August 11, 2016
Some of the myths about mammograms can have a serious impact on your long-term health. Find out what's really behind this vital research.
Think it's no big deal if you miss your annual mammogram this year? Or are you concerned that too much radiation is used during mammograms?
Annual mammograms for women 40 years of age and older help detect breast cancer at an early stage, which allows for less aggressive treatment in the future and ensures a higher survival rate.
Types of research and equipment used
The X-ray examination method is highly accurate, specific, and informative. The results of mammography of the mammary glands form the basis for diagnosing organ pathologies.
The set of equipment for the procedure consists of:
- mammograph;
- laboratory assistant workstation;
- digital detector;
- printer;
- doctor's workstation.
Devices are constantly being improved; modern equipment makes it possible to detect breast cancer at the very beginning of tumor formation from altered organ cells. Today, doctors detect up to 96% of breast pathologies in the early stages, compared to 80% diagnosed 10 years ago.
Radiologists use two types of mammographs:
- analogue (film)
- images of organs obtained by passing X-rays through tissue are transferred to film. Such devices are cheaper, but exclude the possibility of editing the image, transferring it to various media, or transferring it over the Internet for consultations with specialized oncologists; - digital mammographs
- display a “picture” on a computer monitor. It is saved as a graphic file. The devices operate at a reduced dose of radiation and allow you to quickly transfer images of the organ to the attending physician. It is convenient to work with them, zoom in or zoom in on the problem area, and make changes to the description. However, the clarity of a digital image is somewhat inferior to an analog photograph.
Tumor diagnosis is carried out in several ways and, if necessary, combined with other methods. For breast cancer, the doctor can use the following types of mammographic examination of the breast:
- with tomosynthesis – produces a layer-by-layer image of tissues, makes it possible to evaluate contours and comparative analysis of different projections of the “picture”;
- projection optical procedure - identifies malignant tumors, determines the type of their cells due to the effects of infrared radiation, provides two projections of images;
- with a biopsy attachment - designed for targeted examination of changes in the formation with the collection of suspicious tissues for histological analysis;
- tomographic optical - provides a three-dimensional image of the organ, outlines the specific location of the tumor, the main characteristics of oncopathology;
- luminescent procedure - involves the use of special marker substances that color pathological structures, which improves the visualization of malignant formations, as well as metastases;
- MRI mammography of the breast is considered one of the most informative methods for diagnosing breast cancer;
- radiothermometry - uses the penetrating ability of microwaves, the condition of cells is assessed based on temperature indicators of pathological tumor tissues. Together with the classical technique, radiothermometry detects breast cancer at any stage of the formation of the primary focus.
Mammographic diagnosis of breast cancer cannot be called completely safe, but modern devices allow the procedure to be carried out with minimal radiation exposure to the body. If you follow safety rules and frequency of manipulations, they will not cause harm to health. The diagnostic value of the analysis is very high.
What diseases does mammography detect?
The information content of the mammography method makes it possible to identify tumor-like formations of a benign or malignant nature in the early stages. Using a mammographic examination, tumors can be identified in more than 86% of cases. But the most important advantage of this method is the detection of cancer in the early stages in more than half of cases, when the mammologist is not able to detect the tumor by palpation, and the woman herself does not feel any changes. And yet, in 14% of cases, mammographic examination cannot detect signs of tumors, and then the mammologist prescribes additional research through pneumocystography or ductography.
Indications for diagnostics
Examination of the mammary glands with a mammograph can be both a preventive and diagnostic procedure. The first ones are intended for early primary detection of pathological changes. They are indicated for all patients over 40 years of age.
Young girls undergo routine mammography in the following situations:
- belonging to a risk group for breast cancer (bad heredity);
- infertility in women;
- detection of malignant tumors of the uterus, ovaries, metastases in the lungs, lymph nodes, bones, and other internal organs;
- disruption of the endocrine system.
The only contraindication to manipulation is pregnancy at any stage. During breastfeeding, a mammography procedure is permitted, but is not very informative.
An extraordinary diagnostic examination is prescribed for the patient’s complaints such as:
- detection of palpable formations of varying density in the mammary gland;
- bleeding from the nipple;
- deformation of any part of the chest;
- soreness of the nodes;
- pronounced asymmetry of organs;
- local change in shade, dry skin;
- swelling of tissues;
- nipple retraction.
Examination of organs with a mammograph is necessary after breast surgery to clarify the location of scar tissue. This information will help distinguish scarring from pathological changes in organ cells. After removal of a malignant breast tumor, the scars are examined in more detail on X-rays because they are a high-risk area.
Sometimes breast x-rays help girls overcome cancerophobia - an obsessive fear of developing cancer. The condition, of course, does not provoke the appearance of a pathologically altered formation, however, it significantly reduces the woman’s quality of life.
It is advisable to undergo the examination no more than once a year. Emergency situations allow the number of mammography procedures to increase to three during the same period. When more frequent monitoring is required, it is better to use other methods for diagnosing breast cancer (for example, ultrasound).
Tips for self-palpation of the breast
The best time for examination for young women is approximately 10 days after the start of the period, when the tissues become especially soft. It takes about three months to become more familiar with the nature of your own breasts because the tissue changes during your cycle. First you need to look at your breasts in the mirror: have their shape or size changed? This is followed by palpation, which is best done in the shower, after washing the chest.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter
What does a mammogram show?

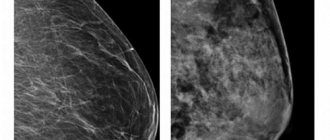
Studying the image, the doctor analyzes all possible changes in breast tissue. Pays special attention to tumor formations, as well as calcifications - bright white spots. It is not possible to find them using ultrasound.
Oncologists distinguish two types of calcifications:
- macrocalcifications
- large deposits of the element are usually formed in women over 50 years old and are associated with age-related changes in the body, injuries, and inflammatory processes. The formations are benign and do not require additional examinations; - microcalcifications
- tiny accumulations of mineral carry the risk of malignancy. Malignant inclusions differ from the safe form by localization. A biopsy is usually not required, but the patient will most likely need additional testing.
Mammography reveals benign formations:
- mastopathy of various forms - fibrocystic non-malignant changes of a hormone-dependent nature with or without atypical cells. Conditions require constant monitoring by specialists, tracking cell changes, treatment;
- Cysts are capsules filled with fluid and can be single or multiple. Simple ones do not pose a threat. If multi-chamber, large formations are detected, it may be necessary to clarify their status and analyze the contents of the cavities using a biopsy;
- papillomas inside the milk ducts are noncancerous growths. They are dangerous because they can ulcerate, bleed, and create favorable conditions for the onset of the inflammatory process;
- fibroadenoma is a benign tumor formed from healthy breast cells. When the formation reaches a large size, it is cut off surgically.
The main advantage of the mammographic method of hardware diagnosis of breast cancer is the ability to visually assess the number and structure of malignant cells. The procedure is often the starting point in identifying breast diseases and helps determine cancer treatment tactics.
conclusions
Today, mammography is one of the most accurate ways to detect tumor formation in the breast. Mammography makes it possible to obtain the maximum amount of information about the condition of breast tissue.

When comparing mammography with ultrasound and other modern research methods, many experts agree that the effectiveness and reliability of mammography results is much higher.
We invite you to familiarize yourself with the catalog on the website. Today you can make a call and buy any equipment from us!
How to prepare for the procedure
The manipulation does not require special preparation. The reliability of the study does not depend on the functioning of the digestive system or blood composition. Accordingly, there are no recommendations prohibiting eating or drinking before the procedure.
On the day of a mammogram, it is advisable for a woman to refrain from using antiperspirants, talcs, and other antiperspirants. On photographs, their remains are sometimes displayed as dark spots, which the oncologist may mistakenly mistake for malignant formations. Before the procedure, the girl must remove any jewelry from her neck and raise her hair.
The doctor or laboratory assistant will first interview the patient, make sure that the woman is not pregnant, and clarify the phase of the menstrual cycle. To obtain the most correct interpretation of the received data, you need to bring the results of previously conducted examinations (ultrasound, MRI, and others). It is permissible to undergo other x-ray procedures at least every other day so as not to exceed the radiation dose to the body.
Analog X-ray diagnostics
In this case, analog mammography systems are used to conduct research. The X-rays are projected onto a special film, which is why such equipment is also called “film”.
You might be interested!
|
|
| Planmed Sophie Classic analogue mammograph with intelligent Flex AEC concept | Analogue mammograph Genoray MX-300 with 19-level compression |
The advantage of this type of research is the medical staff’s many years of experience working with analog mammographs. Another plus is the affordable price.
Among the disadvantages, experts highlight the limited capabilities, since after receiving the image on film, other manipulations will be unacceptable.
However, the problem is solved with the help of digitizers, who help convert images into digital format.
Manipulation technique
Mammography takes place in the X-ray room. The woman stands or sits near the device (the position depends on the design of the device). The mammary glands are placed on a special plate and pressed on top with another bar.
The girl's waist area is covered with a protective lead apron. The laboratory assistant and doctor leave the office and remotely activate the equipment. Both breasts must be examined, even when suspicious lumps are found in one of them.
If necessary, the patient additionally takes photographs of the organ in an oblique or lateral projection. Sometimes targeted mammography is required - an enlarged x-ray of the tissues of the detected suspicious formation, milk ducts or organ lobules. The manipulation lasts from 5 to 10 minutes.
Within several hours after an X-ray examination of the breast, a woman may experience pain in the area of exposure caused by mechanical compression of the gland by the plates during the procedure. This is a normal phenomenon that goes away on its own without treatment.
For some time, the doctor deciphers the examination data, then the woman goes home. Images of organ tissue, as well as descriptions of them, can usually be obtained within a few minutes after the examination. The results must be shown to the attending physician to analyze the situation, prescribe treatment, and further monitor the possible malignant changes in the cells of the organ.
Reliability of the method
Undoubtedly, mammography is an effective way to examine the mammary glands, but it also has some limitations. Thus, the reliability of the method decreases:
- with small breast size
- if the woman is young (under 30 years old).
In addition, a mammography examination is not performed if a woman has undergone aesthetic breast augmentation surgery with implants. In order to conduct the study, no special preparation is required, but the pain that accompanies mammography cannot be called just discomfort. The procedure is, of course, a little painful, since the mammary glands are compressed between the plates, but this is what makes it possible to identify malignant neoplasms and benign tumors, so you can and should be patient for a few minutes. The most important thing is that there should be no damage or complications after mammography.
Interpretation of mammography results

Breast diagnostic data is provided in the form of visual images indicating detected (or not) deviations from the norm. Features of the structure of breast tissue are indicated by letters of the Latin alphabet:
- A – most of the organ is adipose tissue;
- B – fatty structure interspersed with fibrous and glandular fibers;
- C – the breast consists of an approximately equal number of glandular, fibrous, fat cells;
- D – only fibrous, glandular tissues were found.
During a breast examination, the doctor also directly analyzes the formations, if they are present in the breast. The assessment is carried out using the BI-RADS scale. It is divided into several categories, indicated by numbers, depending on the level of likelihood of developing breast cancer.
BI-RADS - 0
The designation is used when deviations from the norm are possible, but the photograph is not sufficiently informative.
The woman is prescribed additional examinations of the organ (for example, ultrasound or repeat mammography). A comparative analysis with data from previous diagnostic procedures is also carried out, aimed at tracking changes in breast cells.
BI-RADS - 1
Negative test result, glandular tissue is within normal limits. The transcript indicates the absence of malignant changes. The breasts are symmetrical, there are no suspicious tumors of the breast, as well as any discomfort in the woman.
BI-RADS - 2
Presence of benign nodes. The result is also considered negative, since it “indicates” that there are no signs of breast cancer.
The study data must be saved so that the doctor can monitor the dynamics of possible malignant changes in the formation.
BI-RADS - 3
This category includes tumors that turn out to be benign in 98% of cases, but are not clearly differentiated from cancer.
Girls with such results are advised to be monitored by an oncologist and have a repeat mammogram in six months. The procedure is repeated until the formation is stabilized and the patient is given an accurate diagnosis. The process of examining breast tissue can last up to two years.
Periodic manipulation allows women with a BI-RADS result of 3 to avoid “unnecessary” biopsies. Helps to notice negative changes in cells at the initial stage of disease development (when the probability of degeneration is 20-30%), and timely take measures aimed at stopping the development of cancer.
BI-RADS - 4
A suspicious tumor was discovered. According to the degree of likelihood of malignancy, doctors divide the results of this group into three categories:
- 4A - low risk;
- 4B - average probability of cancer;
- 4C - high risk of malignancy of the seal.
To clarify the nature of the detected tumor, a biopsy is required.
BI-RADS - 5
Decoding the results of the study indicates a 95% probability of a malignant neoplasm. The woman must be sent for a biopsy.
Problems of modern mammography
Many modern mammographs used today in specialized centers and multidisciplinary clinics can operate with reduced radiation exposure.
Mammography Safety
Despite the advent of modern equipment with minimal radiation doses, mammography is not becoming a completely safe procedure. Negative effects on the body during mammography cannot be completely excluded.
The modern task is to create the necessary and maximally safe conditions for conducting research, reducing the risk of possible complications for the health of patients and medical personnel.
Discomfort during mammography
Another problem is the discomfort that some patients experience during the study.
To obtain a high-quality image, the mammary gland must be tightly compressed with special plates, so with certain types of diseases women may experience pain and severe discomfort.
Modern technologies can reduce compression of the breast during mammography. Manufacturers have recently increasingly produced mammographs with this function.