- Gynecological laparoscopy: indications for performance
- Advantages of the technique
- Laparoscopic surgery in gynecology: preparation for surgery
- Instruments and equipment for laparoscopy
- How laparoscopy is done in gynecology: procedure progress
- List of absolute and relative contraindications
- Rehabilitation period
- Diagnostic laparoscopy in gynecology: price
- Laparoscopy in gynecology: reviews from patients
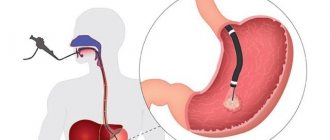
Laparoscopy in gynecology is a modern surgical technique that allows you to do without a layer-by-layer incision of the abdominal wall. Most gynecological operations, which were previously performed through open access, are now performed laparoscopically. Most often it is used for pathologies of the internal organs of the abdominal and pelvic cavity. Let us consider in more detail what is special about the technique and how it is implemented.
How are laparoscopic surgeries performed?
A tiny puncture (4-7 mm in diameter) is made in the navel area. Through it, a laparoscope is inserted into the pelvic cavity, previously filled with a special gas. This instrument looks like a thin tube and is equipped with a light and a tiny video camera at the end.
The laparoscope camera allows the doctor to see all the organs and tissues of the pelvis on a computer screen. The doctor can enlarge the image of each fragment on the screen 40 times to examine it in detail.
If a cyst, fibroid or other pathology is detected, which should not be in a healthy body, the doctor, using robotic instruments for laparoscopic surgery, which are inserted through the same puncture, can remove the formation or take a puncture for analysis.
Laparoscopy of ovarian cyst
A cyst is a pathological cavity (neoplasm) in organs or tissues that has a wall and contents. Follicular or functional cysts are hormone dependent. They appear at a certain period of the cycle and then resolve on their own. The situation is more complicated with endometrioid formations, which are amenable to conservative treatment only at the initial stage. If treatment is not timely, they grow and then merge (polycystic disease). This pathology rarely responds to conservative treatment; surgical intervention is required. Such tumors are characterized by rapid growth. This can threaten ovarian rupture (if the formation is located inside the organ), decreased chances of getting pregnant or infertility, atypia (transformation of benign cells into malignant ones).
Indications for laparoscopy of ovarian cysts.
- Large tumor size (more than 5 cm, when the formation puts pressure on regional tissues and organs and interferes with their functioning).
- The development of pathology inside the ovary, regardless of its size and growth. Untimely removal threatens rupture.
- Features of the structure. Formations on the stalk tend to twist under the influence of certain factors. As a result, tissue necrosis occurs.
- If cell malignancy is suspected.
“Keyhole surgery” is performed through three small punctures (1.5 cm in diameter) in the abdominal wall. To provide access to the lesion and avoid damage to nearby organs, the cavity is “pumped” with gas. An instrument is inserted through the third hole, which is used to perform excision or resection. After the tumor is removed, stitches are placed on the punctures. Advantages of laparoscopy for removal of ovarian cysts:
- minimal level of injury;
- shortened rehabilitation periods;
- aesthetic seams;
- no complications during surgery.
Preparation for planned laparoscopy
Before performing the study, the patient must undergo a number of tests:
- Determination of blood group and Rh factor;
- Blood chemistry;
- Clinical blood test;
- Blood for hepatitis B and C, HIV and syphilis;
- Coagulogram (test for blood clotting);
- General urine analysis;
- Study of vaginal flora;
- ECG.
In addition, patients who have concomitant pathologies should consult with specialists and, on the eve of surgery, with an anesthesiologist.
At the MEDICA reproductive and family planning center, after surgery, patients are kept in comfortable wards of a modern hospital, under the supervision of experienced and caring medical staff. Thanks to this, patients quickly recover and return to normal life.
Advantages of the technique
In modern gynecology, they are increasingly resorting to surgical interventions with abdominal tissue incision, giving preference to an improved technique - laparoscopy. Among its main advantages:
- short recovery period 7-14 days
- a large list of indications;
- absence of postoperative scars (decent cosmetic effect);
- minimal level of injury (access through small punctures rather than incisions);
- absence of severe discomfort and pain in the postoperative period;
- high information content compared to other diagnostic methods;
- minimal blood loss during the operation;
- preservation of reproductive function;
- quick implementation of the technique;
- minimal risks of complications.
- restoration of working capacity in a shorter time without compromising the quality of treatment
Determination of fallopian tube patency
Diagnosis of infertility necessarily requires checking the patency of the fallopian tubes. The laparoscopic method of such testing is called chromohydrotubation.
A tinted solution is injected into the uterine cavity and it is observed whether it passes through the tubes and at what speed. Depending on the results of the study, they decide what to do next.
Chromohydrotubation is a very important study, since often it is the obstruction of the fallopian tubes that prevents conception. Sometimes it is enough to remove adhesions so that patency is restored and conception occurs. If it is impossible to restore patency, the tubes should be removed so that pathological discharge from them does not interfere with IVF.
Technique for diagnostic laparoscopy. Information for specialists
Diagnostic laparoscopy in gynecology is performed under local anesthesia, intravenous or intubation anesthesia. The choice of anesthesia depends on the somatic and psychological state of the patient and the intended surgical tactics. However, relaxation of the muscles of the anterior abdominal wall is desirable, as it improves visibility and increases the diagnostic value of the procedure.
To examine and perform any manipulation in the abdominal cavity, it is necessary to create an adequate pneumoperitoneum. It is better to perform a puncture of the abdominal cavity in the umbilical region - the thinnest place on the anterior abdominal wall. The incision can be made either transversely or vertically, depending on the patient's skin folds and the surgeon's habits. Unlike some authors (Rozin D. et al.), we believe that the location of the incision does not affect the risk of developing purulent complications and the cosmetic effect. When inserting a Veress needle, equipped with a spring and a protective blunt tip, it is necessary to lift the anterior abdominal wall, using clothespins on each side of the navel as handles or grasping it with one hand in the fold. The method of performing this stage is not fundamental and individual; it is only important in the first case not to raise the anterior abdominal wall too high, since in this case the peritoneum and preperitoneal tissue shift downward, and it seems to thicken. By grasping the abdominal wall with your hand, it is possible to lift all its layers in the navel area. Palpation of the abdominal aorta in thin women helps to clarify the angle of needle insertion. In obese patients, the needle should be inserted vertically, and after passing through the peritoneum, it should be moved to an inclined position.
You can confirm the location of the needle in the abdominal cavity using a test with saline (a drop of liquid is applied to the hole of the Veress needle with the screw open), and then by measuring the intra-abdominal pressure using an insufflator (it should be less than 3-4 mmHg) . If the needle is in the abdominal cavity during a drop test, the liquid flows freely into it, otherwise it remains at the same level. Pressure at the beginning of insufflation above the specified norm serves as a signal of incorrect needle position, which may be caused by pressing the distal hole against the omentum or the inner surface of the anterior abdominal wall, closing it with stuck tissue when passing through the layers of the abdominal wall. This can be overcome by slightly lifting the anterior abdominal wall and moving the central part of the needle in different directions. If the measures taken are ineffective, a second attempt is made to insert the needle and inspect its tip.
Next, gas insufflation is performed until tympanitis appears on percussion. There are no specific guidelines for the amount of carbon dioxide introduced, usually about 3-4 liters are required. To avoid problems associated with impaired venous return, intra-abdominal pressure should not exceed 15 mmHg. This figure is set on the front panel of the insufflator and is constantly maintained.
If the presence of adhesions in the navel area is suspected, the needle should be inserted along the midclavicular line, 2 fingers below the angle of the costal arch, or use the technique of open insertion of the first trocar, proposed in 1971 by N.M. Hasson. In the latter case, an incision is made in the umbilical area and, under eye control, the aponeurosis is dissected so much that after insertion of the trocar it covers the instrument hermetically. Then one suture is placed on the aponeurosis on both sides. It is possible to use a video trocar “Visiport” (“Auto suture”, USA), which has an automatically ejecting blade-knife, which, under visual control, cuts tissue to a depth of 1 mm. As the tissue is dissected and separated while advancing the optical trocar, the surgeon is able to identify the different layers of the abdominal wall, the organs adjacent to the transparent peritoneum, and the degree of their fixation to it.
After applying pneumoperitoneum, a 5- or 10-mm trocar is inserted into the abdominal cavity through the same incision, lifting the abdominal wall by the hooks or by hand, depending on the diameter of the laparoscope used. Undoubtedly, the perpendicular position of the instrument in relation to the anterior abdominal wall will provide the greatest range of movements of the laparoscope. It is important to remember that below the insertion site of the main trocar there are vital anatomical structures. These are the aortic bifurcation, internal and external iliac vessels, infundibulopelvic vessels and ureters, which pass over the external iliac arteries. In this regard, V.I. Kulakov et al. recommends inserting the trocar at an angle of 45-60° to the plane of the anterior abdominal wall in the direction of the sacral cavity. Fixing the surgeon's index finger on the trocar cartridge helps limit the depth of its penetration. In addition, the use of tools equipped with springy protective petals will increase the safety of manipulation. To reduce the likelihood of injuries associated with “blind” insertion of the main trocar, J. Hulka, H. Reich, G. Phillips proposed a technique using high-pressure pneumoperitoneum (up to 30 mmHg), which is reduced immediately after confirming the atraumaticity of penetration into the abdominal cavity.
The introduction of additional trocars for manipulators is carried out under endovideo control, as a rule, lateral to the rectus abdominis muscles. You should remember the topography of the lower epigastric vessels, injury of which is accompanied by significant bleeding. They pass in the lateral umbilical ligament, which forms the lateral umbilical fold of peritoneum on the anterior abdominal wall. In the lower abdominal wall, the epigastric vessels pass lateral to the rectus abdominis muscles. Approximately halfway along the anterior abdominal wall, they pass under the rectus abdominis muscles, approximately from the level of the navel passing along their midline. To avoid injury to the inferior epigastric vessels, suprapubic incisions and trocar insertion lateral to the midline should be made either medial to the obliterated umbilical ligament or lateral to the round ligament. When introducing the lower lateral trocar, it is important not to damage the femoral vessels running at the level of the inguinal ligament. Insertion of trocars along the midline of the abdomen is generally safe for the vessels of the anterior abdominal wall, since the midline is an avascular zone.
A panoramic examination of the abdominal organs begins with the patient in a horizontal position, which allows one to get a general idea of their condition and confirm the presence of fluid (blood, pus, serous effusion), fibrin, adhesions, and dissemination of a malignant tumor. Sometimes already at this stage it is possible to establish a preliminary diagnosis and determine further treatment tactics. A targeted examination allows you to clarify the diagnosis and perform a biopsy. For a targeted examination of a particular organ, by controlling the operating table, create a Trendelenburg, Fowler position, on the right or left side. In some cases, it is necessary to use an additional 5-mm trocar and an instrument (clamp, dissector) to lift or retract tissue, aspirate fluid, and take material for biopsy. A biopsy of the ovary, affected area of the peritoneum or other pathological formations is performed using biopsy forceps or scissors. The bleeding area is coagulated with bi- or monopolar forceps.
Inspection of the abdominal cavity is carried out clockwise, starting from the right upper quadrant of the abdomen. For ease of inspection, the abdominal cavity is conventionally divided into 6 sectors.
Sector 1 – right upper quadrant of the abdomen: the right lobe of the liver, the right half of the diaphragm, the gallbladder, the duodenum, part of the greater omentum, and intestinal loops located in this area. On the left, this area is limited by the falciform and round ligaments of the liver.
Sector 2 – left upper quadrant of the abdomen: left lobe of the liver, anterior wall of the stomach, left half of the diaphragm, part of the greater omentum and intestines, spleen.
Sector 3 – peritoneum of the left half of the abdomen.
Sector 4 – the small pelvis and the organs located in it (in the Trendelinburg position).
Sector 5 - peritoneum of the right half of the abdomen.
Sector 6 – small and large intestine, greater omentum, cecum, vermiform appendix.
It is rational, in our opinion, to initially examine the organs located in the projection of the umbilical region, where the Veress needle and the main trocar were “blindly” inserted.
In laparoscopy, there are so-called blind spots: the insertion site of the laparoscope, the posterior wall of the abdominal cavity, and some organs located meso- and retroperitoneally.
After completing the examination, further treatment tactics are chosen: completion of the procedure, biopsy or drainage, laparoscopic surgery or transition to laparotomy.
Indications for implementation
Indications for laparoscopy are:
- diagnostic examination of the pelvic organs;
- uterine fibroids;
- genital endometriosis;
- idiopathic infertility;
- chronic pelvic pain;
- ovarian pathologies (cysts, space-occupying formations, sclerocystosis);
- pathologies of the fallopian tubes (obstruction, hydrosalpinx, sactosalpinx, tubal pregnancy, etc.), as well as tubal ligation for the purpose of sterilization;
- pelvic organ prolapse;
- isthmic-cervical insufficiency;
- adhesive disease of the pelvis.

Contraindications
Absolute contraindications include:
- cancer of the ovary or fallopian tube;
- chronic diseases of the cardiovascular or respiratory systems in the stage of decompensation, as well as acute renal and liver failure;
- bleeding disorders that cannot be corrected;
- obesity degrees III and IV;
- any violations that prevent the patient from being in the so-called Trendelburg position during the operation, in which the pelvis is elevated in relation to the head (sliding hernia of the diaphragm, cerebral vascular pathologies);
- hemorrhagic shock.
In addition, there are relative contraindications, which include severe adhesions in the pelvis, acute infectious diseases and some other disorders.
Possible complications after laparoscopy in gynecology
Immediately after laparoscopy of the ovaries or fallopian tubes, women may complain of aching sensations in the neck, abdomen, and shoulders. This is due to the fact that during the operation gas is injected into the abdominal cavity. Such sensations can be eliminated with the help of simple exercises. The risk of complications after laparoscopy is much lower than after abdominal surgery, since it is a minimally invasive method. As a result, there is less tissue injury and there are no postoperative scars. However, it must be borne in mind that performing laparoscopy requires great skill from the surgeon. Although laparoscopy is performed in many clinics in Moscow, it is recommended to go only to medical centers specializing in the treatment of infertility. This will help avoid potential complications associated with insufficient qualifications of the doctor (damage to blood vessels and internal organs, infection, tissue burns). In particular, all operating gynecologists at Nova Clinic have many years of successful experience in performing such operations. Complications after laparoscopy can also develop due to the fact that the patient does not follow the doctor’s instructions. Therefore, strictly follow the doctor's recommendations and observe restrictions related to physical activity, diet and intimate relationships for a certain time.
Laparoscopy for endometriosis
Laparoscopy allows you to identify foci of endometriosis at a very early stage and remove them in a timely manner. Surgical treatment of endometriosis is aimed at excision of endometriotic foci and infiltrates, and only in the initial forms of development is it possible to use laser vaporization, electrocoagulation and others.
To confirm the diagnosis of external genital endometriosis, it is necessary to obtain pathological tissue, which can only be done through surgery.
Features of the recovery period

Elements of accelerated rehabilitation have been introduced into the work of the gynecological oncology department of UKB 4. One of the aspects of “fact track” surgery is the early activation of the patient, which in such an operation is carried out 5-6 hours after completion of the operation. The patient is allowed to sit down, stand up (the first time under the supervision of medical personnel) and walk if she feels well.
In order to reduce the intensity and relieve pain, intramuscular injections of non-steroidal anti-inflammatory drugs are used, which also contribute to accelerated rehabilitation. Since laparoscopic operations, in comparison with surgical interventions performed by transection, are accompanied by less severe pain, in most cases, the use of narcotic analgesics is not required.
These measures can reduce the risk of postoperative thromboembolic and inflammatory complications, as well as the risk of adhesions.
In addition, all patients are prescribed elastic compression (wearing compression stockings or elastic bandages) to prevent thrombosis of the veins of the lower extremities. Depending on the degree of risk of thromboembolic complications in the postoperative period, low molecular weight heparins or antiplatelet agents may be prescribed, which reduce blood clotting.
As part of rehabilitation therapy, antibacterial drugs are used, as well as agents that normalize intestinal motility and eliminate nausea (if it occurs).
An important point is to follow the correct diet: on the day of the operation, you are not allowed to eat (you can drink still water); for the next 2-3 days, a gentle diet is prescribed until intestinal function is restored.
The following products are not allowed during this period:
- -raw vegetables and fruits;
- -sweets;
- -bakery products;
- -juices, sweet drinks, coffee, carbonated drinks;
- -sweet sour milk products.
If surgical treatment is not associated with an ectopic pregnancy and is not accompanied by intervention on the ovaries (for example, removal of a cyst), menstruation occurs on time (according to the calendar).
However, 1-2 days after chromosalpingoscopy there may be a slight discharge associated with the release of the contrast agent.
The patient spends several days in the hospital (4-6 days), after which she is discharged home (if there are no complications).
It is recommended to limit strenuous physical activity for 21 days after laparoscopy. The duration of sexual rest is determined by the attending physician and depends on the type and extent of the surgical intervention.
In addition, sitz baths, steam baths, saunas, swimming pools, and swimming in the sea are not recommended for about 2 weeks, but the period may vary depending on the extent of the operation and the healing of the sutures.
Sutures are removed 5-7 days after laparoscopy (the day of surgery is not taken into account in the calculation). After this, you can shower completely, including soaking post-operative scars.
At first, the scars are pink in color, then gradually fade and become almost invisible.
Compliance with all doctor’s instructions during the recovery period after laparoscopy helps reduce the likelihood of complications and successful rehabilitation.