The intestine consists of two sections: thin (with a diameter of 4 to 6 cm at the beginning and from 2.5 to 3 cm at the end) and thick (with a diameter of 4 to 10 cm). The total length of the intestine reaches 7-8 meters. Oncological diseases can develop in any of these departments. Depending on the location of the tumor, symptoms, treatment and diagnosis of colon cancer may differ. With timely detection and treatment, this disease has a favorable prognosis.
Early diagnosis of intestinal cancer is carried out at the Yusupov Hospital in Moscow. Thanks to modern diagnostic equipment and the vast experience of our specialists, maximum accuracy of research results is achieved.
Kinds
Based on histological characteristics, intestinal cancer is divided into:
- adenocarcinoma - a formation of malignantly changed glandular cells and occurs in 95% of all cases of the disease;
- lymphoma - a tumor formed from fibrous tissue of the intestinal wall;
- carcinoma - a formation consisting of epithelial cells;
- sarcoma is a malignant tumor that forms mainly on the outer wall of the intestine from connective tissue cells;
- melanoma - the basis are skin cells called melanocytes.
Tumors are classified according to the type of growth:
- exophytic - growing on the inner wall in the intestinal lumen, as a result of which obstruction of the organ gradually develops;
- endophytic – growing into the intestinal wall with subsequent formation of ulcers and a high risk of metastases upon contact with healthy tissues;
- diffuse – tumors growing to the sides from the focus without narrowing the intestinal lumen;
- mixed - having characteristics of two or three of the listed types.
Blood chemistry
The method identifies abnormalities that may be a sign of cancer. It should be taken into account that the same changes are characteristic of many non-oncological diseases, so the results cannot be interpreted unambiguously.
The doctor analyzes the following indicators:
- Total protein. Cancer cells feed on protein, and if the patient has no appetite, then its volume is significantly reduced. In some cancers, the volume of protein, on the contrary, increases.
- Urea, creatinine. Their increase is a sign of poor kidney function or intoxication, in which protein in the body is actively breaking down.
- Sugar. Many malignant tumors (sarcoma, cancer of the lung, liver, uterus, breast) are accompanied by signs of diabetes mellitus with changes in blood sugar levels, since the body does not produce insulin well.
- Bilirubin. An increase in its volume may be a symptom of malignant liver damage.
- Enzymes ALT, AST. Increased volume is evidence of a possible liver tumor.
- Alkaline phosphatase. Another enzyme, an increase in which may be a sign of malignant changes in bones and bone tissue, gall bladder, liver, ovaries, and uterus.
- Cholesterol. With a significant decrease in volume, liver cancer or metastases to this organ may be suspected.
Blood is drawn from a vein. It must be taken on an empty stomach.
Symptoms
In case of intestinal cancer, the first symptoms are manifestations of general intoxication, developing due to the growth of a malignant neoplasm and the immune response, as well as due to impaired digestive function. Among them:
- fatigue, general weakness;
- joint pain as a result of an autoimmune reaction;
- a steady increase in temperature to a little over 37 degrees;
- unexplained weight loss;
- aversion to the smell of meat or some other products;
- nausea;
- pale skin;
- flatulence, bloating, colic;
- dark stool with lots of mucus.
Subsequently, as the intestinal tumor grows, the symptoms increase and new signs appear;
- cramping abdominal pain with a frequency of 15-20 minutes;
- asymmetrical increase in abdominal volume;
- frequent vomiting due to general intoxication;
- alternating diarrhea and stool retention;
- traces of blood in the stool.
When intestinal obstruction occurs due to the tumor blocking the intestinal lumen, the intestinal wall stretches excessively, blood circulation in it is disrupted, resulting in necrosis of the deformed tissue and peritonitis.
Forms of bowel cancer
A disease such as intestinal cancer involves damage to various parts of the intestine, from the duodenum to the rectum. However, lesions of the small intestine or duodenal cancer are extremely rare, the stages of the process and symptoms are similar, and digestive disorders predominate. When doctors usually talk about intestinal cancer, they mean the colorectal form of the tumor.
When bowel cancer is diagnosed, additional tests are performed to determine the extent of the disease. The stages of colorectal cancer are as follows:
- Stage I (least common cancer): A tumor that affects only the innermost layers of the colon or rectum. The cure rate for stage I cancer is more than 90%, which emphasizes the importance of early detection of pathology.
- Stage II: cancer demonstrating active growth and spread of the tumor through the wall of the colon or rectum to adjacent structures.
- Stage III: cancer associated with the spread of the process to local lymph nodes (metastases).
- Stage IV (the most common cancer): The tumor cells have spread to distant organs, usually the liver and lungs or lymph nodes far from the original tumor.
Causes and risk factors
At the moment, there is no reliably established list of causes of intestinal cancer, but experts know factors that increase the risk of developing a malignant tumor.
- Benign neoplasms. This includes adenomas and polyps that form in the intestines, but there is no exact data on what exactly triggers the process of malignant degeneration of cells.
- Chronic inflammation. These are nonspecific ulcerative colitis, Crohn's disease, dysbiosis of various types, colon diverticulosis (formation of peculiar pockets in the intestinal wall).
- Unbalanced diet. A lack of plant fiber in combination with a large amount of highly processed meat products causes impaired peristalsis and irritation of the intestinal wall.
- Impact of external factors. Aniline dyes, carcinogenic compounds, and radioactive radiation can serve as a trigger for the malignant degeneration of cells.
Am I at risk?
Your risk of colon cancer may be higher than average if:
- you or your close relatives have had polyps or colon or rectal cancer;
- you have inflammatory bowel disease;
- you have a family history, such as familial adenomatous polyposis (FAP) or hereditary nonpolyposis colon cancer.
If you think your risk of developing colon cancer is significantly higher than the population average, talk to your oncologist about it. He or she may suggest that you get screened more often or enroll in screening programs at a younger age, rather than waiting until age 50.
Stages
Clinical symptoms of intestinal cancer directly depend on the stage of the disease.
- The tumor develops within the epithelium and does not penetrate other tissues; there are no metastases. Clinical manifestations are absent or so insignificant that they do not attract the patient’s attention. Diseases are discovered accidentally during histological examination of removed polyps.
- A malignant neoplasm grows into the submucosal or muscular layer without affecting adjacent lymph nodes. The disease may manifest itself in the form of initial general symptoms.
- The tumor grows through the entire intestinal wall and can affect neighboring organs. Metastases are present in regional lymph nodes. Severe symptoms include general malaise and intestinal dysfunction.
- The malignant node gives multiple metastases to distant organs. The patient experiences constant abdominal pain, intestinal bleeding, and severe intoxication with tissue breakdown products.
Analysis of urine
Cancer of the urinary system manifests itself as blood in the urine.
Urine may also contain ketone bodies, which indicate tissue breakdown. However, these symptoms also accompany diseases not related to oncology, for example, they indicate the presence of stones in the bladder or kidneys, or diabetes mellitus. For diagnosing other types of cancer, urine analysis is not informative. It cannot be used to judge the presence of cancer, but deviations from the norm indicate health problems. If the deviations are serious and confirmed by the results of other basic tests, then this is a reason to conduct special tests to determine cancer.
The exception is multiple myeloma, in which specific Bence Jones protein is determined in the urine.
For the study, morning urine is collected in a sterile container, which can be purchased at a pharmacy. You need to take a shower first.

Diagnostics
The main difficulty in diagnosing intestinal cancer is the patient’s failure to see a doctor in a timely manner.
In the early stages, clinical manifestations are mild, which makes it difficult to make a primary diagnosis.
To identify a tumor, a number of tests are prescribed.
- General and biochemical blood tests. The level of hemoglobin, the number of red and white blood cells, the level of bilirubin, the presence of tumor markers, etc. are examined.
- Colonoscopy. Using a special probe inserted into the anus, an oncologist or gastroenterologist examines the large intestine for the presence of tumors and ulcerative defects. If suspicious areas are detected, a biopsy is performed followed by histological examination of the tissue.
- Irrigoscopy. X-ray contrast examination of the large intestine reveals deformed areas, tumors, compactions and other structural abnormalities.
- Ultrasound of the abdominal cavity. The study makes it possible to clarify the size of the tumor, detect germination into other organs and metastases in the lymph nodes, liver, mesentery, and other organs.
- CT scan of the abdomen. The most accurate and informative study allows you to estimate the size of the tumor, determine the stage of cancer, germination into organs, and the presence of metastases.
Laboratory markers of colon cancer
A study of the concentration of the main markers of colon cancer, which is used for diagnosis, assessment of prognosis and monitoring of treatment of this disease.
Synonyms Russian
Blood tests for colon cancer, tumor markers for colon cancer
English synonyms
CA 19-9, CA 242, Gastrointestinal Cancer Antigen, GICA, Carcinoembryonic antigen, CEA, CD66e, CEACAM5.
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- Do not eat for 8 hours before the test; you can drink clean still water.
- Avoid physical and emotional stress for 30 minutes before the test.
- Do not smoke for 24 hours before the test.
General information about the study
Colon cancer (CC) is the most common malignant disease of the gastrointestinal tract. Diagnosis of cancer is complex, with laboratory research methods playing a central role. The study of tumor markers provides valuable diagnostic and prognostic information. The most well studied tumor markers are CA 19-9 and cancer embryonic antigen.
Carcinoembryonic antigen (CEA) is a large glycoprotein that is structurally similar to immunoglobulins. It is synthesized by cells of the colon and probably mediates cell-to-cell interactions. CEA has been shown to play a role in stimulating tumor growth, invasion and metastasis.
An increase in the level of CEA is characteristic of RTC. At the same time, high levels of CEA are more often observed in late stages of the disease and/or in the presence of a large tumor. In the early stages of the disease, CEA levels are usually normal. It should also be noted that in approximately 15% of cases of large RTC, the CEA level also remains normal. There is no relationship between the level of CEA and the histological type of the tumor. An increase in CEA can also be observed in some non-oncological diseases of the gastrointestinal tract (hepatitis, ulcerative colitis and Crohn's disease, pancreatitis), oncological diseases of other organs (breast, ovarian, kidney cancer) and non-oncological diseases of other organs (chronic obstructive pulmonary disease, endometriosis).
The CEA level is also used to assess the prognosis of the disease. It has been shown that a high level of CEA in the preoperative period is an unfavorable prognostic sign. An increase in CEA levels in the postoperative period may indicate a relapse of the disease.
Tumor marker CA 19-9 (carbohydrate antigen) also belongs to glycoproteins in structure. Like CEA, CA 19-9 is found in elevated concentrations in the blood of patients with RTC and some other diseases (pancreatitis, liver disease). As with CEA, the CA 19-9 level does not reflect the histological type of tumor. The sensitivity of CA 19-9 for RTK is lower than the sensitivity of CEA. A joint study of tumor markers CA 19-9 and CEA makes it possible to achieve higher sensitivity. Some authors suggest using the CA 19-9 tumor marker in combination with CEA to assess the prognosis of cancer.
Cancer antigen CA 242 is a high molecular weight glycoprotein, which, like the tumor marker CA 19-9, is produced by epithelial cells of the gastrointestinal tract, but has more pronounced sensitivity and specificity to malignant tumors. CA-242 levels are elevated in almost all patients with gastrointestinal tumors, especially in pancreatic, colon, and rectal cancer. CA-242 is produced by tumor cells and enters the bloodstream, making it an effective tumor marker that allows diagnosing the disease at an early stage and monitoring its progress.
The main feature of the CA 242 tumor marker is its low expression in benign diseases of the gastrointestinal tract, which makes it possible to use it for the differential diagnosis of benign and malignant tumors.
Currently, the study of the concentration of these tumor markers is not used as an independent test for the diagnosis of cancer, but is complemented by other tests (for example, a fecal occult blood test) and instrumental studies (for example, colonoscopy). The result of the tumor marker study is assessed taking into account all relevant information about the patient.
What is the research used for?
- For the diagnosis of colon cancer (CC);
- to assess the RTC forecast;
- for early detection of RTC recurrence.
When is the study scheduled?
- If colon cancer is suspected in the presence of unmotivated weakness, weight loss, decreased appetite, nausea, stool abnormalities, blood in the stool, abdominal pain;
- periodically when monitoring the patient in the postoperative period.
What do the results mean?
Reference values
For each indicator included in the complex:
- [08-006] CA 19-9
- [08-042] Carcinoembryonic antigen (CEA)
- [08-105] CA 242
| Reasons for the increase | Reasons for the downgrade: | |
| REA |
|
|
| SA 19-9 |
|
|
| CA 242 |
|
|
What can influence the result?
- Presence of concomitant diseases;
- relapse of the disease and the appearance of metastases;
- start of chemotherapy.
Important Notes
- The test is not intended to screen for colon cancer;
- normal values of tumor markers do not completely exclude colon cancer;
- the results of the study are assessed taking into account additional anamnestic, instrumental and laboratory data.
Also recommended
[08-090] Tumor Marker 2 (TM 2) - pyruvate kinase
[42-019] Predisposition to colorectal cancer
[12-015] Histological examination of biopsy samples of organs and tissues (except for the liver, kidneys, prostate gland, lymph nodes)
[12-027]Immunohistochemical study of clinical material (using 1 antibody)
Who orders the study?
Oncologist, general practitioner, therapist.
Literature
- Swiderska M, Choromańska B, Dąbrowska E, Konarzewska-Duchnowska E, Choromańska K, Szczurko G, Myśliwiec P, Dadan J, Ladny JR, Zwierz K. The diagnostics of colorectal cancer. Contemp Oncol (Pozn). 2014;18(1):1-6. Review.
- Chernecky CC Laboratory Tests and Diagnostic Procedures / S.S. Chernecky, V.J. Berger; 5th ed. — Saunder Elsevier, 2008.
Treatment
The choice of treatment for bowel cancer depends on the stage of the disease.
- At the zero stage, i.e. If polyps are detected, they are removed using colonoscopy, without opening the abdominal cavity
- At the first stage, the segment of intestine with the tumor and part of the mesentery are surgically removed.
- In the second stage, chemotherapy is given before surgery to shrink the tumor. After surgery, the remaining cells are destroyed using chemotherapy or radiation therapy.
- For stage three colon cancer, surgical treatment is performed in combination with chemotherapy or radiation therapy. Areas affected by cancer and regional lymph nodes are removed.
- At the fourth stage, the nature of the operation depends on the degree of spread of malignant tumors. If it is impossible to remove the tumor, palliative treatment is performed to exclude intestinal obstruction.
Questions and answers
How to recognize bowel cancer?
The initial symptoms of bowel cancer are similar to a number of other, less dangerous diseases, so patients often do not pay attention to them. If for no apparent reason:
- loss of appetite, aversion to meat dishes;
- stomach ache periodically;
- there is constant discomfort in the abdomen, gas formation has increased;
- prolonged constipation began, alternating with bouts of diarrhea;
this means that you should contact a gastroenterologist or proctologist for examination as soon as possible.
Is there a cure for bowel cancer?
Patients with intestinal tumors can be treated at any stage of cancer. The chances of complete relief from malignant pathology remain even in the most advanced cases.
Colon cancer with metastases: how long do patients live?
Without medical care, the life of a patient with metastases to other organs is 6-11 months, depending on the rate of development of secondary tumors. When completing a course of treatment, the five-year survival rate in patients with metastases is 30-45%, i.e. at least thirty people out of a hundred live more than five years after surgery.
Attention! You can cure this disease for free and receive medical care at JSC "Medicine" (clinic of Academician Roitberg) under the State Guarantees program of Compulsory Medical Insurance (Compulsory Medical Insurance) and High-Tech Medical Care. To find out more, please call +7(495) 775-73-60, or on the VMP page for compulsory medical insurance
Rehabilitation
In the first few days after surgery, the patient is given intravenous nutrition. In the future, it is necessary to adhere to special nutritional principles, consuming only liquid and pureed foods. A special diet for intestinal cancer is prescribed taking into account the individual characteristics of the body, but the menu must include liquid dishes, fresh and boiled vegetables and fruits. In addition, during the recovery period it is necessary to avoid physical and psychological stress, regularly visit a doctor, and take prescribed tests.
List of sources
- Tsukanov A.S., Shelygin Yu.A., Achkasov S.I., Frolov S.A., Kashnikov V.N., Kuzminov A.M., Pikunov D.Yu., Shubin V.P. Principles of diagnosis and personalized treatment of hereditary forms of colorectal cancer. Bulletin of the Russian Academy of Medical Sciences. — 2019
- Association of Oncologists of Russia. Practical recommendations for drug treatment of patients with colon cancer. — 2014
- V.V. Martynyuk. Colon cancer (morbidity, mortality, risk factors, screening). St. Petersburg Medical Academy of Postgraduate Education. — 2000
Is an MRI of the intestines informative?
The method well visualizes the condition of the walls of the thin and thick sections, shows other organs of the abdominal cavity and small pelvis. MRI of the intestine is informative in identifying:
- adhesions;
- ulcerative processes;
- intestinal endometriosis (not found in men);
- oncological diseases;
- pathologies of the blood vessels of the abdominal cavity and pelvis;
- foreign bodies
Vascular pathologies, ulcers of the mucous membrane, malignant neoplasms can cause bleeding. In this case, treatment largely depends on what the intestinal MRI shows.
The method helps determine the etiology of the pathological process by visualizing the features of innervation, blood supply, structure of the digestive system and surrounding organs. Based on layer-by-layer photographs taken in three projections, the doctor can reconstruct a 3D model of the department in question. A three-dimensional MRI image shows how the intestinal loops are located in the abdominal cavity and pelvic area.
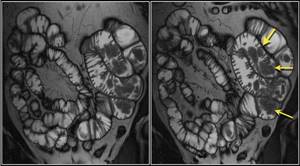
Peutz-Jeghers syndrome (arrows indicate multiple polyps)