Indications for the procedure
The examination of the larynx is carried out as prescribed by the ENT specialist. The main indication for its implementation is unusual sensations or discomfort in the throat:
- hoarseness or lack of voice;
- pain when swallowing;
- feeling of a foreign object;
- pain symptoms of unknown etiology;
- the appearance of a cough with blood inclusions.
The procedure is mandatory for patients diagnosed with:
- laryngitis;
- obstruction of the respiratory tract;
- dysphonia;
- vocal cord paresis.
There are also contraindications
. The procedure is not performed on patients diagnosed with epilepsy, heart disease, or inflammatory processes in the larynx or nasal cavity.
Causes
Diseases of the throat and larynx can have various causes. The most common of them:
- viral infection caused by adeno-, rhino-, enterovirus, pathogens of influenza, mumps, parotitis, Epstein-Barr and Coxsackie virus;
- a bacterial infection caused by streptococci, diphtheria pathogens, staphylococci, less commonly gonococci, chlamydia and other microorganisms;
- the effect of toxic or irritating substances - cigarette smoke, exhaust gases, chemical products, soot;
- allergic reaction, cough, sinusitis, gastroesophageal reflux;
- trauma or foreign body penetration, as well as excessive vocal strain.
Treatment of diseases of the throat and larynx should be entrusted to a specialist - an ENT doctor. Correct determination of the cause of the disease is one of the main conditions for recovery.
Procedure for throat endoscopy
No special training is required. You should not drink or eat food for four hours before the endoscopy. This will help minimize gagging. If the patient uses removable dentures, they must be removed.
Before starting the manipulations, find out what endoscopy of the larynx is, how the procedure will be carried out and how long it can last. The doctor is obliged to tell the patient about what will happen to him.
The patient is then placed on his back. The mucous surface of the larynx is anesthetized. The endoscope tip is disinfected. An anesthetic gel is also applied to it. The doctor inserts an endoscope into the larynx. The resulting image is transmitted to the screen in enlarged form. The specialist carefully examines the anatomical structure of the larynx. Section by section, he carefully examines the mucous membranes.
During the examination, the doctor may take an analysis of the affected tissues for cytological examination. If necessary, simple surgical operations can be performed.
Diagnostics
To diagnose diseases of the throat and larynx, doctors use the following instrumental diagnostic methods:
- pharyngoscopy, which includes examination of all parts of the pharynx using a nasopharyngeal or laryngeal mirror, as well as a special device - an epipharyngoscope;
- laryngoscopy – examination of the larynx using mirrors;
- microlaryngoscopy - direct examination of the walls of the larynx using a microscope;
- fiberoscopy - examination of the larynx using a fiber optic apparatus; During the procedure, you can remove a small foreign body or take a biopsy;
- radiography and computed tomography, including contrast, useful for identifying stenoses, malformations, tumors;
- Magnetic resonance imaging is a safe study, especially informative for soft tissue pathologies, including tumors.
Laryngoscope: types, features, rules of use
A laryngoscope is a medical device, a type of endoscope. With its help, you can quickly, easily and fully examine the larynx and carry out some operational actions. This device is safe for patients and eliminates any risk of injury during the examination.
There are two main types of laryngoscopes:
- Flexible. It is a tube to which replaceable blades are attached. These blades include a light located on the laryngoscope. The device is inserted through the patient's nose.
- Rigid. This is a rigid handle that also has blades and a lamp. The device is inserted through the mouth under general anesthesia.
There are also reusable and disposable laryngoscopes. The latter are usually used in ambulances, where there is not enough time and suitable conditions for processing a reusable laryngoscope. An otolaryngologist's office usually uses a reusable device, which must be disinfected in a special solution after each use. Before processing the device, you must read the instructions for it.
Laryngoscopy (especially direct) is a very informative and high-quality way to examine the larynx. However, its quality largely depends on the device used. The Rumex Group company offers to purchase excellent laryngoscopes for conducting examinations at the appropriate level. We guarantee a large selection and excellent quality.
Treatment of metastases in the lymph nodes of the neck
Regional metastases in laryngeal cancer do not interfere with conservative therapy, because neoplasms of this localization (N1-N2) are often amenable to chemotherapy and radiation. Therefore, the lymph nodes on both sides must be included in the irradiation zone of the larynx. If it is necessary to irradiate the lymph nodes of the lower parts of the neck, the use of a direct field with a block is indicated. The lower edge of this field extends 1 cm below the lower border of the clavicle. In case of damage to the supraclavicular lymph nodes, it is necessary to irradiate the lymph nodes of the upper mediastinum.
When non-displaceable or limited displacement metastases are present, it is advisable to begin treatment with neoadjuvant polychemotherapy followed by 40 Gy of radiation. Further, the tactics are determined by the effectiveness of the treatment. If significant or complete regression of metastases is observed, as well as their inoperability after a dose of 40 Gy, then irradiation is adjusted to 60-70 Gy.
It is worth especially noting that today, when the indicator of quality of life is as important as the reliability of oncological treatment, specialists are directing their efforts to the development and improvement of conservative therapy, including various types of chemotherapy and radiation, as well as to performing organ-saving operations that allow preserving or restoring the main functions of the larynx.
Special instructions for treatment
According to research, if the supraglottic region is affected and the process extends to stage T1N0M0, it is better to give preference to irradiation (the cure rate reaches 95%, the function of the larynx is preserved). For T2N0M0 and similar localizations, organ-sparing surgery is indicated, because up to 80% of relapses after irradiation are associated with damage to these particular laryngeal structures.
If the folded area is affected and stage T1N0M0 is recorded, therapy begins with irradiation. With this method, the cure rate is 75-78%, taking into account which it is necessary to carry out an initial assessment of the effectiveness of therapy at a dose of 40 Gy. If regression of the tumor is less than 70%, then surgical intervention – chordectomy – is possible. When the tumor has spread to the anterior commissure and second vocal fold, laryngeal resection is performed, because in this case the long-term results are better than with radiation.
Chemotherapy does not improve treatment outcomes for stage T1-2N0M0.
When treating locally advanced pathology at stage T3N0M0-T4N0M0, the greatest effectiveness was shown by the use of a combined technique with different sequences of irradiation and surgery, because in this case, 70-73% of patients achieve five-year survival. However, this involves performing a laryngectomy, which disables the patient.
If the patient has contraindications to surgery, therapy begins with radiation. If the cancer is advanced T3-T4, then the options for radiation therapy are limited. Moreover, even if operations are possible, they are crippling in nature. An option for organ-preserving treatment of locally advanced pathology or the hypopharynx may be a combination of induction chemotherapy according to the PF regimen (Cisplatin and 5-fluorouracil) with further irradiation if there is a response to therapy. If it is not observed, a laryngectomy is performed.
Features of the development of metastases, depending on the location of the oncology
Supraglottic section
There is a well-developed lymphatic network here, which helps the tumor quickly spread throughout the local and regional localization. Metastases mainly affect the upper and middle group of lymph nodes located in the deep jugular chain - 50-60% of cases. Metastases are localized:
- in 57% of cases on the side of the tumor;
- in 9% - on both sides of the larynx;
- in 6.3% - contralaterally, that is, on the side opposite to the tumor.
Vocal folds
Due to the low lymph circulation, metastases are rarely observed here. In 5-12% of cases they are found in the middle deep jugular lymph nodes.
Subglottic department
Regional metastases occur in 5-12% of cases. Moreover, in 20% of cases they develop in the pretracheal and prelaryngeal lymph nodes. Lymph moves towards the lower deep jugular lymph nodes, where metastasis is also diagnosed.
Distant metastases are most often diagnosed in the ribs, lungs, and mediastinum.
How to sign up for an ultrasound scan at the medical center in Tushino?
In the multidisciplinary medical center, which is located at the Skhodnenskaya metro station, anyone can have an ultrasound of the throat for preventive and diagnostic purposes.
Timely ultrasound examination makes it possible to detect the disease in the early stages and begin therapy.
You can make an appointment with a doctor by calling the numbers listed on the website or in person at the clinic. The administrator of the medical center will answer all questions and familiarize you with the price list. The medical center in Tushino operates around the clock, so you can visit specialists at any convenient time.
Rehabilitation
Speech therapy rehabilitation methods are widely used, aimed at restoring vocal function and achieving good voice quality. It is possible to achieve the set goals in 45-60% of cases.
After laryngectomy:
The voice is a socially important function that does not need proof, so it is quite reasonable for patients to strive to preserve or restore it. For those who have had a laryngectomy, vocal rehabilitation is carried out through training in the so-called esophageal voice, the use of voice devices, or the installation of a tracheoesophageal shunt of the Bloom-Singer type.
One of the methods for voice rehabilitation in patients who have undergone complete resection of the larynx is the use of voice-forming devices of various designs. These can be electric larynxes, sound generators.
According to many authors, the method of teaching esophageal speech is the most physiological and minimally invasive. In 62-91% of cases it is possible to form a pseudo-voice, which will be sufficient for communication.
Disadvantages of the method:
- patients find it difficult to master the method of swallowing air masses into the esophagus and pushing it out during phonation;
- the esophagus as a reservoir for air has a small volume - 180-200 ml;
- spasm and hypertonicity of the compressive elements of the pharynx.
Surgical technique for voice restoration after laryngectomy
The method is based on the formation of a shunt between the esophagus and trachea. Through it, air from the lungs enters the pharynx and esophagus, provoking vibration of the pharyngoesophageal element, which is the voice generator.
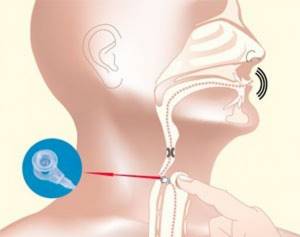
A voice prosthesis placed in the lumen of the shunt allows air from the lungs into the esophagus and prevents food and liquid from entering in the opposite direction.
Good voice quality, thanks to this technique, was achieved in 93.3% of patients. However, the authors of the method indicate that in 7-30% of cases complications are possible: fungal infection of the prosthesis, excessive growth of granulations, displacement of the prosthesis, leakage of the prosthesis, which can lead to aspiration pneumonia in patients.
Studies show that all patients after organ-preserving operations experience impaired swallowing function, because the entire mechanism is rebuilt in accordance with the type of intervention. Violations of the protective function are more significant after horizontal and sagittal resection of the larynx. To prevent aspiration of food and saliva in the postoperative period, various methods of obturation (blockage) of the larynx are used: starting with Mikulicz tamponade (indicated during sagittal surgery) and ending with the use of obturators and T-shaped silicone tubes with a closed upper end, inserted into the formed respiratory anastomosis . These measures are aimed at preventing food from entering the respiratory tract.
Chronic aspiration of saliva often leads to pneumonia, so corrective surgery is indicated in some cases. Solving this problem affects the patient's future life, because constant aspiration may cause the need for laryngectomy.
One of the most difficult tasks when performing organ-saving operations is restoring respiratory function, because all types of resection, with the exception of extirpation of the epiglottis, deform the larynx and reduce its size. V. O. Olshansky gives a relatively higher figure - he is able to decannulate 73.4% of patients. The author used a tube-shaped endoprosthesis consisting of biologically compatible polymer materials impregnated with an antiseptic composition to restore the lumen of the larynx.
Contraindications to direct laryngoscopy
Despite all its informative content, this procedure may not be applied to every patient. There are a number of contraindications to direct laryngoscopy:
- Changes in the cardiovascular system (heart defects, severe hypertension, etc.)
- Epilepsy with frequent seizures
- Sharp stenotic breathing
- Damage to the cervical vertebrae
- Aortic aneurysm
- Acute inflammatory diseases of the oral mucosa/larynx/pharynx
- Bleeding of the pharynx/larynx
- Allergy to certain drugs
- Pregnancy
Some of the listed contraindications are relative - if you have these diseases, it is recommended to consult your doctor about the possibility of direct laryngoscopy. Individual contraindications are also possible: if there is an intolerance to some components, an increased sensitivity threshold, etc. Therefore, before conducting the examination, consultation with a specialist is required , to whom you need to report this data.
Method of performing ultrasound of the throat
Ultrasound of the throat does not require special preliminary preparation of the patient. A special gel is applied to the examined area of the anterior wall of the submandibular cervical spine, which ensures better conductivity of the convex sensor signal. Next, under the influence of ultrasound, information about the condition of the tissues begins to be read and indicators are displayed on the monitor, after which the doctor deciphers the overall picture.
The examination is performed with the patient lying on his side. The entire procedure takes about 20–30 minutes.
Types of laryngoscopy
Depending on the method of implementation it may be:
- straight;
- indirect;
- retrograde;
- or microlaryngoscopy is performed.
Indirect laryngoscopy
Indirect laryngoscopy is a continuation of external examination and palpation of the neck. The doctor acts in the following sequence:
- The laryngeal mirror, preheated in hot water or over an alcohol lamp and wiped with a napkin, is fixed on the handle.
- The patient then opens his mouth and sticks out his tongue. Mouth breathing.
- The tip of the tongue is wrapped in a gauze napkin and slightly pulled down and towards itself. With the index finger of the hand, the doctor lifts the upper lip of the subject.
- The introduction of a mirror into the oral cavity follows the same principle as during posterior rhinoscopy. The tongue is then raised to allow visualization of the pharynx. If necessary, the soft palate is also raised.
- The light beam from the head reflector is directed strictly at the mirror.
- To displace the epiglottis and gain access to the larynx, the patient is asked to pronounce the sounds “e” or “i” and inhale air. Thanks to this, the doctor can assess the condition of the organ in the phases of phonation and inspiration. The vocal folds normally have a pearly white tint and are symmetrical.
After inspection, the mirror is removed from the larynx, separated from the handle and lowered into the disinfection solution.
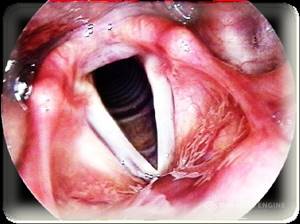
| a — position of the laryngeal mirror (front) b — position of the laryngeal mirror (side) c — indirect laryngoscopy: 1. epiglottis; 2. false vocal folds; 3. true vocal folds; 4 - arytenoid cartilage |
Direct laryngoscopy
Direct laryngoscopy is based on the use of laryngoscopes, which also allow the removal of foreign bodies and surgical interventions. There are laryngoscopy sets that include fiber optic guides, interchangeable spatulas, etc. They are suitable for examining the larynx in both adults and children. The advantage of the direct method, compared to the indirect one, is the possibility of a more detailed assessment of the condition of the organ being studied.
Local anesthesia is provided by lubricating the laryngeal mucosa with a weak solution of dicaine. The introduction of the spatula takes place in several stages:
- bringing first to the epiglottis, and then going around it and entering the larynx;
- pressing the root of the tongue and moving the instrument to a vertical position.
Thus, the arytenoid cartilages, the posterior wall of the trachea, the vocal cords, etc. can be examined.
Retrograde laryngoscopy
This technique is used after tracheostomy. As part of the examination, the upper part of the trachea, subglottic cavity and other parts are visualized. To do this, the doctor inserts a nasopharyngeal speculum through the tracheostomy. As with any other laryngoscopy, in this case it is preheated and wiped with a napkin. A beam of light from the frontal reflector is directed onto a mirror surface.
Epidemiology
- In terms of prevalence in the world, malignant neoplasms of the neck and head occupy 6th place.
- The main localizations of the organs of the neck and head are the larynx and hypopharynx.
- In Russia, laryngeal cancer ranks 5th in terms of incidence.
- The highest incidence is in Thailand, Poland, Ohio (USA), Italy, France, and Spain.
- Men are more susceptible to the disease – 1 in 10.
- Most often - in 95% of cases - among malignant lesions of the larynx, squamous cell carcinoma is diagnosed.
- Among all malignant neoplasms of the neck and head, this disease is in 1st place.
- In the general structure of cancer pathologies – 2.6%.
- The incidence rate per 100,000 people is 4-6.
- Low incidence (that is, less than 2 per 100,000 people) is observed in Japan, Norway, and Sweden.
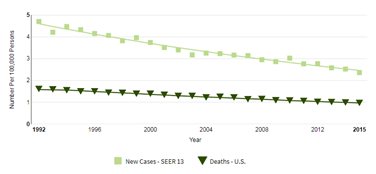
We invite you to familiarize yourself with visualized statistics for the United States for 1992-2015. The graph shows deaths and the number of newly diagnosed cases.
Definition
The larynx is the area of the throat that is located between the trachea and the root of the tongue. Its structure contains vocal cords, the vibration of which produces the human voice.
To determine the prevalence of the process, it is necessary to take into account the anatomy of the larynx. It is divided into 3 sections according to a number of features: differences between the mucous and submucosal layers, lymph and blood circulation, etc. Let's consider the main sections of the organ:
- Upper, or vestibular. It includes the following structures: aryepiglottic ligaments on the laryngeal side, Morganian ventricles, false vocal cords, epiglottis.
- Average. This is the area where the true vocal cords are located.
- Lower, or subglottic.

This gradation largely determines the differences in the course of the disease. Most often, the fold and supraglottic sections are affected (50-70%), while the incidence in the fold section is 30-40% of cases, and in the subglottic section – 3-5%. The most malignant course is if the tumor affects the vestibular region. In this case, metastases develop with a frequency of 40-60%. The most favorable prognosis is if the fold section is affected. Metastases are diagnosed in 5-12% of cases. If the subglottic region is affected by a neoplasm, the indicators are approximately the same.
Precancerous diseases
Let's consider the pathologies that precede laryngeal cancer:
- laryngitis, which a person suffers from in a chronic form for many years;
- a special role in the appearance of this pathology is played by: most often - papilloma, which has existed for a long time, and leukoplakia of the mucous membrane lining the larynx;
- pachydermia;
- dyskeratoses;
- cystic formations on the laryngeal ventricles;
- broad-based fibroma;
- chronic inflammation that cannot be treated and is caused by smoking, alcoholism, and syphilis.

Laryngitis
Laryngitis

Papilloma

Papilloma

Leukoplakia

Leukoplakia