- Home /
- Branches /
- X-ray /
- X-ray of the calcaneus
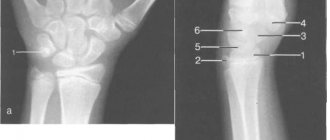
X-ray of the heel bone is an indispensable and accessible research method and is widely used by traumatologists and orthopedists to diagnose heel bone pathology.
The heel bone is the largest bone of the foot and, due to its anatomical features, it bears most of the load, which provokes injury. An X-ray of the heel bone is indispensable in diagnosing and assessing the effectiveness of treatment of heel spurs (plantar fasciitis); in addition, the study is carried out to determine neoplasms and injuries of the heel bone. Advantages:
- Non-invasive and accurate diagnostics
- Minimum radiation dose with high image quality, which is ensured by our X-ray system
- Possibility of recording images onto the patient’s electronic media (digital equipment)
What does a calcaneal x-ray show?
X-rays of the heel bone allow the doctor to determine:
- condition of the heel bone (integrity, shape);
- damage to the heel bone (subluxations, cracks and fractures);
- congenital structural features;
- benign and malignant tumors of bone and joint formations;
- flat feet;
- heel spur;
- osteochondropathy (Haglund-Schinz disease);
- arthrosis and arthritis;
- synovitis;
- gout;
- the degree of pathological changes in the calcaneus.
Preparation and procedure
No special preparation is required for the study. The patient is placed on a special table, the groin area is protected with a lead apron. For children, additional protection is used for the thyroid gland and eyes; the baby is completely covered with an apron, leaving only a limb exposed.
An image of a joint or bone can be taken in one or more projections. To obtain accurate data, it is important to remain still. The study takes just minutes. The doctor sees the condition of the tissues immediately, and a conclusion with a transcript is issued after the procedure.
Excess body weight can become a hindrance - fat cells distort X-rays. This results in the picture not being clear enough. In this case, the attending physician will suggest alternative examinations. Sometimes it is possible to solve the problem by taking pictures from several projections. Some diseases and injuries require only a direct projection, others require a lateral projection, on both sides. Occasionally they resort to a combination of several options. This allows you to get the most accurate picture of the condition of the bone tissue.
Patients who need to have joint x-rays often ask whether the procedure is harmful. The harm from radiation during such diagnostics is minimal if we are talking about the use of modern equipment. The ViTerra clinic uses advanced X-ray equipment with minimal radiation. The photo is taken quickly, which reduces the burden on the body. For example, during an X-ray of the knee joint, the radiation dose is 0.001 mSv - almost the same amount a person receives every day in the course of his life. Therefore, the image can be repeated after 2–4 weeks to assess the effectiveness of the prescribed treatment or the dynamics of tissue healing.
Indications for the study
X-rays of the heel bone are indicated for suspected:
- bone fracture;
- heel bruise;
- tuberculosis of the calcaneus;
- malignant bone tumor;
- heel spur;
- osteomyelitis;
- osteoporosis.
The study is also carried out if:
- severe pain or burning in the heel;
- hematomas and swelling of the heel area;
- signs of bursitis, fibrositis;
- mobility restrictions;
- heel spurs;
- altered gait (shift of the center of gravity to the fingers).
An x-ray of the heel bone is required after treatment for heel spurs to assess the effectiveness.
Heel spur
Which doctors should I contact?
Foot pathology is dealt with by orthopedic traumatologists and surgeons. The necessary list of physiotherapeutic procedures, massage and therapeutic exercises is prescribed by a physiotherapist. If there are concomitant diseases, appropriate laboratory and instrumental studies and consultations with specialists may be required.
Heel spur treatment
One of the main goals of heel spur treatment is to control pain and relieve inflammation. Real effect can only be achieved with an integrated approach.
Foot relief method
.
The most effective method of treatment is to return the foot to the correct position when walking, restore the arch of the longitudinal arches and reduce pressure on the heel area. It is considered rational to wear orthopedic shoes, which prevent overstretching of the plantar ligament and have a maximum shock-absorbing effect, creating comfort while walking. One of the most affordable options is the production of individual arch supports that make physiological foot placement possible. Drug therapy
. Currently, drugs from the group of non-steroidal anti-inflammatory drugs in the form of ointments and creams are used to treat heel spurs. tablet or injection forms. It is worth noting that this is a symptomatic treatment method that does not provide a lasting analgesic effect and does not affect the course of the disease, and also has many unwanted side effects.
Corticosteroids are usually used to reduce pain and inflammation. Although plantar fasciitis is a degenerative rather than an inflammatory process, evidence of the short-term therapeutic effect of corticosteroids suggests. The most common treatment for heel spurs is injections of hormonal drugs.
Tension of the calf muscles aggravates the disease and increases heel pain, so muscle relaxants can be used to reduce it.
In combination with analgesics, they significantly increase the effectiveness of treatment and make it possible to reduce the dose of painkillers.
Physiotherapy:
- electrophoresis with hyaluronidase or 5% calcium chloride solution: introduction of drugs into the tissue using an electric current;
- sonophoresis with hydrocortisone: treatment of tissues with ultrasonic waves that improve the penetration of drugs;
- ultrasound therapy: heating tissues and reducing inflammatory reactions using ultrasonic waves;
- magnetic therapy;
- mud and mineral baths;
- laser therapy: heating the deep layers of tissue with a laser helps to locally improve blood flow.
Shock wave therapy
is a non-invasive treatment method that can quickly reduce or completely eliminate pain. The technique is based on the influence of ultrasonic waves of a certain frequency in order to destroy calcium deposits, reduce inflammation and relieve swelling, and activate tissue regeneration. Under the influence of the shock wave, blood circulation increases, the permeability of cell membranes changes and cellular ion exchange is restored, thereby providing anti-inflammatory and decongestant effects.
Therapeutic exercise and massage
. In the subacute period, when the intensity of the pain has decreased, physical exercises are added to the treatment aimed at stretching the calf muscles of the leg and plantar fascia, improving the mobility of the ankle joint, as well as strengthening the muscles responsible for the correct positioning of the foot during movement. Massage improves metabolic processes in tissues and relieves pain associated with reflex muscle spasms.
Therapeutic exercise and massage are aimed at correcting the biomechanics of the body, which can significantly alleviate the course of the disease and prevent its relapse.
Surgery
. The only way to get rid of a large heel spur is through surgery. When choosing the classic version of the operation, the surgeon cuts the fascia completely and removes the bony protrusion. A more modern and gentle technique is radiofrequency microtenotomy. The essence of the operation is to eliminate damaged tissue using radio frequency waves.
Local administration of hormones (corticosteroids) to the site of inflammation and surgical intervention are extreme measures, which are resorted to only in cases where other treatment methods have not brought the desired result.
In complex cases characterized by a long-term and recurrent course, surgical treatment is the only method.
Complications
The main complication of heel spurs is a deterioration in the quality of life associated with pain and the inability to lead an active lifestyle. Patients often have disturbed sleep, increased anxiety and irritability. They are forced to avoid resting on the sore heel and transfer weight to the healthy limb. This negatively affects gait and posture and increases the risk of joint damage to the weight-bearing limb. With severe pain, asymmetry of posture appears, which leads to the progression of osteochondrosis and the occurrence of pain in the lumbar region. As a result, the patient is forced to limit physical activity.
Other complications, such as tearing of the fascia from the attachment site and suppuration, are rare.
Prevention of heel spurs
In most cases, the development of heel spurs can be prevented. It is recommended to provide regular rest to the feet in combination with proper exercises, and to take breaks to warm up during work if it involves constant stress on the feet.
Shoes should be comfortable, and if you have flat feet, orthopedic.
It is useful to wear individual orthopedic insoles that fit the entire area of the foot - they allow you to restore the normal height of the arch of the foot in the first weeks of constant wear and, thus, reduce the tension of the plantar fascia.
To reduce the severity of pain in the heel area and reduce the load on the plantar aponeurosis, you should take shorter steps, avoid walking barefoot, and avoid running, dancing, and wearing inappropriate shoes.
Sources:
- Reznik L.B., Erofeev S.A., Silantiev V.N., Turushev M.A., Kuznetsov N.K. Current state of the problem of surgical treatment of plantar fasciosis (literature review). Genius of Orthopedics, magazine. T. 24. No. 4, 2021. P. 515-520.
- Bone spurs. Great Medical Encyclopedia (BME), edited by Petrovsky B.V., 3rd edition, volume 27.
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor.
Preparing for the study and carrying out the procedure
X-ray of the foot does not require special preparation. The patient should remove clothing (including shoes), jewelry, or any metal objects that may interfere with the image.
A developing fetus is more sensitive to the effects of radiation than an adult and therefore is at greater risk of harm from X-ray examinations, so if the patient is pregnant, the doctor should be informed.
Although the procedure may take about 15 minutes or longer, the actual radiation exposure is usually less than a second.
The patient enters a special room, which will likely contain a table and a large X-ray machine hanging from the ceiling.
Parents can usually come with the child to ensure peace of mind. Accompanying persons will need to wear a special protective apron to protect certain parts of the body.
The x-ray technician positions the patient both on and off the table to achieve the required position. Then he goes behind the wall, or into the next room to control the machine.
The three x-rays are usually taken from the front, side and angle, so the technician will return to reposition the leg for each new x-ray. Sometimes doctors ask for x-rays of the opposite leg for comparison.
Anatomy of the foot and ankle
Content:
- Anatomy of the foot and ankle
- Indications for the study
- Preparing for the study and carrying out the procedure
- Getting Results
- Risks of X-rays of the foot and ankle
The feet are a flexible structure of bones, joints, muscles and soft tissues that allow you to stand upright and perform activities such as walking, running and jumping. The forefoot contains five toes (phalanxes) and five longer bones.
The middle of the foot consists of pyramidal bones that form the arches of the legs. These include the three sphenoid bones, the cuboid bone and the scaphoid bone.
The back of the foot forms the heel and ankle. The talus supports the lower leg bones (tibia and fibula) to form the ankle. The heel bone is the largest bone in the leg.
Muscles, tendons and ligaments run along the surfaces of the feet, allowing complex movements to be made. The Achilles tendon connects the heel to the calf muscle and is important when running, jumping and standing on your toes.
The ankle joint allows you to move your leg up and down. The subtalar joint sits below the ankle joint and allows lateral movement of the foot.
Numerous ligaments (made of tough, flexible tissue) surround the true ankle and subtalar joints, connecting the leg bones to each other.
Getting Results
The patient will not feel anything during the x-ray. The x-ray room may be cool due to the air conditioning used to keep the equipment operating properly.
The positions required for x-rays may be uncomfortable, but only need to be held for a few seconds.
If the patient is injured and cannot remain in the required position, the technician may find another position that will be easier for him.
A radiologist is a doctor specially trained in interpreting x-ray images. He will be the one to review the patient's x-rays.
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
After evaluating the results, the radiologist will send a report to the attending physician, who will discuss with the patient what the images show and explain what it means.
In emergency situations, X-ray results can be available quickly. And usually the results are ready in 1-2 days. In most cases, results can be given directly to the patient or family during the examination.
Calcaneal fracture (heel fracture)
Treatment is usually carried out in a trauma department and can be conservative or surgical. The treatment program is determined by the type and severity of the heel fracture and includes open or closed reduction (if there is displacement), immobilization, anesthesia, a special regimen, and the use of additional means (crutches).
Fractures without displacement
Non-displaced heel fractures and marginal tuberosity fractures are treated using conservative methods. After anesthesia of the injury site, a plaster boot with carefully modeled arches is placed on the leg. For pain relief, analgesics are administered intramuscularly in the first days after injury. The patient is referred to exercise therapy and UHF is prescribed. The plaster is removed after 8-10 weeks. The patient is recommended to wear orthopedic shoes with arch supports for at least 6 months.
Compression and comminuted fractures
Treatment of complex intra-articular fractures of the calcaneus is associated with significant difficulties due to the difficulty of restoring the normal relative position of the fragments and holding them until union. Taking into account the type of fracture and the nature of the displacement, the following methods can be used:
- Closed reduction
. It is carried out using special manual techniques. First, the lengthwise displacement is eliminated, then the heel flattening, and finally the lateral displacement of the fragments. The limb is immobilized with a plaster cast. - Simultaneous skeletal traction
. Allows you to increase traction and increase the accuracy of manipulations. It is carried out using one or two knitting needles, which are passed through the fragments. The knitting needles are secured to staples, the above techniques are performed, the bone fragments are fixed with other knitting needles, and a plaster cast is applied. - Reposition using the Ilizarov apparatus
. Indicated for stale heel injuries that cannot be eliminated by immediate reduction. It is performed within 1-2 weeks under regular x-ray monitoring. In the future, treatment is carried out according to the same principles as with simultaneous traction.
If conservative treatment is ineffective, surgical interventions are performed. Osteosynthesis of the calcaneus is performed using screws and reconstruction plates; metal structures are used with caution due to the high risk of complications. In the presence of bone defects, auto- or homo-bone transplantation is additionally performed. In case of complex old injuries, an Ilizarov apparatus is applied for microdistraction of fragments for 2.5-3 months.
In the postoperative period, analgesics and antibacterial agents are prescribed. Physical therapy is a mandatory part of treatment. Physiotherapeutic methods include:
- local cryotherapy;
- ultraviolet irradiation;
- laser therapy;
- magnetotherapy.
The immobilization period for complex calcaneal fractures is 3-4 months. After removing the plaster cast, it is recommended to wear insoles with arch supports to prevent flat feet. The total duration of the period of incapacity reaches 5-6 months.