Detailed description of the study
Prenatal (antenatal) screening is a comprehensive medical study (laboratory and instrumental) aimed at identifying a group at risk for the development of chromosomal abnormalities of the fetus during pregnancy. The screening results allow you to decide on the need for a more detailed examination (invasive diagnostics, genetic consultation).
Laboratory Gemotest LLC performs prenatal screening of the first trimester of pregnancy using PRISCA (PrenatalRiskCalculation) software from the manufacturer Siemens Healthcare Global. To calculate the biochemical risk of chromosomal abnormalities, the program uses indicators of biochemical blood markers, anthropometric data of the fetus based on ultrasound results, as well as the pregnant woman’s personal data.
Prenatal screening in the first trimester:
- It is carried out during 11-13 weeks of pregnancy;
- Biochemical (serum) markers: free β-hCG and PAPP (Pregnancy Associated Protein A);
- Ultrasound data of the first trimester indicating the date of execution: coccygeal-parietal size (CTR) for calculating the gestational age, nuchal translucency thickness (NVP), visualization of the nasal bone;
- Personal details of the pregnant woman: age, weight, race, bad habits (smoking);
- History of the pregnant woman: number of previous pregnancies, presence of multiple pregnancies, in vitro fertilization, presence of diseases (insulin-dependent diabetes mellitus).
To correctly calculate the risk of developing chromosomal abnormalities, the laboratory must have accurate data on the gestational age, ultrasound data (CTR, TVP and visualization of the nasal bone for the first trimester) and complete information about all factors necessary for screening (indicated in the referral form). The gestational age can be calculated by the date of the last menstruation (LMP), the date of conception (estimated period).
For prenatal screening, it is recommended to use a more accurate and informative method - calculating the gestational age according to ultrasound data (CTR and BPR). Due to the existence of several statistical methods for determining the gestational age based on fetal ultrasound data, the calculation results performed using the PRISCA software may differ slightly from the gestational age determined by the ultrasound doctor (range up to 5 days in the first trimester).
The computer program for calculating the analysis results PRISCA allows you to:
- calculate the probability of various risks of fetal pathology
- take into account the patient’s individual data
- consider factors influencing the detection of abnormal levels of biochemical markers.
Screening parameters in the 1st trimester (11-14 weeks):
- Ultrasound measurement of CTP + TVP (coccygeal-parietal size should be in the range of 38-84 mm; measurement of the cervical fold is important when diagnosing Down Syndrome and is increased in pathology (normally about 1 mm)
- Immunochemical determination of the free beta subunit of human chorionic gonadotropin and pregnancy-associated protein A (PAPP-A).
Features of risk calculation:
- Risk calculation depends on the accuracy of the data provided for analysis
- risk calculation is the result of statistical data processing
- Results must be confirmed (or excluded) by cytogenetic studies.
1. Pregnancy associated protein A (PAPP-A) is a plasma protein produced in large quantities by placental fibroblasts during pregnancy. Detected in the mother's bloodstream. Its concentration increases throughout pregnancy. This protein ensures the full growth and development of the placenta. With a chromosomal abnormality with fetal malformations, the concentration of PAPP-A in the blood decreases significantly from the 8th to the 14th week of pregnancy. The most dramatic decrease is observed with trisomies on the 21st, 18th and 13th chromosomes. In Down syndrome, the PAPP-A indicator is an order of magnitude lower than in the norm. The level of PAPP-A in the mother's blood serum drops even more sharply if the fetus has a genetic pathology with multiple malformations - Cornelia de Lange syndrome.
2. Free beta subunit of human chorionic gonadotropin is a hormone that is produced in the fetal membrane of the human embryo. It is an important indicator of the development of pregnancy and its deviations. According to its chemical structure, it is a combination of protein and complex carbohydrates. There are several variants, or isoforms, of hCG, including free, or unbound, beta-hCG. An increase in the concentration of free beta-hCG in pregnant women in the first trimester of pregnancy may indicate a risk of developing trisomy 21 (Down syndrome) in the fetus. The risk of developing other fetal aneuploidies also increases - conditions in which the body's cells contain an altered number of chromosomes that is not a multiple of the normal haploid set. A decrease in hormone concentration may indicate the development of other chromosomal abnormalities in the fetus, in particular Edwards syndrome, trisomy 18.
In accordance with the order of the Ministry of Health of the Russian Federation dated November 1, 2012 No. 572n. The procedure for providing medical care in the field of “obstetrics and gynecology (except for the use of assisted reproductive technologies)”: it is necessary to conduct prenatal screening in the first trimester at 10-13+6 weeks of pregnancy.
Attention! Taking medications can affect the results of prenatal screening!
Multiple pregnancy. Lecture for doctors
Lecture for doctors “Multiple pregnancy”. The lecture for doctors is given by S. M. Dyakova, obstetrician-gynecologist, teacher - total work experience 47 years
Part 1. Multiple pregnancy
Part 2. Multiple pregnancy
Part 3. Multiple pregnancy
Additional material
Definition, brief historical background
Multiple pregnancy is a special condition in a woman’s life, which is uncharacteristic for humans, and in terms of the number of complications, it is an increased risk factor for both the fetus and the mother’s body.
A multiple pregnancy is a pregnancy in which two or more fetuses develop simultaneously in a woman’s body.
Births of two or more fetuses are called multiple births.
Children born as a result of multiple pregnancies are called twins.
In 1895, the French biologist D. Ellin formulated the law of the birth of twins: one twin appears in 85 single births, one triplet - in 85 twins, one quadruplets - in 85 triplets, etc. In other words, one triplet occurs approximately in 7000, one quadruplets - by 680,000, and one gear - by 4,712,000,000 births.
Multiple pregnancies occur in 0.4-1.6% of cases. Currently, there is a trend toward an increase in the incidence of twin births.
Factors influencing the occurrence of multiple pregnancies
Heredity. You are more likely to expect twins if the father or mother has already had multiple pregnancies in the family. This is the most proven or significant factor. The greatest likelihood is for women who have this predisposition, mainly through the female line. Of great importance is the combination of the genes of both partners (the homogeneity of their composition) and the patterns of inheritance that are observed after a generation or two, and most often, in the lateral branches of the clan (inheritance by cousins). This means that twins are more common in families where the mother or father, or both parents, have twin siblings. The likelihood of repeating twins increases over a generation, that is, if a grandmother once had twins, then her granddaughter also increases the likelihood of repeating a multiple pregnancy.
The mother's age —between 35 and 40—also increases the likelihood of having more than one child.
Very young mothers aged about 18 have minimal chances. Their probability of having twins is only 0.27%. By age 25, the probability increases by more than 2 times (0.62%). At the age of 30, the initial chance increases by 3 times and is 0.90%. This figure reaches its maximum by the age of 35, increasing by 5.5 times (1.48%), and by the age of 40, the probability of giving birth to twins in a woman begins to decrease (at 40 years old - to 1.25%, at 45 - to 0.73 %). This is explained by the fact that before the onset of menopause, a “last surge” of hormones occurs in the female body, so late pregnancies are often multiple. By the end of the childbearing period (at about 48 years), the chances of giving birth to twins are almost equal to those of an 18-year-old girl (0.30%).
Repeated births. With each subsequent birth, the chances of having twins increase (after the second birth - two times, after the fifth - five times). If the mother has already given birth to fraternal twins, then the likelihood of repeating the success doubles. The latter fact is explained by the fact that the body of a woman who has once conceived twins is capable of producing several eggs during the period of ovulation.
Nationality (a little-studied phenomenon) . Depending on a woman’s nationality, the chance of having twins can vary by more than 10 times. Most often, twins appear in black women (from 4.5% in Nigeria), followed by representatives of the white race, and Asian women close the list (up to 0.4% in China).
Time of conception. The production of the hormone gonadotropin, which stimulates the ovary, is influenced by the length of daylight hours, therefore (and this is confirmed by statistics), there is a greater chance of conceiving twins in the spring.
Taking hormonal medications , which are used both to treat infertility and to protect against unwanted pregnancy. Women who used birth control (for at least 6 months) and became pregnant within 2 months of stopping were twice as likely to have twins than others.
Artificial insemination . Since the mid-1980s, the introduction of infertility treatments such as in vitro fertilization and embryo transfer (IVF and ET) has caused a sharp increase in the incidence of multiple pregnancies. Multiple pregnancy after IVF treatment is 25-30% (that is, in every 3-4 cases). Successfully developing IVF technologies have led to the fact that pregnancy with triplets and quadruplets is no longer a rarity, since several fertilized eggs are implanted into the uterus at once in the hope that one or two fetuses will develop successfully. If more than three fruits survive, then quantity comes at the expense of quality - such children may not be viable at all.
Currently, up to 50% of the structure of multiple pregnancies are made up of pregnancies after IVF and ET, as well as stimulation of superovulation.
Anomalies in the development of the uterus (bicornuate, septum in the uterus) are the cause of an increase in the frequency of twins. With developmental anomalies, more often than with the normal structure of the uterus, two or more eggs mature simultaneously and can be fertilized.
Much less frequently cited reasons for multiple pregnancies are the state of the environment, prolonged sexual abstinence, and the woman’s social status (it is estimated that in lower social classes, for some reason, twins are born more often). Malnutrition or very strict diets are known to reduce the incidence.
However, all these factors reduce or increase the possibility of having only fraternal twins! The probability of being born identical is not associated with any hereditary or external factors and is constant: on average 3 per 1000 pregnancies, that is, 0.3%.
Pathogenesis of multiple pregnancy
There are two types of twins: monozygotic (identical, identical) - from one fertilized egg as a result of atypical splitting of the egg into two (three, four...) parts and dizygotic (fraternal or fraternal, non-identical) - twins developing from two or more simultaneously fertilized eggs (Fig. 1).
Rice. 1. Formation of fraternal and identical twins
Identical twins are genetically identical, always of the same sex, have the same blood type, are very similar to each other in appearance, character, and even often suffer from the same diseases at the same time.
Fraternal twins, from a geneticist's point of view, are ordinary brothers and sisters. They can be same-sex or different-sex, blood type can be the same or different. Opposite-sex twins are always fraternal.
The ratio of fraternal to identical twins is 10:1.
The embryo developing in the uterus is surrounded by the amnion, an internal embryonic membrane that forms a fluid-filled cavity that protects the fetus from mechanical damage and provides an aqueous environment for its development; chorion - the outer embryonic membrane, covered on the outside with villi, which grow into the mucous membrane of the uterus, forming the placenta.
The origin of fraternal twins (fraternal twins) may be as follows:
- simultaneous maturation and ovulation of two or more follicles in one ovary (ovulatio uniovarialis);
- maturation of two or more follicles and ovulation in both ovaries (ovulatio biovarialis);
- fertilization of two or more eggs matured in one follicle (ovulatio unifollicularis).
In dizygotic twins, both embryonic membranes are always different, although it happens that the placentas grow together into one (if two fertilized eggs are implanted into the uterine wall very close to each other).
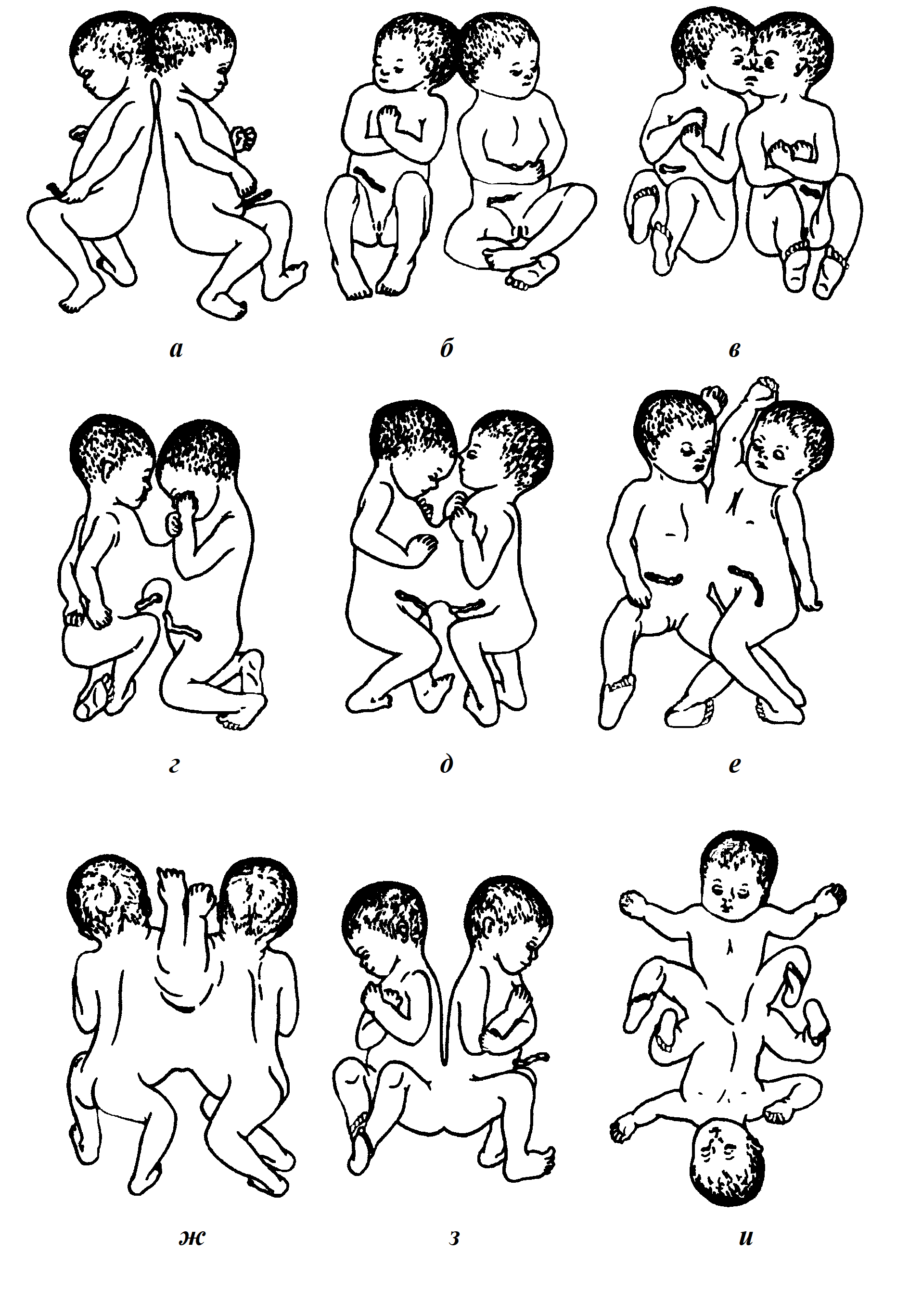
Identical twins can be biamniotic or monoamniotic.
The origin of identical (monozygotic) twins is associated with the division of a single embryonic rudiment into two or more parts:
1. If separation occurred in the first three days after fertilization, that is, within 72 hours, a bichorionic biamniotic pregnancy develops (Fig. 2a, b).
2. If separation occurs on days 4-8, at the morula stage (before the appearance of the amniotic sac), pregnancy develops with a monochorionic biamniotic placenta (Fig. 2c).
3. If splitting occurs on days 9-12 (1% of all monozygotic twins), when the amniotic sac and chorion have already formed, and the twins develop in a common amniotic membrane and with a common placenta, it is a monochorionic monoamniotic pregnancy (Fig. 2d).
4. After 15 days, complete separation of the embryonic rudiments is impossible and conjoined twins develop.
In most cases of identical twins, separation of the embryonic buds must occur before the 8th day (monochorionic biamniotic placenta).
Only monozygotic twins can develop in the same amniotic sac with a common chorion and placenta.
Only monozygotic twins can develop in different amniotic membranes, but in the same chorion.
Identical and fraternal twins can develop in different amnions and different chorions.
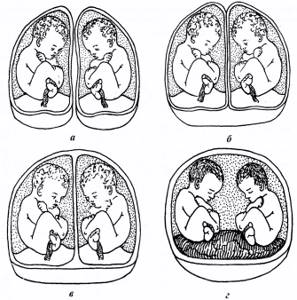
Rice. 2. Formation of membranes and placenta in twins:
a - two placentas, two amnions, two chorions (dichorionic/diamnial twins); b - one placenta, two amnions, two chorions (dichorionic/diamnial twins); c — one placenta, two amnions, one chorion (monochorionic/diamnionic twins); d - one placenta, one amnion, one chorion (monochorionic/monoamnial twins)
Conclusion. The presence of one chorion with one or two (several) amniotic membranes indisputably indicates that we are dealing with identical twins. If there is more than one chorion, only special tests can give an accurate answer - from simple determination of blood group and Rh factor to more complex genetic tests - typing of HLA histocompatibility antigens, DNA analysis.
There are theories of “super-generation” and “super-fertilization”. Superfertilization is the fertilization of eggs from different ovulatory periods, that is, the onset of a new pregnancy in the presence of an existing one. Superfertilization is the fertilization of two or more eggs released during one ovulation by the seminal fluid of different fathers.
Triplets can be identical or fraternal, and it is also possible to have two identical and one single fetus. Quadruplets can be identical, fraternal, or twins; triplets and one single fetus. Twins after IVF are always fraternal, often of different sexes, each with their own character. According to some psychologists, an identical genetic code leaves an imprint on the relationship of monozygotic twins with each other and with the surrounding reality, which requires a special attitude towards them and special efforts aimed at raising them as independent individuals, and not as a single indivisible and self-sufficient tandem, in largely isolated from the outside world.
The phenomenon of twins has long attracted the close attention of biologists and doctors.
Francis Galton put the twin method on a “scientific track”: in 1876, he published the article “The History of Twins as a Criterion for the Effect of Heredity and Environment.”
Galton developed the so-called “method of concordance,” that is, comparing identical twins with same-sex fraternal twins, as well as identical twins raised together with identical twins who, for one reason or another, grew up separately from each other.
American psychologist Thomas Bouchard in the 80s of the twentieth century studied about 30 pairs of identical twins separated at an early age. The most striking was the fate of the brothers Oscar and Jack. The twins were born in 1932. The parents separated. Oscar’s mother took him to Germany, where he “fell ill” with Nazism, and as soon as age allowed, he joined the Hitler Youth. Jack spent his childhood and youth in Palestine and the Caribbean islands. His father raised him in the traditions of Judaism. It would seem that “heredity is resting,” but at the age of forty the brothers met. It turned out that they have a lot in common: both wear the same trimmed mustache, both have weakened vision with age, and even their glasses are almost the same. Clothes preferences are also remarkably similar. The brothers love the same food and behave similarly in the family.
In Ethiopia, on June 5, 1989, Kadija Abdella gave birth to a boy. More than a week passed, the woman managed to almost recover from childbirth, when suddenly on June 13, contractions suddenly began and she gave birth to a girl, who turned out to be 8 days younger than her brother.
Canadian twins Alice and Emma Rhodes were born 39 days apart. After a premature birth, which resulted in the birth of 500g Alice, doctors managed to stop labor and her little sister was born five weeks later.
The Berlin Krug twins have different birth years recorded in their metrics. At the same time, Anton Krug was only 15 minutes ahead of his younger sister Leila. Everything is explained simply: Anton was born on December 31, 1997, shortly before midnight, and Leila was born on January 1, 1998. But the Americans from Massachusetts, Aaron and Luke Hegenberger, who were born 8 minutes apart, are separated by a millennium: the eldest was born on December 31, 2000, the youngest on January 1, 2001.
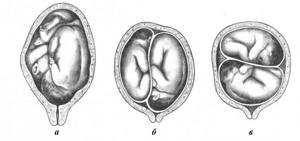
Twins joined together in the mother's womb are called Siamese.
Rice. 3. Types of conjoined twins: a, b, c - craniopagus; d, e, f, g - thoracopagus; h, i - pygopagus
The term is associated with a pair of Chinese twins born in 1811 in Thailand (then called Siam). The boys, whom their parents named Chang - "left" and Eng - "right", were fused at the solar plexus, had a common navel and, apparently, one liver between them. In their youth they worked as peddlers, and by the age of 18 they moved to America, where they began touring with incredible success. They married sisters, had more than 20 children, and died at the age of 63.
Another pair of famous Siamese twins, the Blazek sisters, were born in 1878. The sisters became musicians - a violinist and a harpist, one of them gave birth to a child.
The world's first successful operation to separate conjoined twins was performed in 1952 by Dr. Jacques Geller (USA). Now such operations are being performed more and more often, and twins conjoined with their bodies have an increasing chance of a full independent life.
Depending on the location of the connection, they are distinguished (Fig. 3):
- craniopagus (in the head area);
- thoracopagus (in the thoracic region);
- pygopagus (in the lumbar region and perineum).
Diagnosis of multiple pregnancy
Diagnosing multiple pregnancy often presents significant difficulties, especially in the first half of pregnancy. In the second half, towards the end of pregnancy, recognition of twins (triplets) becomes easier. However, diagnostic errors can occur during examinations at the end of pregnancy and even during childbirth.
When recognizing a multiple pregnancy, the following signs are taken into account:
1. The uterus enlarges faster, and its size does not correspond to the duration of pregnancy. This discrepancy is recorded from 14-16 weeks. The fundus of the uterus is usually high, especially at the end of pregnancy; the abdominal circumference during this period reaches 100 cm or more.
2. If the twins are in a longitudinal position, then a longitudinal depression is formed on the anterior surface of the uterus; in the transverse position of both fruits, the depression is located horizontally.
3. The uterus takes on a saddle-shaped shape (its corners protrude with large parts of the fruit, and a depression is formed in the bottom area).
4. Small size of the presenting part compared to the volume of the uterus.
5. Identification of large parts of the fetus in different parts of the abdomen.
6. Identification of three or more large parts of the fetus in the uterus during an obstetric examination (for example, two heads and one pelvic end).
7. Early sensation of fetal movement - from 15-16 weeks of pregnancy.
8. Feeling of fetal movement in different places.
9. Two points of a distinct fetal heartbeat in different places of the uterus with a zone of silence between them, and the difference in heart rate is at least 10 beats (Fig. 4).
10. Excessive weight gain in a woman from 14-16 weeks in the absence of clinical signs of gestosis in pregnant women.
11. Increased tone of the uterus.
12. Ultrasound allows you to diagnose multiple pregnancies, starting from the first half. Reliable signs of multiple pregnancy are detected at very early stages of pregnancy - at 3-4 weeks.
13. Cardiotocography, phono- and electrocardiography are also used for diagnosis, with the help of which it is possible to record the heart sounds of twins at 20-22 weeks of pregnancy and even earlier.
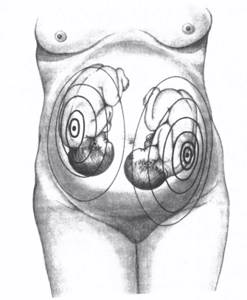
Rice. 4. Two focuses of listening to heartbeats in fetuses with twins
In most cases, recognition of multiple pregnancies is possible with careful examination using publicly available clinical methods. For diagnosis, the presence of several signs of multiple pregnancy is necessary, of which the most important are palpation (three large parts) and auscultation (heartbeat of two fetuses).
Position of fetuses in the uterus during twins
The position of the fetuses can be accurately recognized by ultrasound (Fig. 5).
In 88%, both twins are in a longitudinal position and occupy one the right and the other the left half of the uterus.
In 45%, both fetuses are presented head-on.
Next in frequency are the following combinations:
- one fetus in a cephalic presentation, the other in a pelvic presentation (43%);
- both fetuses in breech presentation (6%);
- one fruit in a longitudinal position, the other in a transverse position (5.5%);
- both fetuses in a transverse position (0.5%).
Rice. 5. Position of the fetuses in the uterus during twins:
a - cephalic presentation of both fetuses; b - cephalic presentation of one fetus and pelvic presentation of the second; c - transverse position of both fruits
Course and management of multiple pregnancy
A pregnant woman should be under close medical supervision. Immediately after multiple pregnancy is detected, it is necessary to prescribe a gentle regime and a special diet, which will ensure the increased need of the pregnant woman’s body for proteins, fats, carbohydrates, vitamins and microelements, prevent the development of iron deficiency anemia, and minimize the possibility of having children with low body weight. A pregnant woman should pay special attention to her diet, especially in the 1st trimester. Each child requires approximately 300-400 kk/day. In this case, vitamins are also prescribed in double doses. If for a singleton pregnancy the optimal weight gain is 12-13 kg, then for a multiple pregnancy it is at least 18-20 kg.
A pregnant woman should visit an obstetrician-gynecologist every 2 weeks, and weekly in the third trimester. Pregnant women are offered planned hospitalization at 29-32 weeks and at 36 weeks to monitor the condition of the woman and fetus, prevent complications and carry out the necessary treatment, determine the optimal period and method of delivery. In some cases, a pregnant woman has to remain in bed for several months.
After 20 weeks, expectant mothers are recommended to rest at least 4-6 hours during the daytime, then up to 8 hours a day. After the 20th week, a woman is recommended to stop active sports, work, and sex life.
It is necessary to carefully monitor the condition of the fetus and the function of the fetoplacental complex. Ultrasound scanning, Dopplerography, and cardiotocography play an important role in assessing the condition of the fetus, the structure and function of the placenta.
After 30-32 weeks, CTG and echographic assessment of the functional state of the fetoplacental system should be carried out weekly. It is advisable to conduct Doppler examination of blood flow in each fetus separately.
If genetically determined developmental anomalies, hemolytic disease are suspected, and to determine the maturity of the fetal lungs by the ratio of lecithin-sphingomyelin levels (which reflects the production of surfactant), amniotic fluid from each fetal sac should be examined under echographic control.
It should be noted that the higher the order of multiple pregnancy, the higher the risk of complications.
If a woman does not want to give birth to more than two children or if pathology is detected in the early stages of one of the twins, selective termination of pregnancy is possible. The most successful termination of pregnancy is completed when the embryo is reduced, having a small size, located closer to the internal os, with a small size of the fertilized egg, conveniently located for this procedure. Reduction is carried out under echographic control via transvaginal access within 7-10 weeks. During the operation, no more than 2 embryos are reduced.
Complications during multiple pregnancy:
1. In the 1st trimester, in 15-20%, the phenomenon of “the death of one of the fertilized eggs” is observed. Therefore, despite the diagnosis of twins or triplets, there is a chance that only one fetus will develop.
2. Fatigue, shortness of breath, increased urination and constipation appear earlier than in a normal singleton pregnancy.
3. An increase in the load on the cardiovascular system can lead to disruption of its function and decompensation. A pronounced functional strain of the hemodynamic state was established. At the same time, the volume of circulating blood is increased by approximately 20% compared to a singleton pregnancy, there is an increase in the number of red blood cells, cardiac output, diastolic blood pressure, and renal glomerular filtration rate.
4. The appearance of iron deficiency anemia in the mother from 20-24 weeks of pregnancy is associated with an increase in the mass of placental tissue and an increase in the content of placental factors that cause anemia; an increase in intravascular volume, resulting in a decrease in the level of hemoglobin and hematocrit.
5. Preeclampsia occurs 4 times more often.
6. Dilatation of the veins of the lower extremities.
7. Polyhydramnios of one or both fetuses. In some cases, polyhydramnios in one cavity may be accompanied by oligohydramnios in the other.
8. Fetoplacental insufficiency.
9. Abnormal location of the placenta.
10. High frequency of premature termination of pregnancy: with twins - 26-56%, with triplets - 66-97%, with quadruples - more than 90%. According to the traditionally widespread hypothesis, the main reason for the premature development of labor is overstretching of the muscle fibers of the uterus due to the large volume of fetuses. Almost 2/3 of newborns who die after multiple births are premature.
11. Dissociated type of development of twins, when one fetus is larger than the other. The difference in weight can even be 1000-1500 g. Such developmental disorders arise due to improper blood circulation in the placenta or umbilical cord, that is, blood flows better to one fetus and worse to another. The most pronounced degree of dissociated development is observed in the feto-fetal blood transfusion syndrome, when identical twins with the same placenta (monochorionic) feed as follows: one child from the other. One becomes the donor, and the second becomes the recipient. In this case, both lives are in danger.
When feto-fetal hemotransfusion syndrome is established abroad, the anastomoses are separated using a laser, and both children continue to develop normally.
12. Low birth weight of newborns. In 40-60% of cases when twins are born, the body weight of the children is less than 2500 g. Usually, the difference in body weight between both twins is small and is about 200-300 g.
13. Functional immaturity of the fetus, more often occurring with triplets, quadruplets, etc.
14. Intrauterine death of one fetus.
15. In multiple pregnancies, congenital malformations are more common: 2.7% - with twins, 6.1% - with triplets. The most common malformations among twins have the following localization: the cardiovascular system, gastrointestinal tract, less often the central nervous system, lungs, musculoskeletal and genitourinary systems.
There are also defects that are characteristic only of multiple pregnancies - undivided twins. The frequency of this defect is 1 case in 50,000-100,000 births.
Course of labor during multiple pregnancy
The least number of perinatal complications and the most favorable period of birth for twins is 36-38 weeks of pregnancy, for triplets - 34-36 weeks.
The course of labor may be normal. The pharynx opens, one amniotic sac ruptures, and the first fetus is born. After the birth of the first fetus, there is a pause in labor lasting from 15 minutes to 1 hour (sometimes more). At this time, muscle retraction increases, and the uterus adapts to its reduced size. Then labor resumes, the second amniotic sac ruptures and the second fetus is born. The time interval between the birth of the first and second twins in most cases is 20-30 minutes. After the birth of the second fetus, both placenta are separated from the wall of the uterus and simultaneously expelled from the birth canal.
However, such a successful course of labor is not always observed.
Complications during childbirth and the postpartum period:
1. Premature and early rupture of amniotic fluid (25-30%) of the first fetus is dangerous due to the possibility of microbes entering the uterine cavity and causing fetal asphyxia. Untimely disruption of the integrity of the fetal bladder leads to a slowdown in the process of cervical effacement and opening of the pharynx.
2. Weakness of labor associated with the inability of the uterus to vigorously contract due to overstretched muscles. Overstretching of the uterine walls is caused by the presence in its cavity of two fetuses with placentas and amniotic fluid; This is also facilitated by polyhydramnios, which is quite often observed during multiple pregnancies. The reason for the weakness of labor may be the exclusion from active contractions of a large area of the myometrium, where two or one large placenta is located.
3. Due to the weakness of labor forces, the period of dilatation can be protracted, the woman in labor becomes tired, which, in turn, inhibits labor activity. The period of exile often drags on. The duration of labor in a multiple pregnancy is longer than in a single birth.
4. After the birth of the first fetus, premature abruption of the placenta of both the born and the unborn twin (or the common placenta) may occur. In this case, severe bleeding occurs, threatening the health of the mother in labor, and asphyxia of the intrauterine fetus. Premature placental abruption after the birth of the first fetus occurs in 3-4% (up to 7%) of twin births.
5. Delayed rupture of the membranes of the second fetus. If in such cases the amniotic sac is not opened artificially, the birth of the second fetus is delayed for many hours.
6. After the birth of the first fetus, the process of muscle retraction may not be active enough, because the uterine cavity does not shrink immediately. In this regard, conditions arise that determine an increase in the mobility of the fetus and promote its self-rotation in the uterine cavity. The fruit, which was in a transverse position, can move into a longitudinal position; There is also a transition from longitudinal to transverse, in which childbirth without the use of obstetric operations is impossible.
7. A rare, but extremely serious complication is the simultaneous entry of the heads of both twins into the pelvis, which causes a so-called collision, or cohesion of the twins (Fig. 6). This complication occurs when the first baby is born in a breech position and the second in a breech position.
head (other clutch options are possible). When twins are conjoined, obstetric surgery must be resorted to.
8. With twins, the stillbirth rate is significantly higher than with a single birth. This depends on the higher frequency of premature births and functional immaturity of premature fetuses, on complications that often arise with twins and lead to intrauterine asphyxia; Surgical interventions are also important.
9. In the afterbirth period, bleeding occurs due to incomplete detachment or due to retention of the detached placenta in the uterus. Disruption of the process of placental abruption and discharge of the placenta is facilitated by reduced contractile activity of the uterus.
10. In the postpartum period, a slowdown in uterine involution is observed; postpartum diseases occur more often than after childbirth with one fetus. This depends not only on a slower involution, but also on a higher incidence of complications and surgical interventions during childbirth.
The prognosis for childbirth with multiple pregnancies is less favorable than with a single fetus.

Rice. 6. Fetal collision in twins
Management of childbirth and the postpartum period
Frequent complications during childbirth give reason to consider them in multiple pregnancies to be borderline between physiological and pathological.
Managing childbirth requires a lot of attention and patience. It is necessary to carefully monitor the condition of the mother and fetus, the dynamics of labor.
If labor is weak, its timely correction with medications is necessary.
If there is polyhydramnios, amniotomy is indicated when the cervix is opened by 3-4 cm. The water is released slowly, since rapid discharge can cause a number of adverse consequences: prolapse of the umbilical cord, pen, premature placental abruption. To do this, the amniotic sac is ruptured from the side; the hand is not removed from the vagina, holding back the rapid outpouring of water. After amniotomy, excessive stretching of the uterus disappears, and its contractile activity improves.
The expulsion period is also left to its natural course. Active action is resorted to only when complications arise that threaten the well-being of the mother and fetus. If pushing is weak, agents that enhance labor are used; carry out the prevention of fetal asphyxia.
After the birth of the first fetus, not only the fetal but also the maternal ends of the umbilical cord are carefully tied. This is necessary because after the birth of the first fetus it is impossible to determine whether the twins are identical or fraternal. With identical twins, the second fetus may die from blood loss (through the umbilical cord of the first fetus, if it is not tied). After the birth of the first fetus, an external examination is performed and the position of the second fetus and the nature of its heartbeat are determined. If the woman in labor is in good condition, the fetus is longitudinally positioned, and there is no asphyxia or other complications, labor continues expectantly.
If the second fetus is not born within 10-15 minutes, the amniotic sac is opened and labor is allowed to proceed naturally. Some obstetricians suggest rupturing the amniotic sac after 30 minutes, on the assumption that during this time the uterus will contract and its motor function will increase.
When the second fetus is in a transverse position, the fetus is turned onto its stem and then removed. In a breech presentation, the fetus is removed by the leg or inguinal fold.
If fetal asphyxia or bleeding from the birth canal occurs, immediately turn the fetus and remove it; if the fetal head is in the cavity or at the pelvic outlet, the birth is completed by applying obstetric forceps.
The third stage of labor requires special attention. It is necessary to carefully monitor the condition of the woman in labor and the amount of blood lost. At the beginning of the afterbirth period, the woman in labor is given intravenous uterine contractions (oxytocin or methylergometrine) to prevent blood loss. If bleeding occurs, measures are immediately taken to remove the placenta from the uterine cavity. If there are signs of separation of the placenta, it is isolated externally. If the placenta has not separated and the bleeding is significant, manual separation of the placenta and release of the placenta are used. The birth placenta(s) are carefully examined to ensure its integrity and to establish the identical or dizygotic origin of the twins.
In the first hours after childbirth, you need to monitor the condition of the mother, contractions of the uterus and the amount of blood released from the genital tract. If the uterus contracts sluggishly, agents that contract it are administered, and an ice pack is placed on the stomach; If necessary, apply uterine massage and other measures to combat bleeding.
In the postpartum period, during multiple pregnancies, uterine involution occurs more slowly than after childbirth with a single fetus. Therefore, it is necessary to monitor the nature of the discharge (lochia), contractions of the uterus and the general condition of the postpartum woman. If necessary, medications are prescribed to reduce it. Such postpartum women benefit from gymnastic exercises that strengthen the muscles of the abdominal wall and pelvic floor.
Perinatal mortality in multiple births is 2 times more likely than in single births. Therefore, in modern obstetrics there is a tendency to expand the indications for abdominal delivery in the interests of the fetus.
Indications for caesarean section in multiple pregnancies:
- transverse position of both fetuses or the first fetus;
- breech presentation of both fetuses or the first fetus;
— excessive overstretching of the uterus and large fetuses (total weight more than 6 kg);
— hypoxia of the fetus (fetuses);
- presence of a diagnosed one amniotic sac;
- conjoined twins;
- unprepared birth canal after 38 weeks of pregnancy;
- severe gestosis, in which natural childbirth is contraindicated;
— anomalies of labor, umbilical cord prolapse, placenta previa and abruption, other obstetric indications;
- extragenital pathology of the mother, requiring surgical delivery.
If there are no special indications, then natural childbirth is optimal. But if there are three or more children, regardless of the woman’s condition, it is recommended to perform a cesarean section at 34-36 weeks.
Development of twins after birth
Unfavorable conditions of intrauterine development, complications of pregnancy and childbirth affect the physical condition and development of newborns. They usually weigh less than single-born children, and catch up with them in height and weight only after 1.5 years.
Due to their reduced weight, twins have reduced resistance to infections and get sick on average 3 times more often than other children. They experience sleep disorders, especially in infancy: intermittent, restless, shallow sleep. Eating disorders are observed - from refusal to eat to overeating. These disturbances subside after 3 years of age, but may continue into adulthood. Enuresis (more common in boys) occurs in approximately 15% of twins. As a rule, children acquire neatness skills by the age of 3.5 years; for twins this happens later.
More often, the role of the main, strong, intelligent child in a twin pair is played by the first-born child, since he usually has a higher birth weight and develops faster.
Medical literature on obstetrics
Prenatal echography: differential diagnosis and prognosis - M.V.
Fundamentals of ultrasonic fetometry - M. V. Medvedev
Screening ultrasound examination at 11-14 weeks of pregnancy - M. V. Medvedev
Screening ultrasound examination at 18-21 weeks of pregnancy - M. V. Medvedev
Screening ultrasound examination at 30-34 weeks of pregnancy - M. V. Medvedev
Fundamentals of volumetric echography in obstetrics - M. V. Medvedev
Ultrasound diagnostics in obstetrics and gynecology for beginners - N. A. Altynnik






