What can be seen on an ultrasound
Ultrasound of the heart
Such a diagnostic method as cardiac ultrasound (cardiac ultrasound) is an accessible and informative study in pediatric practice. With the help of a sensor and a device, there is an excellent opportunity to “look” at the heart without violating the integrity of the body.
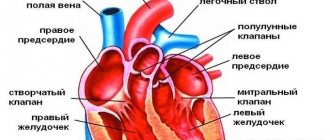
Using cardiac ultrasound, not only anatomical but also physiological parameters of the heart are assessed: left ventricular end-diastolic diameter (LVEDD), left atrium diameter (LA diameter), right atrium (RA) thickness, right ventricle (RV), interventricular septum thickness (thickness of the IVS), ejection fraction (EF), blood flow velocity in the pulmonary valve (blood flow velocity in the PA valve), etc.
Normal indicators differ depending on the age and body weight of the child. Using this method, a pathology can be diagnosed that the doctor suspected or could not notice using an electrocardiogram, auscultation, palpation, percussion and general examination.
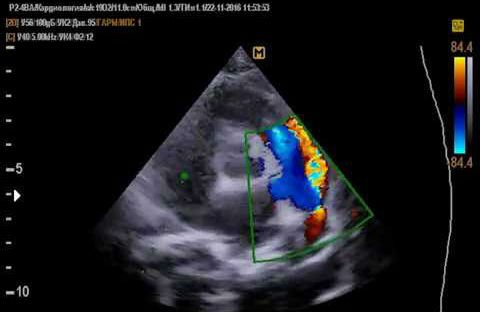
Cardiac ultrasound can diagnose:
- congenital heart defects (CHD): patent ductus arteriosus (PDA), IVS defect, mitral valve defects, aortic valve (AV);
- acquired heart defects;
- nature of noise;
- rhythm disturbances;
- minor cardiac anomalies: open foramen ovale, abnormally located chord of the left ventricle, etc.;
- enlargement of the heart chambers;
- hyper-, hypotrophy of the heart;
- blood clots in the cavities of the heart chambers;
- myocarditis, endocarditis, pericarditis;
- neoplasms.
For what pathologies is the study repeated and how often?
An ultrasound of the heart and blood vessels in a young child is most often associated with the presence of congenital defects that were not diagnosed during pregnancy:
- Open Botallov (arterial) duct is a connection between the aorta and the pulmonary artery system, which ensured the removal of blood from the pulmonary circulation in the prenatal period. Normally, the formation should become sclerotic within 1 year.
- An open foramen ovale is a physiological opening between the atria, which should be eliminated in the first hours of a baby’s life.
- A ventricular septal defect is a pathological connection of the right and left ventricles, which, when interpreted by ECHO-CG, is characterized by the presence of blood discharge from the left half of the heart to the right with excessive load on the latter.
- Combined defects (tetralogy and pentade of Fallot), which consist of a defect of the interatrial and interventricular septum, hypertrophy (increase in size) of the right ventricle, altered origin of the great vessels. Such anomalies require early diagnosis and surgical correction.
- An abnormal attachment or the presence of an additional chord (muscle bundle) in the ventricular cavity.
The main causes of functional or organic murmur in the heart area are pathologies of the valve apparatus: stenosis and insufficiency.
Stenosis is characterized by narrowing of the lumen and deficient filling of the ventricles with blood. The compensatory reaction is hypertrophy of the muscular layer of the atrium. Insufficiency of the valve apparatus is characterized by the absence of complete closure of the valves. The pathology is associated with the presence of regurgitation - the reverse flow of blood into the atrium during contraction of the ventricles.
Treatment of congenital heart defects involves surgery within the first 3 years of life. Dynamic monitoring of health requires ultrasound examinations 2 times a year before surgery and 1 time a year after it until adulthood.
When might an ultrasound be needed?

Auscultation of the heart
The following reasons may be an indication for prescribing a cardiac ultrasound for a child:
- heart murmurs heard by the pediatrician during auscultation;
- trembling over the heart area, which can be felt not only by the doctor, but also by the child’s parents;
- child's complaints of discomfort in the heart area;
- infant refusal to breastfeed, sluggish sucking, screaming and crying while breastfeeding;
- blueness of the nasolabial triangle during feeding, screaming, crying, defecation;
- causeless coldness of the hands and feet;
- poor height and weight gain;
- frequent colds in the baby;
- fainting, presyncope;
- congenital heart defects (CHD) in close relatives.
Indications
The functioning of the cardiovascular system in a child of the first year of life differs from the functioning of the body of an adult.
Structural differences, which normally disappear before the age of two, are caused by the peculiarities of the intrauterine blood supply to the fetus by the umbilical arteries and veins during pregnancy. Warning symptoms that require an ultrasound of the heart in an infant are:
- Sluggish sucking, lack of appetite and frequent regurgitation are caused by insufficient blood circulation in the child’s body and a lack of energy in the muscle organs. In other words, the baby is exhausted and does not have the strength to actively suckle at the breast. Parents note poor weight gain.
- Deformations in the chest and heart (retractions and protrusions) are associated with an increase in the size of the organ with combined defects.
- Tachycardia (increased heart rate). The norm for infants is 120-160 beats per minute. An increase in heart rate is a compensatory reaction of the body when there is insufficient blood supply to tissues.
- Dyspnea (tachypnea) is characterized in children of the first year of life by a frequency of respiratory movements of more than 60 per minute with the involvement of additional muscles (intercostal and sternocleidomastoid muscles).
- Perioral cyanosis is a bluish tint to the area around the mouth. This symptom indicates cardiac or pulmonary failure. Depending on the appearance of cyanosis at rest or during physical activity (breastfeeding, crying), the severity of the disorders is determined.
Older children complain of chest pain, increased heart rate, swelling of the lower extremities, and periodic coldness of the hands and feet.
The basis for prescribing echocardiography for a child after an objective examination is the presence of:
- cardiac hump - a specific deformation of the chest;
- pathological intrathoracic murmurs (systolic, diastolic) with different conduction paths;
- systolic trembling of the chest in the area of the projection of the apex of the heart;
- expansion of the diameter of the heart - determined by percussion, indicating an increase in size of the organ.
In addition, the study is carried out for patients with a burdened family history (presence of congenital heart defects in relatives) and frequent diseases of the respiratory system.
Norms for newborns

Indicators of the cardiovascular system in newborns
All normal cardiac ultrasound indicators depend on the child’s body weight. There is a limit when children weighing up to 3.5 kilograms have the same standards, and children weighing up to 4.5 kilograms have different standards. We present a table that contains some indicators of the cardiovascular system in newborns.
| Indicators | Body weight up to 3.5 kg | Body weight up to 4.5 kg | ||
| Girls | Boys | Girls | Boys | |
| LV EDC | 1.5-2 cm | 1.7-2.2 cm | > 2.4 cm | > 2.5 cm |
| LA diameter | 1.1-1.6 cm | 1.2-1.7 cm | 1.2-1.7 cm | 1.3-1.8 cm |
| pancreas | > 1.3 cm | > 1.4 cm | > 1.4 cm | > 1.5 cm |
| MZhP thickness | > 0.5 cm | > 0.6 cm | 0.3-0.6 cm | |
| FV | > 75% | > 75 % | ||
| Blood flow velocity in the pulmonary valve | 1.4-1.6 m/s | 1.3 m/s | ||
Below are the normal values for left ventricular end-diastolic diameter (LV EDD), left ventricular posterior wall thickness (LV PWD), aortic diameter and left ventricular end-systolic size (LV ESD). End-diastolic diameter can be synonymous with end-diastolic dimension (EDD), the same applies to systolic diameter. Sizes vary depending on age.
| Age | LV EDD (mm) | LV TSV (mm) | LV ESD (mm) | Aortic diameter |
| 0-1 month | 13-23 | 2-5 | 8-16 | 7-13 |
| 1-3 months | 16-26 | 2-5 | 9-16 | 9-15 |
| 3-6 months | 19-29 | 3-6 | 11-20 | 10-16 |
| 6-12 months | 20-32 | 3-6 | 12-22 | 10-17 |
| 1-3 year | 23-34 | 3-7 | 13-22 | 11-18 |
| 3-6 years | 25-36 | 3-8 | 14-25 | 13-21 |
| 6-10 years | 29-44 | 4-8 | 15-29 | 13-26 |
| 11-14 years old | 34-51 | 5-9 | 21-35 | 15-30 |
For ease of viewing, below is a table of other indicators in children according to age: thickness of the interventricular septum in diastole (IVSD), left atrium diameter (LA diameter), thickness of the middle wall of the right ventricle (RV MW), right ventricular diameter (RV diameter).
| Age | TMZhPd | LA diameter | TSS PZhd | Pancreas diameter |
| 0-1 month | 2-6 | 9-17 | 1-3 | 2-13 |
| 1-3 months | 2-6 | 10-19 | 1-3 | 2-13 |
| 3-6 months | 2-6 | 12-21 | 1-3 | 2-14 |
| 6-12 months | 2-6 | 14-24 | 1-4 | 3-14 |
| 1-3 year | 2-6 | 14-26 | 1-4 | 3-14 |
| 3-6 years | 3-7 | 15-27 | 1-4 | 4-15 |
| 6-10 years | 4-8 | 16-31 | 1-4 | 5-16 |
| 11-14 years old | 5-8 | 19-32 | 1-4 | 7-18 |
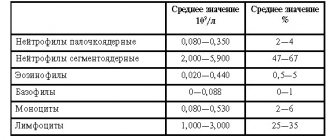
When performing an ultrasound of the heart in children, the doctor determines blood flow rates, which have their own norms. In children they are higher than in adults:
- transmitral blood flow (blood flow through the mitral valve) - 0.8-1.3 m/sec,
- transcuspid blood flow - 0.5-0.8 m/sec,
- transpulmonary blood flow (blood flow through the pulmonary valve) - 0.7-1.1 m/sec,
- blood flow in the terminal cardiac sections is 0.7-1.2 m/sec.

Normal heart ultrasound readings
The norms for a 14-year-old child on cardiac ultrasound correspond to those for an adult:
- The end-diastolic size of the left ventricle is 4.5-5.5 cm;
- The end-systolic size of the left ventricle is 3-4.3;
- Myocardial mass: girls - about 100 g, boys - about 300 g;
- The thickness of the LV wall in diastole is 1.1 cm;
- Ejection fraction - 55-60%;
- The diastolic size of the right ventricle is 0.95-2 cm;
- Left atrium - 1.85-3.31 cm;
- Aorta diameter - 1.8-3 cm;
- Stroke volume - 60-110 ml;
- Blood flow speed in the common carotid artery is 16.89-27 cm/sec;
- The speed of blood flow in the vertebral artery is 7.9 -18.1 cm/sec.
Features of CVS in children
The cardiovascular system of children differs significantly from the cardiovascular system of adults. The difference is clearly visible both during a routine examination and according to the results of electrocardiography (ECG). These differences greatly frighten parents and force them to urgently consult a doctor. Therefore, in this article we will try to consider all the main features of the cardiovascular system in a child, which may cause concern to his parents.
The cardiovascular system of children has its own anatomical and physiological characteristics compared to the cardiovascular system of adults. For example, when compared with the total body weight, the heart of a newborn is much larger than the heart of an adult, and rapid growth is observed, and by about three years the heart weight increases almost 3 times, and by 6 years almost 11 times.
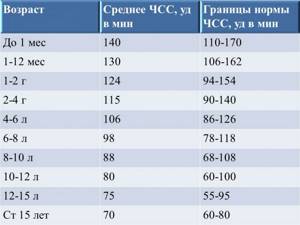
Due to the peculiarities of the nervous regulation of the heart and the high intensity of metabolism, the heart rate in children is much higher than in an adult, and only by about 15 years does the heart rate become like that of an adult. The decrease in heart rate (HR) with the age of the child is directly related to the onset of the influence of the vagus nerve on the heart.
In addition, sex differences in heart rate are noticeable in children. So, boys have a lower heart rate than girls.
But the main feature of the heart in a child is respiratory arrhythmia, which is manifested by an increase in heart rate during inhalation and a slowdown during exhalation. In early childhood, arrhythmia is slightly expressed, and from preschool age to 15 years, respiratory arrhythmia is expressed to a significant extent. In children over 15 years of age, as a rule, only isolated cases of respiratory arrhythmia occur.
The heartbeat in young children is very pronounced. This is due to the small amount of subcutaneous fat. As the child ages, subcutaneous fat increases, as a result the heartbeat becomes almost invisible.
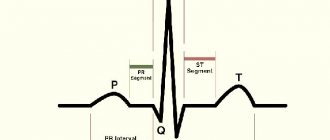
The electrocardiogram of a child and an adult has significant differences. First of all, arrhythmia, and secondly, due to the active growth and development of the heart muscle and conduction pathways, changes in the QRS complex are possible, which are manifested by splitting and narrowing of the complex. ECG conclusion: incomplete blockade of the left or right bundle branch.
In addition, all ECG waves are more pronounced in children than in adults. Migration of the pacemaker through the atria may occur, which is due to the formation of new short-term sources of excitation.
In older children, remodeling of the conduction system of the heart occurs, which causes the development of cardiac arrhythmias.
The most common diseases of the cardiovascular system in children
1. Congenital heart defects (CHD) are defects in the structure of the heart cavities or heart vessels, which lead to disruption of their functioning. Congenital defects are most often recorded either on ultrasound during pregnancy or in the first month after birth. Children with congenital heart disease experience rapid fatigue, weakness, small increase in height and weight in the first year of life, and frequent respiratory diseases. Most often, surgical treatment of defects is required.
2. Arterial hypertension. Almost 20% of schoolchildren experience increased blood pressure. Children of prepubertal and pubertal age are most predisposed to increased blood pressure. Depending on the age when the increase in blood pressure first appeared, there may be various reasons. In younger people, increased blood pressure is associated with congenital pathology of the kidneys and cardiovascular system. As you grow older, increased body weight, heredity, etc. take first place among the reasons. Very often, the child does not feel the increased pressure and it is an accidental finding during medical examination. Sometimes children may complain of fatigue, dizziness and headache. At the first stage of treatment, non-drug methods are used, which include normalizing the daily routine, sleep, nutrition and physical activity. If positive dynamics are not observed for some time, then medications are added.
FOR REFERENCE!
Nekrasova Anastasia Mikhailovna.
Doctor – pediatrician, pediatric cardiologist.
Medical
Elektrougli, st. Shkolnaya, no. 49, no. 38.
www.family-mts.rf
Decoding the results

Interpretation of ultrasound results
After performing an ultrasound of the child’s heart, the functional diagnostics doctor makes his conclusion. Next, with this conclusion, the little patient is examined by the attending physician. It is he who interprets the results of cardiac ultrasound, comparing clinical data. Such a complete picture allows you to draw the right conclusion and make the correct diagnosis. The attending physician chooses the treatment tactics that are optimal in each specific case. Being a simple method, ultrasound has a number of advantages and disadvantages:
- Safety. Ultrasound examination is not dangerous for children of all ages and can be repeated.
- Painless.
- High information content and reliability of the results. Using this method, more than 70 percent of various pathologies are detected.
- Availability.
- Speed of implementation.
- Lack of special training. To conduct the study, no special diet or regimen is required.
- No radiation exposure.