not been proven.
Indicators of infection of the urogenital tract with mycoplasmas are very inconsistent and among the sexually active population vary from 10 to 50%. In patients with NGU, U. urealyticum is isolated in 20–34% and higher (V.I. Kisina, 2002). Ureaplasma is usually found in people who are sexually active, and most often these microorganisms are detected in people who have three or more sexual partners. Generalized data on the epidemiology of M. genitalium were presented by David Taylor-Robinson (2001) based on an analysis of the works of 19 of the most authoritative researchers, according to which these microorganisms were isolated in 10–50% of patients with NGU and in 0–17.7% of healthy individuals. Later, N. Dupin and co-authors (2003) showed that the disappearance of these microorganisms from the urethra is accompanied by resolution of urethritis, and vice versa - relapse of the disease may be associated with the use of drugs that are not sufficiently active against M. genitalium.
The clinical picture of urethritis, in which mycoplasmas are detected, as well as with chlamydia infection, does not have pathognomonic symptoms. M. genitalium is more often found in individuals with chronic urethritis, for which it is a likely cause of recurrence. L. Mena et al (2002) showed that patients with M. Genitalium-associated urethritis complain of dysuria and discharge to a lesser extent than patients with gonococcal urethritis, and their discharge is much less likely to be purulent in nature.
As in most cases of identifying opportunistic flora, for mycoplasmas a number of factors are identified that contribute to the development of infectious and inflammatory processes. The most important of them are immune disorders, changes in hormonal status, massive colonization, and associations with other bacteria. All these factors should be taken into account when choosing management tactics for such patients.
The role of aerobic and anaerobic saprophytic flora in the occurrence of NGU. The role of various saprophytic flora in NGU is highly controversial. On the one hand, it is obvious that often high levels of colonization of the urogenital tract by these bacteria are found in men with urethritis, but, on the other hand, often the same high levels of colonization are detected in men without signs of inflammation. It can be assumed that in some cases, individual representatives of opportunistic flora or their associations, due to certain conditions, are capable of becoming causative agents of urethritis, and in other situations they can support inflammation initiated by other factors.
Studies of patients with NGU have shown that this disease can be a manifestation of urinary infection of the upper urinary tract, the main role in which is played by gram-negative microbial agents - Pseudomonas aeruginosa, Proteus spp., Escherichia coli, etc.
(I. Schugt et al., 2004). There is also information about the certain importance of gram-positive flora - Staphilococcus spp., Corinebacterium spp. In such cases, when the role of this flora in the occurrence of NGU is likely, when choosing adequate therapy, it is necessary to determine the sensitivity of these microorganisms to antimicrobial drugs (WW Li et al., 2003). Research conducted in the early 90s. last century (JC Lefevre et al., 1991), indicate the frequent detection of Haemophilus spp., Gardnerella vaginalis, group B streptococci and Escherichia coli in patients with urethritis.
Pathogens of intestinal infections have attracted attention as agents capable of causing NGU, due to the possibility of transmission of these microorganisms through orogenital and anogenital contacts. The potential ability of enterobacteria to cause infection of the urethra was pointed out by Yu. K. Skripkin and co-authors (1999). As V.P. Kovalyk (2006) showed in his work, often NGU caused by opportunistic flora are the result of unprotected orogenital and anogenital contacts.
With urethritis, various types of non-gonococcal neisseria are detected, and in 85% of cases it is Neisseria (N.) meningitidis (M. Maini et al., 1992). The likely routes of transmission in these cases may be orogenital or anogenital sexual contact, which most of these patients have a history of. Occasionally, such urethritis clinically strongly resembles a gonococcal infection, accompanied by purulent discharge and significantly pronounced dysuria.
Often, when examining the urethral contents of both healthy people and men with NGU, anaerobic bacteria are detected. Information about the role of anaerobes in the occurrence of urethritis is contradictory. Most researchers have not found any evidence of a pathogenic role for these microorganisms. In the course of microbiological studies devoted to the comparative study of the bacterial flora of the urethra in healthy and patients with NGU, no significant differences in this matter were identified. EA Fontaine et al (1986) noted only that Bacteroides urealyticus may be involved in a small number of cases of NGU due to the fact that this species is slightly more often identified in men with NGU than in healthy individuals.
The role of anaerobes could be indirectly judged by the results of double-blind, placebo-controlled studies on the use of metronidazole, which is active against these microorganisms. However, the work of PD Woolley et al (1990) showed that the use of metronidazole in addition to tetracycline did not improve the effectiveness of NGU therapy. At the same time, DA Hawkins et al (1988), using metronidazole, found that in cases where the disease was associated with anaerobic bacteria, positive dynamics were noted significantly more often than in the group without anaerobes.
In addition to the listed representatives of the opportunistic flora, the etiological or associated agent in NGU, according to the literature, turned out to be Streptococcus (Str.) pneumoniae, Str. viridans, Str. mitis, Str. Sanguis, Str. anginosus, Str. agalactiae, Enterococcus faecium, N. subflava, N. perflava and N. flava, Staphilococcus (S.) aureus, S. epidermidis, Corynebacterium pseudodiphtheriae, bacteria belonging to the genera Enterobacter (Spp.), Proteus (Spp.), Branhamella ( Spp.), Moraxella (Spp.), Pseudomonas (Spp.), etc.
The role of protozoa in the emergence of NGU. Almost the only representative of this group of microorganisms that can be the causative agent of urethritis is Trichomonas (T.) vaginalis. They were first described by Alfred Donne in 1837, long before the discovery of other currently known STIs. For a long time, T. vaginalis was considered as a urogenital pathogen that causes inflammatory diseases of the female genital area. Currently, the share of these protozoa in the etiological spectrum of NGU in men is, according to some reports, up to 17%. At the same time, when examining men who were sexual partners of women infected with T. vaginalis, trichomonas were isolated only in 14–60% of cases (JN Krieger et al., 1995). Trichomonas infection in men is often asymptomatic. If symptoms are present, the clinical picture of trichomonas infection in men is represented in most cases by acute NGU, usually short in duration. Also, protozoa were detected in 15% of patients with persistent urethritis. Trichomonas infection is one of the most common STIs in the world: about 174 million people become ill with it every year (WHO, 2001).
There is evidence of an etiological role in urethritis of other protozoa - Giardia lamblia and Entameoba histolytica (VM Licea et al., 2005; JG Meingassner et al., 1981), mainly in men who have sex with men.
The role of viruses in the occurrence of NGU. According to modern concepts, the herpes simplex virus (HSV) may be the cause of urethritis (PJ Horner, 2001). Work carried out using modern diagnostic methods has shown that herpetic urethritis is detected in 42.4–46.6% of cases in men suffering from recurrent genital herpes (E. S. Baluyants, 1991; T. B. Semenova et al., 2001). According to foreign studies, the frequency of detection of HSV in urethritis ranges from 6 to 25% (PD Sturm et al., 2004; AA Oni et al., 1997). According to V.P. Kovalyk (2006), in 44.4% of patients with NGU that arose after unprotected orogenital contact, the etiological cause of urethritis is HSV.
V.N. Grebenyuk and co-authors (1986) noted that the association of HSV with gram-negative bacteria increases the pathogenicity of each pathogen and is the reason for the resistance of urethritis to treatment.
According to N. Avgustinaki et al (2004), the majority of patients with NGU associated with HSV types 1 and 2 have no history of erosive lesions of the genital organs characteristic of genital herpes.
Many experts recommend testing for HSV as a standard test for urethral discharge syndrome.
Adenoviruses have also been isolated from the urogenital tract of men. Urethritis associated with adenoviruses is most often accompanied by the appearance of erosive and ulcerative lesions of the genitals, conjunctivitis, and “cold” symptoms. In addition, clinical features of urethritis include the presence of meatitis and symptoms of dysuria (CS Bradshaw et al., 2002). The first reports appeared in 1985 - during an immunofluorescence study, the authors found adenoviruses in 11.47% of patients (S. Anghelescu et al., 1985). Epidemiological studies in recent years indicate that the isolation of adenoviruses occurs more often in the autumn-winter period and occurs in 0.33–4% of patients examined for STIs (PD Swenson et al., 1995; CS Bradshaw et al., 2006).
All patients had a history of unprotected orogenital contact.
Treatment of patients with NGU
To develop an individual treatment plan, it is important to take into account factors such as the type of pathogen, duration of infection, history of previous treatment, and the presence of concomitant pathogenic and opportunistic flora.
Etiotropic treatment of NGU is based on the use of antibacterial drugs of various groups that are active against the main pathogens of NGU - chlamydia and mycoplasmas. The activity of drugs against any infection is determined by the minimum inhibitory concentration (MIC) in in vitro studies. BMD indicators, as a rule, correlate with the results of clinical cure. Antibiotics with the lowest MIC are considered the optimal drugs, but one should remember the importance of parameters such as bioavailability, the ability to create high interstitial and intracellular concentrations, tolerability and treatment compliance.
To select an adequate treatment regimen in specific cases, laboratory determination of the sensitivity of isolated cultures to various antibiotics is recommended. But this mainly concerns the identified saprophytic flora. Thus, many authors note the ability of mycoplasmas to quickly acquire resistance to antibacterial drugs when they are passaged in vitro. Therefore, testing of strains freshly isolated from diseased individuals is necessary. Another difficulty is that when detecting chlamydia and mycoplasmas, sensitivity to antibiotics in vitro does not necessarily correlate with a positive effect in vivo. This may be related to the pharmacokinetics of the drugs. All these factors must be taken into account when prescribing etiotropic therapy, which in many cases can be part of combination therapy, especially for mixed infections.
The European guidelines for the management of patients with urethritis (2001) contain recommendations according to which NGU should be treated according to basic and alternative regimens.
Basic schemes:
- doxycycline - 100 mg 2 times a day for 7 days;
- azithromycin - 1.0 g orally, once.
Alternative schemes:
- erythromycin - 500 mg 4 times a day for 7 days or 500 mg 2 times a day for 14 days;
- ofloxacin - 200 mg 2 times a day or 400 mg 1 time a day, for 7 days;
- tetracycline - 500 mg 4 times a day for 7 days.
From the above schemes it is clear that the main antibiotics recommended for the treatment of NGU are tetracycline drugs, macrolides and fluoroquinolones.
There are no specially developed official domestic guidelines for the treatment of NGU yet, but there are recommendations for the treatment of certain types of NGU - trichomonas, chlamydial and mycoplasma infections. If we summarize the recommendations set out in the main domestic guidelines (“Federal Guidelines for the Use of Medicines”, “Rational Pharmacotherapy of Skin Diseases and Sexually Transmitted Infections” (edited by Academician of the Russian Academy of Medical Sciences, Professor A. A. Kubanova), “Methodological Materials on the diagnosis and treatment of the most common sexually transmitted infections and skin diseases (protocols for patient management), published by TsNIKVI), then the following schemes for the etiotropic treatment of NGU can be presented.
Tetracycline antibiotics. Main drugs:
- doxycycline - 100 mg 2 times a day for at least 7-14 days. The first dose when taking the drug is 200 mg.
Alternative drugs:
- tetracycline - 500 mg 4 times a day for 7–14 days;
- metacycline - 300 mg 4 times a day for 7–14 days.
Macrolides. Main drugs:
- azithromycin - a single dose of 1.0 g or 250 mg once a day for 6 days. The drug is taken 1 hour before meals or 2 hours after meals;
- josamycin - 500 mg 2 times a day for 7–14 days.
Alternative drugs:
- erythromycin - 500 mg 4 times a day for 7–14 days;
- roxithromycin - 150 mg 2 times a day for 7–14 days;
- clarithromycin - 250 mg 2 times a day for 7–14 days;
- midecamycin - 400 mg 3 times a day for 7–14 days.
Fluoroquinolones:
- ofloxacin - 200–300 mg 2 times a day for 7–14 days;
- sparfloxacin - 200 mg 1 time per day for 10 days (on the first day the dose is doubled);
- levofloxacin - 500 mg 1 time per day for 10 days;
- pefloxacin - 600 mg 1 time per day for 7-14 days.
Tetracycline drugs are the most common drugs for the etiotropic treatment of patients with NGU. Despite the fact that doxycycline has been used in the treatment of various pathologies for several decades, its activity against the main pathogens of NGU remains high (D. Kilic et al., 2004).
That is why, according to all the recommendations mentioned above, the drug of choice for the treatment of NGU is doxycycline. The advantage of using doxycycline is its fairly high effectiveness and relatively low cost of treatment. Doxycycline has higher bioavailability, a longer half-life, and is better tolerated than tetracycline. In addition, when using doxycycline, unlike other tetracyclines, there is no need to follow a diet designed to take into account the possibility of tetracyclines binding to Ca2+ ions. The most common side effects when taking tetracycline drugs are nausea, vomiting, diarrhea, and allergic reactions. These reactions are significantly less severe when using doxycycline monohydrate rather than traditional doxycycline hydrochloride. Doxycycline monohydrate (Unidox Solutab) is available in a unique dosage form of tablets that can be taken orally whole, can be divided into pieces or chewed, and can be dissolved in water to form a suspension syrup (when dissolved in 20 ml of water) or a suspension solution ( when dissolved in 100 ml of water). The bioavailability of doxycycline monohydrate (Unidox Solutab) in this form is 95%, which practically corresponds to intravenous infusion.
During treatment with tetracycline drugs, patients should avoid exposure to sunlight due to the possibility of photosensitivity.
Antibiotics from the macrolide group are completely free of this side effect. All of the mentioned guidelines list the macrolide antibiotic azithromycin as the drug of choice for the treatment of NGU. This is facilitated by the unique pharmacokinetic characteristics of azithromycin: a long half-life, a high level of absorption and resistance to an acidic environment, the ability of this antibiotic to be transported by leukocytes to the site of inflammation, a high and prolonged concentration in tissues, as well as the ability to penetrate into cells. Due to the fact that a high therapeutic concentration of azithromycin in tissues is achieved after a single dose of a standard dose of antibiotic and remains in areas of inflammation for at least 7 days, with the advent of azithromycin, for the first time it became possible to effectively treat patients with chlamydial infection with a single oral dose of an antibiotic. Now many generics of azithromycin have appeared on the market (for example: azitrox, hemomycin, zitrolide). The original and most famous drug of azithromycin is sumamed, which has been used in the Russian Federation since the early 90s. last century.
The advantages of all modern macrolide antibiotics over the first antibiotic from this group, erythromycin, are higher efficiency, improved pharmacokinetics, good tolerability and lower frequency of dosing.
When taking macrolides, side effects from the gastrointestinal tract (nausea, vomiting, diarrhea) and liver (increased transaminase activity, cholestasis, jaundice), as well as allergic reactions, may occur.
Josamycin has the most favorable safety profile compared to other macrolides. The frequency of side effects when taking it does not exceed 2–4%. The drug does not have hepatotoxicity and almost does not change the normal intestinal microflora. In addition, this drug is approved for use in pregnant women in the Russian Federation. On our pharmaceutical market, josamycin is currently represented by the only drug vilprafen.
It is necessary to note that ureaplasmas are resistant to lincosamines, but sensitive to macrolides and streptogramins, and other mycoplasmas can be resistant to “old” macrolides (erythromycin, rovamycin, oleandomycin) and streptogramins, but are highly sensitive to the newest macrolides (josamycin, clarithromycin) and lincosamines.
The next group of drugs that are highly active against a wide range of NGU pathogens are fluoroquinolones. The only drugs in this group that the authors of modern guidelines recommend for the treatment of chlamydial infection are ofloxacin and its improved analogue, levofloxacin. Limitations in the use of fluoroquinolones for the treatment of chlamydial infection are due to the fact that, in comparison with antibiotics of other groups listed above, the percentage of relapses after therapy is too high.
Fluoroquinolones such as ofloxacin and sparfloxacin are especially highly effective for NGU caused by opportunistic saprophytic flora, since this flora is usually sensitive to these antibacterial drugs. Their “leading position” is due to the breadth of the antibacterial spectrum, high bactericidal activity, excellent pharmacokinetic characteristics (rapid absorption, high concentrations of the drug in tissues, cells, biological fluids), low toxicity. When treating with sparfloxacin, higher compliance is achieved, since the drug is taken only once a day. According to Yu. N. Perlamutrov and co-authors (2002), sparfloxacin is also highly effective against mycoplasma and ureaplasma infections.
Like tetracyclines, fluoroquinolones have a photosensitizing effect. In addition, drugs from the fluoroquinolone group are contraindicated in patients with impaired liver and kidney function. Adverse reactions after taking fluoroquinolones may include dyspepsia, nausea, vomiting, dizziness, allergic reactions, and tendonitis.
For the treatment of trichomonas NGU, metronidazole is recommended - 2 g orally as a single dose of 2.0 g for 3 days or 500 mg 2-3 times a day for 5-7 days. In addition to metronidazole, other nitroimidazoles can be used:
- ornidazole 1.5 g once 500 mg 2 times a day for 5 days (for complicated forms up to 10 days);
- tinidazole 2.0 g once for 3 days or 500 mg 2 times a day for 5 days;
- nimorazole 2.0 g once;
- secnidazole 2.0 g once or 250 mg 2 times a day for 10 days.
These drugs have slightly better pharmacokinetic parameters than metronidazole, which makes it possible to reduce dosages and frequency of use. However, these drugs do not have significant advantages over metronidazole, since if Trichomonas are resistant to metronidazole, they will be resistant to other nitroimidazoles.
Treatment carried out simultaneously in both sexual partners increases the effectiveness of treatment for NGU.
According to V.P. Kovalyk (2006), for the treatment of NGU, in the etiology of which the role of herpetic infection has been established, valacyclovir is effective in a course dose of 4.0 g (2.0 g at intervals of 12 hours). You can also use regimens that involve longer-term use of antiviral drugs:
- famciclovir - 250 mg 3 times a day for 5–10 days;
- acyclovir - 200 mg 5 times a day for 5–10 days;
- valacyclovir - 500 mg 2 times a day for 5–10 days.
If a patient with NGU, in addition to a herpetic infection, is also diagnosed with a bacterial one, then antiherpetic treatment is prescribed as an addition to antibacterial therapy. In cases where nothing other than viruses is found in urethritis, it is recommended to prescribe only antiviral therapy.
Despite proper antibiotic therapy for acute NGU, in 20–69% of cases, persistent or recurrent urethritis develops 1–2 weeks after treatment (M. Janier et al., 1995; PJ Horner et al., 1999; PJ Horner et al. , 2001).
The inflammatory process that continues after treatment of urethritis is one of the least studied clinical problems in venereology. Despite significant efforts being made to study this phenomenon, its etiology remains unclear.
Treatment of patients with chronic or recurrent NGU
Late presentation of patients with NGU and the spread of self-medication are the causes of chronicity and complicated course of the disease. Therapy of patients with long-term NGU is associated with significant difficulties in terms of achieving clinical effectiveness.
There is no single approach to the treatment of chronic urethritis. It is important to clinically and laboratory confirm the presence of such urethritis, since the proportion of patients with urethral symptoms but without urethritis is quite high.
The regimen proposed by the European Guidelines for the Treatment of Chronic Urethritis: erythromycin - 500 mg 4 times a day for 2 weeks plus metronidazole - 2 g once or 400 mg 2 times a day for 5 days.
According to KK Holmes et al (1998), about 2/3 of patients get rid of urethritis after undergoing this course of treatment, and the remaining 1/3 develop relapses or persistent urethritis.
Treatment regimens are also offered that differ in the longer duration of antibiotic use - from 3 to 6 weeks. However, they may not be effective for all patients. It is important for the doctor to try to find the reason for the ineffectiveness of antibacterial therapy and the recurrence or persistence of urethritis.
For example, with a long-term existence in the body, C. trachomatis can change its typical life cycle to an atypical one, when the normal life cycle of chlamydia is suspended. In this case, special relationships are formed in the system of macro- and microorganisms, allowing this system to coexist. This phenomenon is called latency and persistence. With this course of infection, there may be no clinical manifestations, as well as transmission of the infection from one sexual partner to another.
And antibacterial therapy at this stage may not be effective.
Chlamydia persistence requires a special approach to the patient. The use of antibiotics alone for this form of infection is, as a rule, not enough, since all antibiotics effective against chlamydia have a bacteriostatic effect and can only act on reproducing bacteria. When treating such conditions, combination therapy with antibiotics and immunocorrectors is usually recommended.
Our observations, based on the treatment of more than 1000 patients with persistent chlamydia, show that the most optimal in these cases is combination therapy based on a combination of antibiotics and immune drugs. For antibiotic therapy, standard courses and dosages of the antibiotics listed above are used for complicated infections. But it is advisable to start treatment with a course of immunotherapy. Based on our own research, we offer the following options for immunotherapy prior to antibiotics:
- polyoxidonium is prescribed 6 mg intramuscularly once a day; the first 2 injections daily, then 3 injections every other day, the rest - 2 times a week, for a total of 10 injections per course. After the 4th injection, a course of antibacterial therapy begins;
- Immunomax is prescribed 200 IU (1 bottle) intramuscularly once a day, 3 injections daily, then a break of 4 days and another 3 daily injections, a total of 6 injections per course. After the 3rd injection, a course of antibacterial therapy begins;
- interferon α-2β is prescribed in the form of rectal suppositories in two 5-day cycles with an interval of 2 weeks between them at a total dose of 10 million IU per course. After completion of immunotherapy, a course of antibacterial therapy is carried out. Moreover, the optimal course in this situation turned out to be a course of azithromycin, used according to the treatment regimen for complicated forms (1.0 g each on days 1, 7 and 14).
Combination therapy may also be effective for recurrent urethritis of mycoplasma etiology. The work of MMT Hadson et al (1998) reported on the importance of the immunological status of the patient during ureaplasma infection. The use of immunotropic therapy may be especially relevant if at least one course of antimicrobial treatment is ineffective.
Our own studies have shown that when choosing immunotropic therapy, the drug Immunomax demonstrated particularly high effectiveness. This drug belongs to the group of immunomodulators, and is indicated for the correction of weakened immunity, treatment and prevention of viral and bacterial infections. The regimen for using Immunomax does not differ from the method of its use for recurrent chlamydial infection.
Thus, adequate, i.e. based on the results of clinical and laboratory studies and existing recommendations, antibacterial therapy can achieve a positive effect in NGU.
M. A. Gomberg , Doctor of Medical Sciences, Professor A. M. Solovyov , Candidate of Medical Sciences, Associate Professor V. P. Kovalyk , Candidate of Medical Sciences TsNIKVI, MGMSU, Moscow
Patient preparation rules
In men: from the urethra. Standard conditions:
During the working day DC.
Important:
During the day before collecting the material, do not use topical medications and refrain from urinating for 2 hours.
Possible:
deviations from standard conditions in agreement with the doctor.
You can add this study to your cart on this page
Carrying out the smear procedure
A special probe or tampon is inserted into the urethral canal to a depth of about 3 centimeters, and a smear is taken. In this case, a man may experience discomfort and pain in the head of the penis, which may persist for some time after the procedure for taking material for analysis. If the pain does not go away, or purulent or bloody discharge from the urethra appears, you should immediately consult a doctor.
If necessary, before taking a smear, the doctor may prescribe a massage of the prostate gland through the anus or urethra using a special probe.
The following biological fluids are used as material for sowing:
- Urine;
- Ejaculate;
- Prostate secretion;
- Discharge from the male urethra.
The resulting materials are placed in a nutrient medium. After a week, the results of the urethral culture tank will be ready. In addition to the type of microorganism, laboratory assistants will identify those active medicinal substances to which this infectious agent is sensitive.
Interpretation:
- leukocytes (neutrophils and lymphocytes): fresh urethritis or exacerbation of chronic urethritis; eosinophils (over 5-10%) - allergic urethritis; epithelial cells (with a small number of leukocytes): chronic urethritis with epithelial metaplasia (desquamative urethritis) or urethral leukoplakia; red blood cells ( with leukocytes and epithelial cells): traumatic urethritis, urethral tumor, crystalluria, ulceration of the mucous membrane, etc.; lipoid granules: prostatorrhea; spermatozoa: spermatorrhea; mucus without formed elements: urethrorrhea; accumulations of small polymorphic rods on epithelial cells (key cells) with a small number of polynuclear neutrophils: urethritis caused by Corynebacterium vaginale; key cells, bacteria, single polynuclear neutrophils: bacterorrhea.
Sample result (PDF)