The birth of a healthy child is the natural desire of every pregnant woman. But, unfortunately, hopes for happy motherhood are not always justified. About 5% of newborns have various congenital diseases. Screening in the 1st and 2nd trimesters of pregnancy allows you to determine how high the risk of congenital pathology is in the unborn child.
Currently, there are quite effective methods for prenatal (prenatal) diagnosis of many fetal diseases that can be detected from the 11th week of pregnancy. Timely screening examinations make it possible to identify a wide range of fetal pathologies and see ultrasound signs of chromosomal abnormalities.
Scheduled ultrasound at 12 weeks
Ultrasound at the 12th week of pregnancy is the first routine examination of the expectant mother, during which you can see a lot.
Firstly, after an ultrasound at 12 weeks, the gynecologist will be able to accurately diagnose the gestational age, determine the size of the fetus, and its correct formation and development. An ultrasound at 12 weeks of pregnancy allows you to calculate the heart rate of your unborn baby, which is also an important diagnostic indicator. At a routine diagnosis (10-12 weeks), the fetus is already mature enough for a specialist to assess its health status and indicators of proper development, as well as confirm that the pregnancy process is proceeding without pathologies and the child is not in danger. The size of the developing fertilized egg and the embryo inside it determines the gestational age, the state of the amniotic fluid, and the uterine epithelium.
What is assessed during ultrasound in the 1st trimester
Coccygeal-parietal size (CPS) of the fetus
This indicator accurately determines the gestational age (pregnancy), especially if a woman does not remember the 1st day of her last menstruation, or if her menstrual cycle is not regular. In conclusion, the gestational age is set according to the fetal calf temperature, and not according to the date of the last menstruation.
Correct measurement of fetal CTE
Markers of chromosomal pathology:
- nuchal translucency thickness (TN) is the main sign of chromosomal pathology in the fetus. A pathological value is considered to be an increase in TVP greater than the 95th percentile for each gestational age. Each increase in TVP increases the risk of a chromosomal abnormality in the fetus.
TVP is normal TVP is pathological
It is important to understand that an increase in TVP is a sign (marker), but not an accurate diagnosis of chromosomal abnormalities in the fetus. Only invasive diagnostics followed by genetic analysis can determine the presence of Down syndrome and other diseases in an unborn child.
- nasal bone. In fetuses with Down syndrome, the nasal bone may be absent or reduced in size (hypoplastic). Very rarely, this can occur in completely healthy children. An accurate diagnosis can only be established using genetic analysis.
Normal nasal bone Absent nasal bone
- blood flow in the ductus venosus is a small vessel in the fetal liver. With reverse (retrograde) blood flow in this vessel, it can be assumed that the fetus has a chromosomal syndrome or a congenital heart defect.
Normal blood flow in the ductus venosus
But it is important to correctly obtain this blood flow and evaluate it. This requires certain skills and qualifications of a doctor, which are confirmed by annual FMF certification.
- blood flow through the tricuspid valve into the fetal heart. Here, retrograde (reverse) blood flow also indicates a chromosomal pathology, or can manifest itself in congenital heart defects.
Anatomical structures of the fetus and exclusion of major congenital defects
Fetal hand Fetal brain in the form of a “butterfly” is normal
Cervical length
Walls of the uterus and appendages (ovaries)
Blood flow in the uterine arteries
Ultrasound can be performed either transabdominally or transvaginally.
Indications for unscheduled ultrasound
Typically, the first planned ultrasound is scheduled at 10-12 weeks of pregnancy. But if the expectant mother or the gynecologist suspects the development of pathology, then an ultrasound examination is prescribed much earlier.
Indications for unscheduled ultrasound in early pregnancy:
- with artificial insemination
- threat of miscarriage detected
- uterine cancer
- identification of a serious chronic disease
- frozen pregnancy
Ultrasound in the first trimester is performed for the purpose of:
- Confirming the fact of intrauterine pregnancy and determining the site of fetal implantation in the endometrium
- Exceptions for ectopic pregnancy
- Definitions of term
- Diagnosing multiple pregnancy
- Exceptions for frozen pregnancy and hydatidiform mole
- Monitoring the dynamics of embryo development and its compliance with generally accepted standards
- Detecting the threat of miscarriage due to pathological hypertonicity of the uterus
- Diagnosing abruption of the ovum
- Tracking the size of the corpus luteum in the ovary
- Detection of pathology of female reproductive organs
Determining the thickness of the collar space
Ultrasound examination, which allows you to determine the likelihood of having a child with Down syndrome. We are talking about the accumulation of subcutaneous fluid on the back of the fetal neck, which is measured at 11-13 weeks. Some fluid is present in every case, but in many children with Down syndrome the amount is much higher than normal. An accurate diagnosis can only be made on the basis of additional studies: chorionic villus biopsy or amniocentesis. However, their implementation carries a small risk of miscarriage.
Determining the thickness of the nuchal translucency does not provide an accurate picture of the child's condition, but it helps determine whether a more in-depth diagnostic test is required.

Thickness determination should be carried out at 11 to 13 weeks plus 6 days. Before this time, it will be difficult to complete it, because the child is still too small, and later the excess fluid is absorbed by his lymphatic system. As a rule, measurements are carried out in the usual way, only sometimes a vaginal ultrasound is required.
In order to accurately determine the gestational age, the ultrasound doctor measures the fetus from the crown to the tailbone (this is called the coccygeal-parietal size KTR). Then the doctor determines the thickness of the collar space. In this case, the skin appears on the monitor as a white line, and the subcutaneous fluid appears as a black line.
At the 11th week of pregnancy, the norm is 1-2 mm, and at 13 weeks and 6 days - 2.8 mm. The thickness of the collar space increases in proportion to the growth of the child. A high reading does not always indicate a problem. In some children who are not predisposed to Down syndrome, the subcutaneous fluid content is sometimes higher than normal. Nine out of ten children with an indicator of 2.5-3.5 mm are born absolutely normal.
The higher the nuchal translucency thickness, the higher the risk of developing Down syndrome and other chromosomal disorders.
Every woman has a chance of having such a child, and it increases with age. To determine the degree of risk, the age of the expectant mother and the result of a test to determine the thickness of the collar space are taken into account. A special program helps determine this probability for a woman of a certain age - it is called the background indicator. Personal indicators are used to determine the degree of risk in each specific case. This degree may be higher or lower than the background level.
Most high-risk women give birth to healthy children. A child with Down syndrome occurs in one in 150 high-risk cases or even less often. In a situation where the risk is so high that it is 1 in 5, it is worth remembering that there is still a four to one chance that the baby will be born healthy. The only way to accurately diagnose the likelihood of chromosomal abnormalities is with a diagnostic test such as chorionic villus sampling or amniocentesis.
One of the advantages of the nuchal translucency test is that it is done early in pregnancy. Therefore, chorionic villus sampling (CVS) can also be done in the first trimester.
In 75% of children suffering from Down syndrome, abnormalities were identified during a study of the thickness of the nuchal translucency.
Sometimes measurements show the likelihood of a defect in healthy children. This result is called a false positive, it is 5% of the total. Thus, one in 20 women is mistakenly identified as having a high risk of having a child with disabilities. The most accurate result can be obtained by combining the results of a test to determine the thickness of the nuchal translucency and a blood test. The latter detects the level of free beta-hCG and the concentration of PAPP-A protein (pregnancy-associated plasma protein A). Children with Down syndrome typically have high levels of free beta-hCG and low concentrations of PAPP-A protein. Ultrasound to determine the thickness of the nuchal translucency in combination with a blood test in 90% of cases gives an accurate result. This test is called a double test.
What does an ultrasound show?
For an expectant mother, an ultrasound at 12 weeks of pregnancy is also interesting because you can see your baby on the monitor. The child is very small, but can already suck the thumb of his small hand, and it is quite possible that you will be able to see it. For a gynecologist who is caring for a woman’s pregnancy, an ultrasound examination at the 12th week of pregnancy will show the condition of the pregnant woman’s uterus, the place of placenta attachment and the state of vaginal muscle tone will be determined. During pregnancy ultrasound, much attention is paid to examining the occipital region of the fetus, since thickening of the nuchal translucency space can be a bad sign and indicate a developmental defect.
An ultrasound at 12 weeks of pregnancy will also show the number of fetuses in the uterus. All established indicators will subsequently serve as the basis for monitoring the correct development of the fetus. At this stage of a woman’s pregnancy, the obstetrician-gynecologist will be able to draw a conclusion about how the pregnancy process will proceed, whether there are complications, and, if necessary, make appropriate appointments.
What is early prenatal screening and when is it performed?
Screening (from the English “sifting”) is a set of studies that allows us to identify groups of pregnant women who are at risk of having a child with chromosomal abnormalities and congenital defects. But early screening is only the initial, preliminary stage of the examination, after which women with an identified risk of congenital anomalies are recommended to have a more detailed diagnostic examination that will accurately confirm or exclude the presence of pathology.
This diagnostic complex is carried out for pregnant women at a period of 11–13 weeks + 6 days (when the coccygeal-parietal size of the fetus is from 45 to 84 mm). The most optimal time for screening is considered to be from 12 to 13 weeks, since such an examination evaluates both the signs of chromosomal pathology in the fetus and the anatomical structures of the unborn child, and at a period of 11 weeks - 11 weeks + 4 days it is very difficult to do this .
What does early prenatal screening include?
A comprehensive examination includes:
- Ultrasound of the fetus for the presence of markers (signs) of chromosomal pathology and congenital malformations;
- determination of the level of biochemical markers of chromosomal abnormalities in the blood of a pregnant woman: beta-hCG and PAPP-A. The study is carried out on special high-tech equipment Cobas e, Roshe, approved for calculating the risk of chromosomal syndromes in the Astraia (FMF) program;
- Doppler ultrasound of the uterine arteries
- cervicometry – measurement of the length of the cervix;
- collecting anamnesis (age, height, weight, number of pregnancies and births, smoking, diabetes, arterial hypertension, etc.);
- measuring blood pressure in both arms.
The data obtained: medical history, ultrasound and biochemical markers are placed in a specially developed Astraia program, which calculates the risk of having a child with congenital anomalies. The combination of these studies increases the efficiency of identifying fetuses with Down syndrome and other chromosomal diseases.
How is an ultrasound performed at 12 weeks?
There are two ways to do an ultrasound at 12 weeks of pregnancy:
- transvaginal, or internal - the sensor is passed through the vagina;
- transabdominal, or external - examination is carried out through the anterior abdominal wall.
The transvaginal method is the most accurate because the sensor is as close to the uterus as possible. This allows you to see all parts of the fetus when its size does not exceed 5 cm. The technique does not require special preparation; it is enough to carry out ordinary hygiene measures.
Transabdominal ultrasound - The study is performed using a standard technique, in which the diagnostician applies a water-soluble gel to the surface of the skin in the pelvic area and moves the emitter along the projection of the uterus. At the same time, the gel allows you to make the procedure as comfortable and informative as possible - it reduces friction and ensures full contact between the skin and the sensor.
This examination is absolutely painless and can be done at any time convenient for the woman. The only thing the patient must do is prepare for the procedure, namely, fill the bladder for optimal visualization. To do this, you will need to not urinate for 1.5–2 hours or drink about half a liter of still water no later than 30 minutes before.
The choice of method remains with the doctor, and it can be influenced by many things, including the physique of the expectant mother herself. If a woman is overweight and has a noticeable layer of fat on her stomach, then it is most likely that the doctor will choose the vaginal method of examination. Thin patients are more likely to undergo an abdominal ultrasound at this time. In some cases, the doctor may use both methods.
Sign up for a study with a discount:
How long does this procedure take?
No more than 20 minutes if the embryo is healthy. More time is required if any pathologies are detected.
Does this procedure (ultrasound) cause any harm to the woman or the embryo?
The harm of ultrasound is reduced to zero if the time regulations are followed. For example, if a woman is watched for an hour or more, this is unacceptable. To minimize harm, exposure (duration) is important, not the frequency of ultrasound. For a qualified specialist, 30 minutes is enough to look at the norms or pathologies. Modern devices allow you to archive cine loops, record videos, and view 3D files, so no additional time is required for ultrasound examination even if pathology is detected.
Screening
informs the woman as fully as possible about the condition of the child, each of its organs and all systems.
Each ultrasound examination in our center is recorded on video; if a woman wishes, she can take it for her home archive completely free of charge. This is not only informative for analyzing the baby’s condition, but also very exciting for the family. The ultrasound examination is accompanied by doctor's comments, three-dimensional and four-dimensional images. If 3D is beautiful and informative pictures, then 4D is more of an animated film. Often children in the womb make dance movements, you can watch this an infinite number of times, it is very beautiful.
The 3D files contain information about the state of the child’s brain, heart and appearance. The files are divided into 12-14 windows, which allows you to study details in different planes. If in a regular two-dimensional image many pathologies can simply not be seen, then a three-dimensional image allows you to see, for example, the fissures of the heart, anomalies in the development of brain or facial structures. Such diagnostics are carried out in 3D using modern presets, which are presented in our clinic.
Norms and interpretation of results
The final week of the first trimester of pregnancy perfectly demonstrates the peculiarities of the evolution of an embryo ready to move into a new stage of development. The data is compared with a table of normative values corresponding to the 12th week of embryonic development. Deciphering screening data starts with analyzing the results of ultrasound diagnostics - these are:
- Bipareital head size (BPR) is the distance between the temples, the so-called width is about 21 mm.
- Coccygeal-parietal size (CPS) - the length of the fetus from the crown to the coccyx is on average 51 mm (can vary from 43 to 59, which will also be the norm).
- The thickness of the collar zone (TVR) should be within the range of 0.71–2.5 mm. An indicator of 2.7 is considered critical and indicates the presence of Down syndrome.
- The child's height at this stage of development should be approximately 8–9 cm.
- Weight – normal body weight is 17–19 g.
- Thigh length (HL) – normally can range from 7 to 9 mm.
- Chest diameter (CHD) – the average value is 24 mm.
The development of tubular bones and the circumference of the fetal abdomen are analyzed. Deviations may indicate an incorrect determination of the gestational age if all indicators differ proportionally from normal values. Ultrasound standards contain average values. The interpretation should take into account the entire complex of data obtained during the diagnosis.
An important value that allows us to judge the duration of pregnancy and the rate of development of the baby is the size from the crown to the tip of the tailbone, the so-called coccygeal-parietal size, or CTE. This week's averages are presented below.
Table of CTE standards for the period 11-12 weeks and 12-13 weeks:
| Gestation period (week + day) | Coccygeal-parietal size (CTR), mm – normal | KTE – fluctuations within normal limits, mm |
| 11+1 | 44,7 | 38,6 – 50,8 |
| 11+2 | 46,3 | 40,2 – 52,5 |
| 11+3 | 48,0 | 41,8 – 54,2 |
| 11+4 | 49,6 | 43,4 – 55,6 |
| 11+5 | 51,3 | 45,0 – 57,6 |
| 11+6 | 52,9 | 46,5 – 59,3 |
| 12 weeks exactly | 54,6 | 48,0 – 61,1 |
| 12+1 | 56,3 | 49,6 – 62,9 |
| 12+2 | 57,9 | 51,0 – 64,5 |
| 12+3 | 59,5 | 52,7 – 66,0 |
| 12+4 | 61,0 | 54,3 – 67,6 |
| 12+5 | 62,6 | 55,7 — 69,5 |
| 12+6 | 64,0 | 57,1 -71,0 |
The thickness of the collar space and the length of the nasal bones at 12 weeks:
| Gestational age | TVP, mm | Nose bones, mm |
| 11 -12 weeks | 1.6 (fluctuations from 0.8-2.4) | 2.3 (fluctuations from 1.8 to 2.9) |
| 12-13 weeks | 1.6 (fluctuations from 0.8-2.5) | 2.4 (fluctuations from 1.8 to 3.1) |
Condition of the uterus
At 12 obstetric weeks, an ultrasound scan must measure the length of the cervix, which normally should be approximately 30 mm. The size of 20 mm is considered critical. Under such circumstances, the pregnant woman is prescribed bed rest, in more severe cases hospitalization, and sometimes even surgical intervention may be required. During this period, the condition of the muscular layer of the uterus is also assessed. When hypertonicity is diagnosed, which can lead to spontaneous abortion - miscarriage, therapeutic measures are prescribed on an outpatient basis or in a hospital setting.
The thickness of the placenta must be measured. Its abnormal growth may also indicate either infection of the fetus or genetic pathologies. Normal values for this period are from 14.5 to 15.5 mm.
Gender of the child
Starting from 10-12 weeks, during an ultrasound, a specialist can determine the baby’s gender. The doctor can find out whether it is a boy or a girl visually, because female or male genitalia, as a rule, are already quite well formed.
There is still a possibility of an error at week 12, which is due to the peculiarities of intrauterine development. Sometimes an ultrasound specialist may confuse the penis with a loop of the umbilical cord, and swollen labia with the scrotum. More accurate results on gender identification using ultrasound can be expected at 23-25 weeks of pregnancy.
Possibilities of fetal echocardiography in the first trimester of pregnancy (11-14 weeks)

Ultrasound machine HM70A
Expert class at an affordable price.
Monocrystal sensors, full-screen display mode, elastography, 3D/4D in a laptop case. Flexible transformation into a stationary scanner with a cart.
Introduction
The relevance of the topic of prenatal diagnosis of congenital heart defects (CHD) is clear to all doctors who are involved in prenatal diagnosis, neonatology, pediatrics, cardiology, and genetics. CHDs are one of the leading causes of perinatal mortality and are registered with a frequency of 4-13 per 1000 live births [1]. Due to the fact that preventive measures to prevent congenital heart disease are not sufficiently successful, their prenatal ultrasound diagnosis seems relevant and necessary.
Numerous studies by foreign and domestic colleagues have repeatedly formulated and studied various risk groups for the occurrence of congenital heart disease. This was done to potentially narrow the group of pregnant women eligible for echocardiography at a tertiary center. Among these risk groups were:
- Families with a child with congenital heart disease.
- Families with congenital heart disease in one or both spouses.
- Women suffering from diabetes, systemic connective tissue diseases, hypothyroidism.
- Pregnant women with teratogenic exposure in early pregnancy (herpes before the 6-7th week) [2].
However, in parallel, other scientists rejected these risk groups, because most congenital heart diseases occurred in fetuses and children whose mothers were not included in any of the proposed risk groups. The only reasonable criteria for the so-called selective selection were recognized as pregnant women who were at risk after screening in the first trimester and pregnant women with suspected congenital heart disease during ultrasound examination of the fetus [3].
It is undeniable that the optimal period of pregnancy for studying the fetal heart is 20-22 weeks, however, most lethal and clinically significant heart defects can be diagnosed at the end of the first trimester of pregnancy. Let us quote the words of the head of the Fetal Medicine Foundation, Kipras Nicolaides, expressed on the pages of the FMF website (www.fetalmedicine.com): “An ultrasound specialist should assure most parents from the 12th week of pregnancy that their child does not have major congenital heart defects. In the case of large congenital heart defects, early detection can lead to a correct diagnosis or at least raise suspicion for ultrasound monitoring.”
The main goal of prenatal diagnosis has been formulated by prenatal diagnostic specialists around the world - to provide women with the maximum possible information about the defect as early as possible. We must give the woman and the family as a whole the right to decide on prolonging pregnancy with gross malformations in the fetus [4].
Every year, an increasing number of publications are devoted to the diagnosis of congenital heart disease in the early stages - in the first trimester of pregnancy [5-8]. Almost none of the issues of the ISUOG journal (Ultrasound In Obstetrics and Gynecology, or the “white” journal, as experts call it) ignores the topic of early diagnosis of congenital malformations.
The most famous website in the world of prenatal diagnostics, www.thefetus.net (Philippe Jeanty, USA), has already published more than 30 cases of congenital heart disease in the first trimester of pregnancy. However, in Russian periodicals there are only a few works on this topic. All of them belong to the “pen” of prenatal diagnostic specialists of the Russian Association of Ultrasound Diagnostics in Perinatology and Gynecology, although for many specialists, both before and now, examination of the fetal heart at 11-14 weeks consists only of ascertaining the number of heartbeats.
The purpose of echocardiography in the first trimester of pregnancy is to identify fatal and clinically significant congenital heart disease. This study does not aim to identify stenoses and hypoplasias of the outflow tracts, diagnose minor septal defects, pathologies of the aortic arch and ductus arteriosus. Many of these defects are not only technically impossible to suspect in the first trimester, they manifest themselves after the 30th week of pregnancy, i.e. their diagnosis is the prerogative of research in the third trimester.
The accuracy of prenatal diagnosis of congenital heart disease at all stages of pregnancy varies widely. The reasons for this may be different experience of specialists, obesity of the pregnant woman, frequency of ultrasound transducers used and class of ultrasound machine, previous abdominal surgeries, gestational age, amount of amniotic fluid and fetal position. However, we note that many of these factors lose their relevance precisely when transvaginal echocardiography is performed in the first trimester of pregnancy. Timely diagnosis of congenital heart disease makes it possible to identify high-risk fetuses based on genetic syndromes, which is important during prenatal counseling and has a significant impact on obstetric tactics.
results
From 2006 to 2011, 125 congenital heart diseases were detected prenatally in the first trimester of pregnancy. Of these, 68 (55%) CHDs were combined with various chromosomal anomalies (CA) of the fetus, 30 (24%) were part of various multiple congenital malformations (MCDM), 27 (21%) CHDs were isolated.
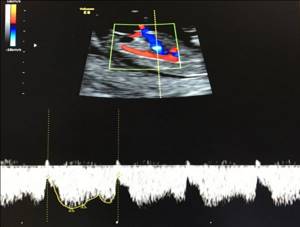
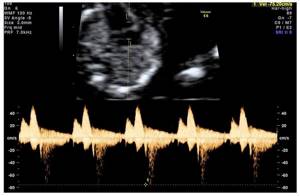
Echocardiography examined a four-chamber section of the fetal heart (Fig. 1) and a section through three vessels (Fig. 2). Ultrasound was performed with a transabdominal sensor; only when necessary (difficult visualization) was an intracavitary sensor used. A four-chamber section of the fetal heart during ultrasound scanning with a transabdominal sensor was visualized in 85% of cases, a section through the vessels - in 73%, when using a transvaginal sensor, these figures increased significantly to 100 and 91%, respectively. Optimization of prenatal diagnosis of congenital heart disease can be achieved through strict adherence to basic methodological rules. When assessing a four-chamber section of the fetus, it is necessary to evaluate the normal location of the fetal heart, excluding its ectopia (Fig. 3), the position of the axis of the fetal heart, which does not present any difficulties, the normal proportions and sizes of the chambers of the heart, the movement of the atrioventricular valve leaflets should be free, the septal leaflet of the tricuspid the valve should be located closer to the apex of the heart (Fig. 4). When assessing a section through three vessels, it is necessary to evaluate the relative position of the vessels and their diameter.

Rice. 1.
Pregnancy 12 weeks. Four-chamber section of the fetal heart. The chambers of the heart are clearly visible.

Rice. 2.
Pregnancy 12 weeks. Section through three vessels. The aorta and pulmonary trunk are visualized. The vessels are located in one line and have normal sizes.

Rice. 3.
Pregnancy 8 weeks. Ectopia of the heart. The heart is located outside the chest cavity.

The case was published on the website www.thefetus.net.

Rice. 4.
Pregnancy 13 weeks. Four-chamber section of the fetal heart. The chambers of the heart are clearly visible. Position of atrioventricular valves.
Advanced echocardiography involves the use of additional modes and sections - a section through the aortic arch (Fig. 5), a section through the outflow tract of the left ventricle (Fig. 6), a CD mode (Fig. 7), pulse Doppler, STIC technology (Fig. 8-11 ). This examination is carried out when abnormal screening projections of the fetal heart are detected, markers of CA [widening of the thickness of the nuchal space - TVP, hypoplasia/absence of the nasal bone (Fig. 12, 13), regurgitation in the ductus venosus (Fig. 14), tricuspid regurgitation (Fig. 15 )] and/or congenital malformations of the fetus.

Rice. 5.
Pregnancy 13 weeks. Section through the aortic arch. Three brachiocephalic vessels extending from the arch are clearly visible.

Rice. 6.
Pregnancy 12 weeks. Tetralogy of Fallot. Color flow mode. Section through the left ventricular outflow tract. The “equestrian aorta” is visible, sitting above the VSD. The case was published on the website www.thefetus.net.

Rice. 7.
Pregnancy 13 weeks. Double exit of vessels from the right ventricle. Color flow mode. Parallel exit of vessels from the right ventricle.
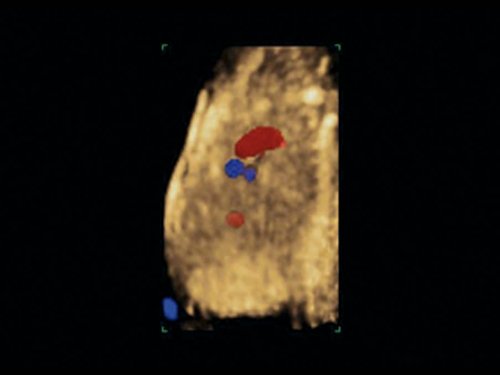
Rice. 8.
Pregnancy 12 weeks. Atrioventricular communication (AVC) in Down syndrome. STIC mode.

Rice. 9.
Pregnancy 12 weeks. Tetralogy of Fallot. STIC mode. The “horsewoman” aorta sits above the VSD. The case was published on the website www.thefetus.net.

Rice. 10.
Pregnancy 13 weeks. Transposition of the great vessels. STIC mode. A parallel course of efferent vessels is visible, the upper of which leaves the left ventricle and divides into a bifurcation (pulmonary artery).
Rice. eleven.
Pregnancy 12 weeks. Common arterial trunk. STIC mode. A single efferent vessel of two ventricles is visible.

Rice. 12.
Pregnancy 11.4 weeks. Multiple markers of CA. Patau syndrome (trisomy 13). Increased TVP, abnormal profile with hypoplasia of the nasal bone, protuberance on the upper jaw (a sign of a cleft face), polydactyly. The fetus was diagnosed with hypoplasia of the left heart.

Rice. 13.
Pregnancy 12 weeks. Multiple markers of CA. Down syndrome (trisomy 21). Increased TVP, abnormal profile with nasal bone hypoplasia. AVC was detected in the fetus.

Rice. 14.
Pregnancy 12 weeks. Reverse blood flow in the ductus venosus in a fetus with heterotaxy.
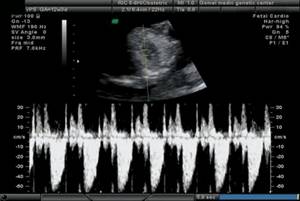
Rice. 15.
Pregnancy 12 weeks. Tricuspid regurgitation in a fetus with a common truncus arteriosus.
The nosology of the congenital heart diseases we identified was as follows:
- hypoplastic left heart syndrome (HLHS) - 29 cases (Fig. 16);
- atrioventricular communication (AVC) - 23 (Fig. 17, 18);
- ventricular septal defect (VSD) - 19 (Fig. 19);
- pathology of the great vessels - 19 (of which transposition - 3, double origin of vessels from the right ventricle - 2, tetralogy of Fallot - 5, common truncus arteriosus - 9);
- pathology of the right heart (pathology of the tricuspid valve) - 3;
- heterotaxy syndrome - 6;
- single ventricle - 4;
- ectopia of the heart - 7;
- combined forms of congenital heart disease occurred in 15 cases.

Rice. 16.
Pregnancy 13 weeks. Hypoplastic left heart syndrome in a fetus with Turner syndrome (45X). Single flow through the tricuspid valve. Shunting of blood into the hypoplastic left ventricle through the VSD.

Rice. 17.
Pregnancy 11.4 weeks. Four-chamber section of the heart. Single atrioventricular valve. There is no “cross” of the normal relationship between the atrioventricular valves and the heart septa.

Rice. 18.
Pregnancy 11.4 weeks. Four-chamber section of the heart. Color flow mode. Single atrioventricular valve.

Rice. 19.
Pregnancy 12 weeks. Color flow mode. Extensive VSD in a fetus with Edwards syndrome (trisomy 18).
When karyotyping fetuses with a prenatal diagnosis of congenital heart disease at 11-14 weeks, 68 chromosomal abnormalities were diagnosed:
- trisomy 21 (Down syndrome) was detected in 23 (34%) cases,
- trisomy 18 (Edwards syndrome) - in 19 (28%);
- trisomy 13 (Patau syndrome) - in 7 (10%);
- monosomy X (Turner syndrome) - in 6 (9%);
- triploidy - in 8 (12%);
- other chromosomal imbalances - in 5 (7%).
It should be especially noted that in 8 cases of detected CA, the indication for karyotyping was the identification of congenital heart disease. These fetuses had normal values for both TVP and nasal bone length.
In case of CA, the identified congenital heart disease according to nosology had the following features: in the majority of fetuses with Down syndrome, AVK and VSD were diagnosed; with Patau syndrome - GLOS and VSD; with Edwards syndrome - VSD, tetralogy of Fallot and OSA; with Turner syndrome - GLOS and aortic pathology - coarctation of the aorta in a typical place (Fig. 20).

Rice. 20.
Pregnancy 12 weeks. Section through the aortic arch. Color flow mode. Narrowing of the aorta in a “typical” location in a fetus with Turner syndrome (45X).
It is necessary to separately consider the issue of verification of ultrasound diagnosis. All pregnancies with isolated congenital heart disease in the first trimester were prolonged until the second trimester, when 100% morphological verification of the diagnosis is possible. In modern conditions, verification of diagnoses after termination of pregnancy in the first trimester is a rather significant problem. However, with specialized training of specialist morphologists, verification of congenital heart disease is also possible during termination of pregnancy in the first trimester (Fig. 21, 22). This undoubtedly depends on the quality of the material obtained, the qualifications of the morphologist and the special equipment required in some cases, as well as on the general methodological approaches to anatomical and morphological diagnosis, regardless of gestational age.

Rice. 21.
Pregnancy 13 weeks. Increased TVP in a fetus with hypoplasia of the left heart.

Rice. 22.
The same fruit. Morphological examination - hypoplasia of the ascending aorta and cystic cavities (marked by arrows).
Conclusion
From the above, the following conclusions can be drawn.
The fetal heart should be assessed in all pregnant women during a screening examination in the first trimester (11-14 weeks). Since the modern concept of the development of prenatal diagnostics within the framework of the “pilot” project of the Ministry of Health of the Russian Federation implies a screening examination in the first trimester by an expert doctor, it is he who should evaluate the fetal heart and suspect congenital heart disease at the end of the first trimester of pregnancy.
To exclude lethal and clinically significant cardiac pathology in the first trimester, it is necessary to evaluate the four-chamber projection of the fetal heart and the section through three vessels.
Extended echocardiography should be performed if abnormal screening projections of the fetal heart, markers of CA and/or fetal congenital malformation are detected.
If congenital heart disease is detected in the first trimester, fetal karyotyping is indicated.
Literature
- Office for National Statistics. Mortality statistics. Childhood, Infancy and Perinatal. Series DH3. Stationary Office: London, 2007; 40.
- Novikova I.V., Pribushenya O.V., Rumyantseva N.V. Formation of risk groups for prenatal diagnosis of congenital heart defects. Instructions for use. Minsk, 2004.
- Carvalho JS, Moscoso G, Tekay A et al. Clinical impact of first and early second trimester fetal echocardiography on high risk pregnancies. Heart. 2004; 90: 921-926.
- Becker R., Wegner R.-D. Detailed screening for fetal anomalies and cardiac defects at the 11-13 week scan. Ultrasound Obstet Gynecol 2006; 27; 613-618.
- Allan LD, Sharland GK, Milburn A. et al. Prospective diagnosis of 1,006 consecutive cases of congenital heart disease in the fetus. J Am Coll Cardiol 1994; 23: 1452-1458.
- Huggon IC, Ghi T, Cook AC et al. Fetal cardiac abnor-malities identified prior to 14 weeks' gestation. Ultrasound. Obstet. Gynecol. 2011; 20: 22-29.
- Persico N., Moratalla J., Lombardi CM et al. Fetal echocardiography at 11-13 weeks by transabdominal high-frequency ultrasound Ultrasound Obstet. Gynecol. 2011; 37: 296-301
- Allan LD Echocardiographic detection of congenitalheart disease in the fetus: present and future. Br. Heart. J. 1995; 74: 103-106.
Ultrasound machine HM70A
Expert class at an affordable price.
Monocrystal sensors, full-screen display mode, elastography, 3D/4D in a laptop case. Flexible transformation into a stationary scanner with a cart.
What pathologies are detected at 12 weeks of pregnancy?
Sometimes the test result differs from normal values. In this case, the gynecologist suspects a developmental anomaly and recommends that the woman undergo additional examination.
Signs of early pregnancy pathology:
- frozen pregnancy - the death of the embryo inside the fertilized egg, determined by the lack of embryo growth when examined at intervals of 1-2 weeks;
- CTE less than 6 cm - intrauterine growth retardation, genetic abnormalities;
- absence of nasal bones - Down syndrome;
- thickening of the cervical fold more than 2.4 mm - genetic abnormalities;
- a low location of the placenta indicates a risk of miscarriage or premature birth;
- the amount of amniotic fluid is more than 30 ml - intrauterine infection;
- decrease in biparietal size - fetal underdevelopment;
- increase in biparietal size - large fetus.
The diagnosis is not made by ultrasound alone.
Is it harmful to have an ultrasound at 12 weeks?
Ultrasound examination is a safe diagnostic method based on the use of ultrasonic waves produced by a special device. The waves, passing through the tissues and organs of the mother and fetus, return to the sensor, which transforms the received data into a digital image on the monitor screen.
Since different organs and tissues have different densities, when passing through them, waves of different lengths return to the device. The difference in wavelength will serve as the basis for reading the indicators.
Ultrasound is safe for mother and child; it does not affect the quality and composition of amniotic fluid and fetal membranes. Therefore, there are no restrictions on the number of procedures.