Interesting Facts
| Options | Indications |
| Time from conception | 17 weeks |
| Period by month | 19 weeks |
| What month | 5 |
| Dimensions and weight of the fetus | 200-230 mm, 240-270 g |
| Uterus dimensions | 1-2 cm below the navel or at its level |
| Pregnant weight | The increase over the last week is no more than 400-500 g |
Your baby is the size of
Mango
200-230mm Size
240-270 g Weight
This is a quiet time for mom and baby. Every day your tummy becomes more and more rounded, and the fetus becomes like a tiny person.
Baby's activity and movements
It is at 19 weeks that the baby is most active: there is still enough free space in the uterus for him to move, and the nervous system stimulates the brain to improve movements. The child clenches his fingers and somersaults, pushing away from the walls of the uterus. The development of the fetus in the 19th week of pregnancy allows the expectant mother to experience completely new sensations: first, light tremors, then more active movements. These movements bring the main positive news: the pregnancy is proceeding normally. If this is your second or third pregnancy, you may feel fetal movements a couple of weeks earlier than this.
Feelings of the expectant mother
Pregnancy can no longer be hidden from prying eyes; the belly is noticeable, even if the woman is wearing loose clothes. Vaginal discharge becomes more abundant. This is normal, due to the influence of progesterone. Skin pigmentation increases. Spots can appear on the forehead, cheeks and upper lip - this is the so-called chloasma, or mask of pregnancy. The skin on the inner thighs darkens. It is also a result of hormonal changes.
By week 19, as a rule, a woman can gain from 3.5 to 6.5 kg. The pain in the breast goes away, the mammary gland has noticeably enlarged, and many people are already producing colostrum.
What happens to the uterus?
She, of course, is growing, and now her bottom, that is, the upper part, is located approximately at the level of the navel. Its approximate weight is 300 grams. The uterus puts pressure on the internal organs, which causes frequent urination, heartburn, constipation, and shortness of breath. Due to a shift in the center of gravity of the body, a pregnant woman experiences lower back pain.
Who should be screened?
All expectant mothers undergo ultrasound diagnostics in the 2nd trimester. If there are no risks, the doctor nevertheless urgently needs to assess the development of the fetus, have information about the child’s growth and weight gain, and how adequately all his organs are formed. In addition, it is important to monitor the condition of the mother’s placenta, which right now, during this period of pregnancy, is actively transforming in order to provide the baby with the necessary nutritional substances and meet the need for oxygen.
Therefore, at an appointment in the first months of pregnancy, the clinic doctor will remind the woman of the importance of screening in the 2nd trimester, clarify in what week she needs to have an ultrasound, tell in detail how and what is looked at during the manipulation and why this study plays such a role.
Venous blood sampling for biochemical analysis will be recommended only for those women who have a history of some risk of developing an anomaly or previous screening results whose hormonal examinations at the beginning of pregnancy were questionable.
Pregnancy 19 weeks: fetal development
The nineteenth week of pregnancy is a period of active growth of the baby. Now he is 240-270 grams and 20-23 cm. He still has enough space in the womb, so he often moves, turns over, tumbles, pushes. His actions are more coordinated. The body has the correct proportions, cartilage tissue continues to be replaced by bone. A sleep-wake pattern arises, which often may not coincide with the mother’s, and then many women wake up at night, feeling fetal movements.
The nervous system is developing rapidly:
- Areas responsible for the perception of smell, sounds, touches and visual images are formed in the brain.
- The formation of the myelin sheath of nerve fibers, which is responsible for communication between cells, continues.
- The development of visual analyzers is completed, and soon the baby will begin to open and close his eyes.
How often does the baby move at 19 weeks of pregnancy?
The norm is 10 movements within 12 hours. A lower number indicates a lack of oxygen in the fetus and requires consultation with a specialist. However, at this stage it is too early to make such calculations: the child is not so large that the mother could track all his movements. The test is informative from 24-28 weeks, depending on the type of pregnancy.
Examination price
The cost of ultrasound in the second trimester on average ranges from 600-850 rubles. For the study of uteroplacental-fetal blood flow using Doppler, you need to pay about the same amount. Such a complete examination is advisable, since Doppler allows you to find out the functionality of the cardiovascular system. In case of multiple pregnancy (if twins or more are expected), the price for ultrasound and Doppler examinations will increase by 150-200 rubles. If it is not possible to take a photograph yourself, you can purchase an ultrasound image directly from a sonologist. This service will cost on average 150-300 rubles.
Ultrasound is ideal for prenatal screening. It does not cause discomfort and does not hide any health risks for the expectant mother and her child. In addition to the above, an important advantage is its high effectiveness - with its help, at 19 and other weeks of pregnancy, you can learn in detail the process of formation and stages of development of the child’s body systems, and assess the functionality of the woman’s reproductive organs.
Tests and ultrasound
At your next gynecologist appointment, take a general urine test to rule out infections of the genitourinary system, as well as a general blood test, where the most important indicator will be the hemoglobin level. Using it, the specialist will determine the presence or absence of anemia, a common complication of the 2nd trimester associated with a lack of iron in the blood.
Now is the optimal time for 2 pregnancy screenings. Using ultrasound and biochemical blood tests, you can identify the risks of developing genetic pathologies in the fetus. During an ultrasound examination, the sex of the unborn child can be determined.
Description of the diagnostic procedure

The manipulation is done transabdominally - through the anterior abdominal wall. A pregnant woman lies with her back on the couch and removes her belly from clothes. The doctor applies the gel to the abdomen and slides a sensor over it, which is attached to the monitor of the device. The fetus is visualized on the screen, the doctor measures all the necessary indicators.
Most often, there are 2 monitors in the office so that the expectant mother can also watch her baby. The presence of the future dad is also allowed, who can take a photo of the monitor with the image of the baby.
What to discuss with your doctor
I don't feel fetal movements
If this is your first pregnancy, then normally you can first feel the baby’s movements in the womb at 18-20 weeks. Listen to yourself. If you have already experienced this sensation, and then it disappeared for 10-12 hours, then you should contact a gynecologist to make sure that everything is okay with the child.
I have pain in my lower abdomen and groin
Typically, discomfort occurs after sudden movements and goes away on its own within a few minutes. This is how the round ligament is stretched, which holds the uterus in the correct position. If your lower abdomen hurts for a long time and is accompanied by unusual vaginal discharge, you should immediately seek medical help.
What will you need for an ultrasound?

Carrying out ultrasound diagnostics does not require special preparation. The procedure itself is also not a complex manipulation. At this stage, there is no need to fill the bladder, since there is already enough amniotic fluid to examine the structure of the areas of interest. Eating food before the procedure does not in any way affect the results of the ultrasound.
Many clinics do not indicate the need to bring anything with you; otherwise, you will be warned about this in advance. Most often, for the procedure, the patient may need a diaper and napkins. The diaper will need to be placed on the couch, since the ultrasound is performed in the supine position. Wipes are used to wipe away excess gel.
Low placentation - a possible complication of the 19th week
By this time, the formation of the placenta ends. The course of pregnancy depends on the place of its attachment to the wall of the uterus. Normally, the placenta should attach to the highest point of the uterus, where the best blood flow is. When it is located in the lower part, in the area of the cervix, we are talking about placenta previa. As the fetus grows, it puts pressure on it, which can lead to detachment and the threat of miscarriage.
There is no specific treatment for this condition. There are only general recommendations: exclude intimate life and physical activity. If by the 36th week the placenta does not rise on its own, then the woman is hospitalized in the maternity hospital and, according to indications, a cesarean section is performed.
First ultrasound in early pregnancy (up to 11 weeks)
Ultrasound examination of pregnancy from A to Z
An ultrasound can not only determine the presence of pregnancy, but also monitor the growth and development of the baby.
Ultrasound examination is the only method to detect fetal malformations. The study allows you to timely detect a frozen pregnancy, ectopic pregnancy, establish the cause of bleeding, and suspect the presence of a chromosomal pathology in the fetus (for example, Down's disease). The safety of ultrasound during pregnancy is confirmed by research from the American Institute of Ultrasound in Medicine, during which no changes were found in mammalian tissues and cells when exposed to ultrasound. Using this method for more than 30 years, there was no evidence of any complications in the fetus.
Fetal ultrasound has become firmly established in clinical practice. We provide you with information about what an ultrasound scan should include at different stages of pregnancy and what result you should get after undergoing this study.
The first ultrasound in early pregnancy is usually performed using a transvaginal probe. At 6-10 weeks of pregnancy, an ultrasound makes it possible to establish that this pregnancy is progressive (i.e., the fetus has a normal heartbeat), develops inside the uterus (i.e., exclude the dire diagnosis of ectopic pregnancy), and determine the number of fetuses. This study is recommended for those women who have had spotting during this pregnancy, or have had a previous miscarriage, missed abortion or ectopic pregnancy.
At 11 weeks the fetus is of sufficient size that a detailed assessment of its major anatomical structures can be made. During these periods, severe fetal malformations that are incompatible with life or lead to severe disability can be diagnosed.

This is how the coccygeal-parietal size of the fetus is measured in the first trimester

Fetal hand at 12 weeks of pregnancy
From 11 to 13 weeks, ultrasound markers (signs) of chromosomal pathology of the fetus can be detected - an increase in the thickness of the fetal nuchal space and the absence of the nasal bone during ultrasound.
Fetal nuchal translucency thickness (FNT) is the size of the area between the fetal skin and the soft tissues surrounding the cervical spine. The nuchal space is detected in fetuses both normally and with chromosomal diseases (for example, Down's disease), but fetuses with chromosomal diseases are characterized by an increase in the thickness of the nuchal space by more than 2.5 mm. The nuchal translucency in all fetuses disappears spontaneously after 14 weeks of pregnancy, so it is very important to have a study done from 11 to 13 weeks of pregnancy, when it can be measured.
The nasal bone is normally determined by ultrasound from the 10th week of pregnancy. In fetuses with chromosomal pathology, ossification processes occur later, so the absence of the nasal bone during ultrasound examination at this time may be a sign of chromosomal pathology of the fetus.
The physician must be highly skilled in assessing these signs, since obtaining the necessary views of the fetus in early pregnancy requires experience and technical skill. To measure TVP, you need to obtain the following image:

In the ultrasound photo of a pregnant woman, only the head and upper part of the fetal body are visible, the profile, nasal bone and TVP are clearly visible. Quite often you can see such incorrect images:
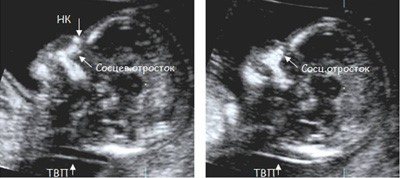
In these images, the fetus lies crookedly, the image magnification is insufficient, and a clear profile of the fetus cannot be seen. Measuring TVP in such images is INCORRECT and leads to an overestimation or underestimation of the risk of Down syndrome!!!
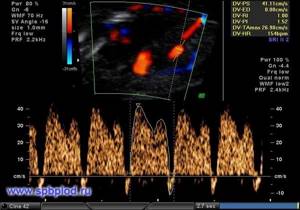
In addition to measuring the thickness of the nuchal translucency and assessing the nasal bone, several other markers have been proposed: assessment of blood flow through the tricuspid heart valve and through the ductus venosus, as well as measurement of the fetal facial angle. The assessment of these markers requires highly qualified physicians, and is possible only after obtaining international certification for each marker.
Typically, blood in the fetal vessels flows in one direction: from the heart to the peripheral vessels. If there is a chromosomal abnormality in the fetus or heart defects, the direction of blood flow may change, and in some phases of the cardiac cycle, blood begins to flow back to the heart.
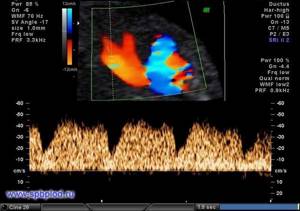
Normal blood flow in the fetal ductus venosus at 12 weeks of pregnancy
Reverse blood flow in the fetal ductus venosus at 12 weeks of gestation
Registration of blood flow through the tricuspid valve of the heart and through the ductus venosus (this small vessel is present only in fetuses; during the newborn period, the blood flow in it stops and it closes) allows us to identify up to 65% of fetuses with Down syndrome. In 1-3% of normal fetuses we may also see reversed flow in the ductus venosus or tricuspid valve, so these findings must be assessed in conjunction with other ultrasound findings.

Normal blood flow through the tricuspid valve of the fetal heart at 12 weeks gestation

Pathological reverse blood flow through the tricuspid valve of the fetal heart at 12 weeks of pregnancy
Measuring the fetal facial angle is based on the fact that the faces of patients with Down syndrome are wider and flatter than those of normal people. The same pattern is observed in fetuses with this disease. By measuring the angle between the frontal bone and the upper jaw of the fetus, an objective conclusion can be made about the presence of a flattened profile in the fetus; this marker is present in 60-65% of fetuses with Down syndrome in the 1st trimester of pregnancy.

Method for measuring the facial angle of the fetus at 12 weeks of pregnancy
If the necessary standards are met, an ultrasound examination at 11-13 weeks of pregnancy assessing the thickness of the nuchal translucency, nasal bone, facial angle, blood flow through the tricuspid valve and ductus venosus can identify up to 80% of fetuses with Down's disease and other chromosomal diseases, and in combination with biochemical screening allows you to increase the diagnostic efficiency to 85-90%. It should be emphasized once again that the assessment of these markers requires a highly qualified doctor and is possible only after undergoing appropriate training and certification.
Ultrasound examination at 11-13 weeks of pregnancy is currently the most effective way to prevent the birth of a child with Down syndrome or other chromosomal diseases.
Scheme for measuring the thickness of the collar space

And this is what the fetus looks like on three-dimensional images (3D/4D ultrasound) in the first trimester:

We hope that this information will help you better understand why we are conducting this study, and why it is important to conduct it specifically from the 11th to the 13th week of pregnancy.
At 18-22 weeks of pregnancy, the fetus reaches a mass of 400-500 grams and a length of 22-27 cm. With such dimensions, an ultrasound examination makes it possible to examine in detail all the anatomical structures of the fetus and identify the majority of malformations that require surgical correction or lead to a deterioration in the child’s quality of life. In addition, this ultrasound scans for markers (signs) of Down's disease and other chromosomal diseases. The appearance of many fetal organs with Down syndrome has slight differences from the appearance of normal organs, and a comprehensive assessment of all anatomical structures makes it possible to assess the risk of the fetus having Down syndrome and, if necessary, recommend in-depth diagnostics (using invasive methods) of this disease.
After an ultrasound scan at these times, most questions of prenatal diagnosis are considered closed.
In addition, an ultrasound at 18-22 weeks assesses the amount of amniotic fluid, the position and structure of the placenta. The transvaginal sensor can accurately measure the length of the cervix and thus determine the risk of premature birth. This study is especially recommended for women who have already had premature birth, cervical surgery, and also with multiple pregnancies.

2D profile of a fetus at 20 weeks of gestation

Fetal spine at 21 weeks of gestation in 2D mode

Fetal heart chambers at the 22nd week of pregnancy in 2D mode
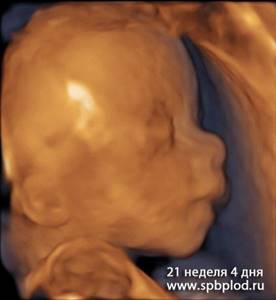
Ultrasound of the fetus at 21 weeks and 4 days in 3D mode
The main task of ultrasound at 32, 33, 34 weeks is to measure the circumference of the head and abdomen, the length of the bones of the limbs, and calculate the estimated weight of the fetus. This allows us to predict whether spontaneous birth is possible, whether there is a delay in fetal development or its disproportionate development.
In addition, ultrasound at 32-34 weeks allows:
- evaluate the appearance of the placenta and ensure that its position in the uterus does not interfere with normal labor
- measure the amount of amniotic fluid and exclude polyhydramnios and oligohydramnios
- assess the location of the fetus in the uterus (cephalic, pelvic or transverse)
- assess blood flow in the fetal and umbilical cord vessels using Doppler ultrasound to ensure that the fetus is receiving sufficient oxygen and nutrients
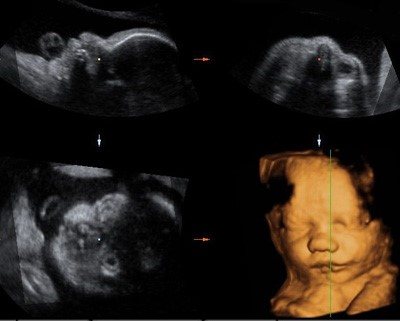
Fetal face in 3 projections in 2D mode and its three-dimensional (3D) reconstruction
A conventional ultrasound is a series of two-dimensional flat images of the fetus or its individual organs.
3D (3D) ultrasound is a method of obtaining an image, which is achieved by complex transformation of the obtained two-dimensional information into a three-dimensional three-dimensional model. Transformations are carried out using a special three-dimensional sensor and computer programs included in the ultrasound machine. The resulting volumes can be rotated and viewed from different angles.
4D (4D) ultrasound is the acquisition of a three-dimensional image of the fetus and its movements in real time. Thus, in addition to the three-dimensional image of the fetus, a fourth dimension is added - time, and it is possible to consider the motor activity and facial expressions of the fetus in motion.
Ultrasound in 3D and 4D modes can be done at different stages of pregnancy, but the result and quality of the image primarily depends on the position of the fetus in the uterus, the amount of amniotic fluid in front of its face, the presence of obstacles in the path of the ultrasound wave (uterine fibroids, uterine scar, subcutaneous tissue may obstruct examination and reduce image quality). So, if the fetus lies close to the wall of the uterus, then it is almost impossible to obtain a three-dimensional image of its face, just as it is impossible to see the face of a person who has rested his head against the wall. Sometimes you have to wait 15-20 minutes and continue the study after changing the position of the fetus.
The optimal period for obtaining an image of the fetal face is 20-26 weeks of pregnancy. At these stages, the fetus often changes its position, and there is enough water around it to see the face and body. After 30 weeks of pregnancy, the fetus is so large that it has to cluster well to fit in the uterus. However, obtaining a beautiful three-dimensional image of the face can be difficult and even impossible - it all depends on the position of the fetus.
It is important to understand that 3D/4D ultrasound is performed in addition to regular fetal ultrasound and cannot completely replace it. Measuring the size of the fetus and excluding malformations is carried out using conventional two-dimensional ultrasound. Only for some malformations does the use of three-dimensional ultrasound provide the doctor with additional information.

3D ultrasound of the fetus at 11 weeks and 4 days
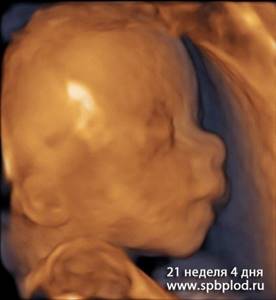
3D ultrasound of the fetus at 21 weeks and 4 days
Ultrasound during multiple pregnancy
A multiple pregnancy is considered a high-risk pregnancy for various complications for the mother and fetus, since a woman’s body is more designed to carry one fetus. Therefore, during multiple pregnancies, it is necessary to conduct ultrasound more often and monitor the growth and development of the fetus. There are several types of twins, depending on the number of placentas and membranes.
Dichorionic diamniotic twins are the most favorable type of twins. Each fetus has its own placenta and its own amniotic space, separated from the other by the amniotic septum. The fruits can be of the same or different sex. The probability of delayed development of one of the fetuses is 20% (4 times higher than in a singleton pregnancy), premature birth is 5% (1% in a singleton pregnancy). In order to promptly identify these complications, it is necessary to conduct an ultrasound at 11-13 weeks, 18-22 weeks (as in a singleton pregnancy) and then every 4 weeks until birth (in a singleton pregnancy - at 32-34 weeks). If any complications are detected, the number of ultrasound scans may increase.
Monochorionic diamniotic twins - occurs when a fertilized egg splits into two parts. In this case, the fetuses have one common placenta and their own amniotic space. The fruits are always the same sex and completely genetically identical. The presence of a single placenta can lead to the development of specific complications associated with the fact that the vessels in this placenta can connect the circulatory systems of both fetuses. In this case, one fetus receives some blood from another fetus, and they both suffer from this: one has excess blood, which leads to increased stress on its heart; the second does not receive enough blood, oxygen and nutrients, and begins to grow more slowly, as a result of which it develops intrauterine growth retardation. This complication is called feto-fetal transfusion syndrome, and without timely treatment can lead to the death of one or both fetuses. In order not to miss this complication, it is necessary to do an ultrasound at 11-13 weeks (as in a singleton pregnancy), at 16, 18, 20, 22, 24, 26, 28 weeks of pregnancy. If signs of feto-fetal syndrome are detected, ultrasound should be performed even more often - once a week. If there are no signs of this syndrome before 28 weeks of pregnancy, then its development in the future is extremely unlikely, and ultrasound can be performed once every 4 weeks - as with dichorionic twins.
Monochorionic monoamniotic twins - occurs when a fertilized egg is divided into two parts, while the fetuses have a common placenta and a common amniotic space.
The fruits are always the same sex and completely genetically identical. This is an extremely rare type of twins, and is accompanied by the greatest risk of complications, developmental delay and intrauterine death. In addition to the complications associated with a single placenta (see description above), the fetuses are located in a common amniotic space and are not separated by the amniotic membrane. This can lead to torsion and compression of their umbilical cords, stopping the flow of blood to one of them and, accordingly, its death. The risk of this complication is very high, so an ultrasound is performed every week of pregnancy, and if signs of umbilical cord torsion are detected, hospitalization and daily monitoring of the fetus are recommended; If the condition of one of the fetuses becomes critical, immediate delivery by cesarean section is required. Back to articles
Do's and Don'ts
The child’s sensory organs are already practically developed, and the formation of internal organs is finishing. During this period, a woman should be attentive to her diet, sleep and rest patterns, and physical activity.
You can and should:
- engage in swimming and special gymnastics for pregnant women - sport saturates the body with oxygen, strengthens muscles, improves blood circulation;
- perform Kegel exercises - developed pelvic floor muscles will help you during childbirth and prevent the development of postpartum complications;
- spend a lot of time outdoors - walking strengthens the nervous system;
- meeting friends, leading a cultural life - social activity calms you down and relieves anxiety.
You should not use a sauna or take a hot bath, or lift more than 3-5 kg. This increases the tone of the uterus and can cause premature labor. Choose comfortable shoes without heels to prevent swelling and fatigue in your legs and back. Avoid large amounts of simple carbohydrates in your diet: sweets and starchy foods increase the risk of gestational diabetes.
Don't forget what's important
In the middle of pregnancy, it is time for the expectant mother to begin preparing for childbirth and life with the baby. Courses and specialized schools for pregnant women will help you learn proper breathing during childbirth, choose a birth option (classical, water, vertical, partner, etc.), and also begin to create a list of necessary things for a newborn.
Things to remember at 19 weeks of pregnancy:
- About quality sleep. You can no longer sleep on your back and stomach, but it is quite possible to get a good night's sleep using a pregnancy pillow, which allows you to take the pressure off your stomach and legs, placing them comfortably on special bolsters.
- About drug restrictions. Even if you have a cold, do not rush to take the drug that you were usually treated with before pregnancy: first consult your doctor.
- About physical activity. Do not spend your pregnancy lying on the couch: walk and travel for your own pleasure, unless there are prohibitions from your doctor. Don’t forget that the best option would be to regularly visit a sports club: today, almost any sports network offers classes for expectant mothers in special yoga, aqua aerobics, belly dancing, and Pilates. If you decide to practice at home on your own, choose only the usual (not complicated) level, do not try to make the classes intense, and do not load your body the way you did before pregnancy. If you feel tired, weak, or dizzy, it is better to complete the classes. Rest after physical activity and walks: lie down for a while, have a snack.
- About body weight control. Of course, it’s nice to feel that toxicosis is over, but this is not a reason to get carried away with cakes and sweets. Carefully create your menu for every day (do not drink alcohol, soda, fast food, do not be lazy to cook homemade dishes in the oven and steam) - this way you will additionally take care of childbirth without complications.
- About essential vitamins. Do not forget to take all medications prescribed by your doctor: they are recommended not “just in case,” but in order to replenish the body’s missing reserves of nutrients. Now the fetus is developing a central nervous system, strengthening cartilage and bones, and developing sense organs: in order for everything to happen as planned, the baby needs vitamin support. Pay special attention to a course of magnesium B6 - it is prescribed by a gynecologist in case of increased uterine tone. The vitamin will help eliminate pain and reduce the risk of premature birth.
- About intimate life. Toxicosis has passed, and the tummy is not too big yet, so take the opportunity to resume your intimate life, if there are no medical prohibitions (if there is a threat of miscarriage, isthmic-cervical insufficiency, placenta previa). Choose the most comfortable positions for you, high-quality lubricants, and have fun without worrying about the baby: when it’s good for mom, it’s good for him too. For healthy women, sex during pregnancy is beneficial because during orgasm, the body releases the hormone of joy - endorphin. And active sexual positions allow a woman to strengthen the muscles of the pelvic floor and legs, which will be useful during vertical childbirth.
Checklist for 19 weeks of pregnancy
- Take a blood test for hemoglobin to rule out iron deficiency and anemia.
- Complete screening 2 if you have not done so previously.
- Choose a school for expectant mothers, where you can learn everything about pregnancy, childbirth, recovery after it, and caring for a newborn.
- Sleep on your left side with a pillow under your back and between your knees.
- Buy a maternity brace that will relieve excess stress from your back and prevent lower back pain.
We invite you to a school for expectant mothers at the Women's Medical Center. Here you will learn how to breathe correctly during childbirth, do self-massage, care for your body and baby after childbirth, and prepare for breastfeeding. Classes are taught by experienced obstetricians-gynecologists and pediatricians.
Your to-do list this week
In addition to managing your pregnancy symptoms, take time to relax. Stress is not good for you and your unborn baby. You may have some things to cover, but try not to put so much pressure on yourself.
Analyzes
Your ultrasound during pregnancy is a congenital anomaly scan (CAS), also sometimes called a congenital anatomy scan or a 20-week scan, performed in the second trimester, between 18 and 22 weeks. The International Society of Ultrasound in Obstetrics and Gynecology (Isuog) recommends CAS as part of routine prenatal care for all pregnant women.
This is a typical 2D or 3D ultrasound to check your baby's overall development. It simply helps rule out "fetal" growth abnormalities in more detail, such as anencephaly (lack of scanning of the top of the skull), heart defects and intestinal obstructions, as well as congenital malformations such as cleft lip and spina bifida.
Below are 19 weeks pregnant belly photos of expecting girls:

How is screening carried out?
When the deadline for ultrasound screening for the 2nd trimester comes, you need to make an appointment with your doctor. First, it is necessary to evaluate the results of previous studies. In order for the interpretation of screening results to be adequate, it is advisable to carry it out on the same device each time, in the same laboratory, and also for maximum objectivity with one doctor.
During the study, the woman lies on her back, the doctor places the device’s sensor on the anterior wall of the abdomen. The duration of the study is about 20-30 minutes. Additionally, Doppler sonography of the vessels of the fetus and uterus is performed to exclude hemodynamic pathologies and determine the parameters of the child’s heart.
If biochemical screening is prescribed, blood will be taken from the woman's vein.
Reliability of screening results
Sometimes it happens that according to the preliminary results of screening in the 2nd trimester, a woman is at risk for possible defects. Do not panic ahead of time, it happens that the results of the examination are false positive. The final result is influenced by many factors: age 35 years and older, the woman’s overweight (obesity contributes to changes in hormonal blood parameters), bad habits, past or present, taking medications or the unfavorable influence of the woman’s environment.
In each individual case, the doctor individually assesses the reliability of the tests and the presence of associated factors. If, nevertheless, a sufficiently high degree of risk of possible deviations is determined, then the expectant mother will be prescribed auxiliary studies:
- blood sampling for certain, specific hormones, in addition to the main ones;
- taking amniotic fluid to study its contents, a manipulation called amniocentesis;
- obtaining blood for analysis from the baby's umbilical cord artery - cordocentesis;
- histological examination of chorionic villi.
In addition to testing blood from a woman’s vein, other studies are invasive and quite difficult, but they most reliably refute or confirm the doctor’s conclusion, which he makes based on the results of screening in the 2nd trimester.
Norms
Normal screening values vary somewhat. It depends on the laboratory in which the research is carried out and what units of measurement the doctor uses. The final interpretation of the results will be influenced by some factors, such as the woman’s condition, circumstances (a woman is pregnant with one baby or several), body weight (overweight, obesity), previously identified chronic diseases, bad habits and addictions, method of conception (IVF, in in particular).
The doctor conducts a comprehensive assessment, looking at not just one indicator, but a set of results, their combination. As an example, the table shows the approximate norms of hormonal levels regarding the current gestational age:
| hormone | term | norm |
| AFP | 17-19 weeks | 15-95 IU/ml |
| hCG | 15-25 weeks | 10x103-35x103 IU/ml |
| free estriol | 17 weeks | 1.17-5.52 nmol/l |
| free estriol | 18-19 weeks | 2.43-11.21 nmol/l |
In combination with the results of ultrasound screening, the doctor makes a final conclusion about the likely presence of a particular complication in the fetus. It is worth considering that the conclusion after screening is not an established diagnosis, but only suggests a possible degree of risk.
What anomalies can be detected?
Based on the data shown by ultrasound screening together with blood biochemistry, the following malformations can be suspected:
- three chromosomes instead of two - so-called trisomy (these include such congenital pathologies as Patau syndrome, Down syndrome, Edwards syndrome);
- triplodia – a multiple set of defects due to tripling of chromosomes;
- various hernias;
- malformations of the baby's heart;
- deviations in the formation of the fetal nervous system;
- anomalies in the skeletal system and its structure.
All of these defects are very serious, the presence of some can provoke the child’s non-viability. Therefore, an ultrasound of the fetus from 11 to 22 weeks, a venous blood test for hormones, if necessary, and consultation with a specialist are strictly mandatory for a woman who has entered, so to speak, the second trimester of pregnancy. Even if, after screening performed in the first weeks after conception, the doctor did not suspect any risk, a repeat examination is necessary to completely exclude possible abnormalities and, of course, to give peace of mind to the expectant mother.










