What is a tooth root cyst?
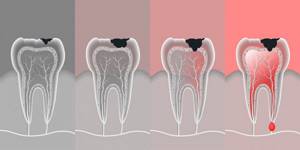
A cyst is an advanced form of inflammation of the tooth ligament.
There are several types of jaw cysts, but the most common is odontogenic, i.e. tooth root cyst. We will talk about it in this article.
It is of an infectious-inflammatory nature, i.e. is a consequence of “no treatment” or poor treatment of the tooth.
Translated from Greek, “cyst” means “bubble”. Morphologically, it is a cavity with a fibrous wall and contents. Simply put, a sac under problem roots filled with inflammatory fluid (for example, pus). Its dimensions vary from a few millimeters to several centimeters. The cyst that appears is attached to the apex of the tooth root and is located in the periodontal space - between the root and the bone tissue.
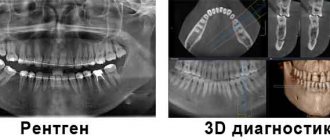
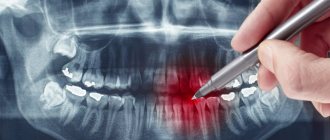
The X-ray image shows an area of bone tissue destruction (a large “dark cavity” adjacent to the root of the tooth). This is a cyst.
Removal of a dental cyst. Historically significant and modern methods of surgery for removing dental cysts
Initially, the most common method of treating cysts was their removal. For this purpose, 2 fundamentally different methods were used: cystotomy and cystectomy.
Cystotomy (or the PARCH-I method) has historical significance in the development and establishment of medicine. Today this method is practically not used, but previously it was indispensable for removing large cysts. To avoid complications and its severe consequences, a wide channel was created between the cyst cavity and the vestibule of the oral cavity by suturing the edges of the cyst shell with the oral mucosa.
Cystectomy (or PARCH-II method) involves complete excision/removal of the cyst. This surgical intervention is often simultaneously accompanied by the removal of the root apex, the source of the formation of the cyst containing infected apical deltas. Today this method is the most popular.
The main goal of cystectomy is complete sanitation of the cyst cavity, which is not possible without resection of the root apex. The fact is that the root pulp in its apical third has an apical delta with an unclear structure and very fine branching of the canals, even in single-rooted teeth. If such canals can be cleaned during tooth treatment, then during retreatment this is almost impossible, especially considering the narrowness of the lateral deltas. Removing the root apex, in addition, allows you to most effectively clean the cyst cavity behind the root. This is especially true for teeth 12 and 22, which have a more curved root system. The operation is carried out as follows: using a small incision on the gum, the surgeon very carefully reaches the surface of the bone located above the cystic cavity, removes the wall with a trephine or bur, making sure that the neighboring teeth are not damaged, and then removes the cyst shell and performs a resection of the root apex . Next, sanitation of the cystic cavity is carried out and its subsequent revision for residual cyst particles. After this, in some cases, retrograde filling is performed. The final step in the operation to remove cystic formations is filling the resulting cavity with osteoplastic material and suturing the wound.
In the case of the formation of a large cyst, amputation of the apex of the tooth root can be performed, or half of the tooth and damaged root can be removed (hemessection), and in the case of an interradicular cyst, this can be done by corono-radicular separation.
Why does a cyst occur?
Most often, a cyst is associated with an infection in the canals of the tooth. If caries and its complications (pulpitis, periodontitis) are not treated promptly, then microorganisms (bacteria, viruses, etc.) that live in the root canals of carious teeth sooner or later penetrate into the surrounding bone tissue. The body of a healthy person builds a barrier against microflora, which is the shell of the cyst. In this way, it tries to localize and isolate pathogenic microbes, preventing them from spreading further. The cyst zone is nothing more than the front line in which the body fights the infection, and military action is the infectious inflammatory process.
As long as the infection persists, that is, as long as the body has someone to fight with, the cyst will exist and grow.
Other causes of dental cysts may be:
- Tooth injury.
- Incompetent treatment of the root canals of the tooth, namely poor-quality mechanical and medicinal treatment of the canals or poor-quality filling of the canal (in particular, loose filling, with voids that are very quickly filled with bacteria, which can ultimately lead to a dental cyst.
Causes of dental cysts
The main reasons for the appearance of formations include injuries and infection - for example, due to insufficiently thorough treatment and filling of tooth canals when removing nerves or when working with poorly sterilized instruments. If the patient’s immunity is weakened due to acute respiratory viral infections or other diseases, the likelihood of developing a pathological process increases. Cysts arise as a result of chronic sinusitis and other ENT diseases of a bacterial nature. The infection spreads to the teeth and gums through the bloodstream.
Other reasons for appearance:
- tooth injury from hard food or mechanical impact;
- untreated complicated caries;
- improper prosthetics, due to which the tooth was overloaded;
- periodontitis and periodontitis, dangerous due to the development of inflammation;
- pathology of jaw development, atypical teething, including wisdom teeth, and so on.
Regardless of the etiology, cysts must be treated immediately, resorting to highly professional help. However, before this, the pathology must be identified by correctly diagnosing the symptoms.

How does a cyst manifest itself?
The insidiousness of a dental cyst lies in the fact that its appearance at first is almost asymptomatic. It makes itself felt when the purulent sac has already reached a fairly large size. Exacerbation of inflammation and the manifestation of cysts occurs when the immune system is weakened. It is often learned about during acute respiratory viral diseases, when the body weakens due to the fight against the disease. So, we list the possible symptoms of a dental cyst:
- acute toothache appears;
- swelling and swelling of the gums and cheeks;
- increased body temperature;
- weakness;
- general malaise;
- a fistulous tract may appear on the gum, through which pus from the cyst will enter the oral cavity;
- absence of visible symptoms (the cyst does not manifest itself in any way and is discovered by chance on x-rays).
If outwardly the tooth looks completely healthy and the patient does not experience any discomfort or pain, this does not indicate that the tooth is healthy. A cyst is one of the pathologies that does not always occur with any clinical manifestations. However, the consequences can be quite dire, both for the tooth itself and for the tissues surrounding it.
A dental cyst is diagnosed based on the results of radiography. On an x-ray, it looks like a dark spot at the apex of the root, in other words, like a black ball. Sometimes pathology is discovered completely by accident, when examining a neighboring tooth or during a routine preventive examination at an appointment with a dentist or ENT doctor during an examination of the maxillary sinuses.

An x-ray of all teeth (orthopantomogram) shows a zone of bone tissue destruction (“black ball” adjacent to the root of the tooth). This is a cyst.
Symptoms of a dental cyst
At the very beginning of cyst formation, there may be no symptoms. The presence of a neoplasm can be suspected by the occurrence of periodic pain when loading the affected tooth, the appearance of increased sensitivity to cold and hot foods and drinks, and soreness of the gums in the area of the affected tooth.
In addition, symptoms of a dental cyst may include:
- Changes in enamel color.
- The appearance of bad breath.
- A feeling of tightness in the area of the diseased tooth.
- Swelling of the soft tissue around the cyst.
- The appearance of a bump on the gum or palate. This symptom appears if the cyst reaches a sufficiently large size.
- It becomes impossible to eliminate the pain with painkillers.
If you have several symptoms, you should immediately consult a doctor for diagnosis and treatment.
How to treat a tooth with a cyst?
There are 2 fundamentally different ways to treat dental cysts:
Therapeutic and surgical.
- Therapeutic method : treatment of tooth canals, as a result of which the cyst disappears. As a rule, it takes several visits to the doctor, ranging from 2 weeks to six months.
It is carried out by a dentist-therapist, whose main task is to remove the infection from the root canals, that is, to eliminate the factor supporting the cyst. After root canal treatment, temporary medications are left in them, which act on the cyst and contribute to its regression and complete disappearance. At the end of treatment, the root canals are filled with permanent materials and the damaged tooth is restored. Subsequent dynamic monitoring of the tooth is also necessary, which consists of visiting the dentist every six months, and X-ray monitoring.
- The surgical method is to remove the tooth root cyst. It is used when the therapeutic technique is ineffective.
There are 2 types of surgical techniques:
- Removal of the cyst, preserving the causative tooth.
- Removal of the cyst along with the causative tooth.
Preserving a tooth is advisable only if the causative tooth is not severely damaged and does not cause inflammation in neighboring organs and spaces.
The cyst is removed by a dental surgeon under local anesthesia.
Types of dental cysts
There are several types of molar cysts, which are classified according to location and depending on the reasons for their formation.
Depending on the location, the following types of cysts are divided:
- A cyst on the root of a tooth: it can be interradicular, peri-radicular and basal. With a tooth root cyst, symptoms do not appear for a long time, and only at a late stage does a purulent capsule form and pain appear.
- Cyst on the gum: with this type of dental cyst, the fistula can form in any area of the gums; filling with pus occurs a little later. A cyst near a tooth may be accompanied by a tingling sensation. As with other cases of fistula formation, the consequences of a cyst in the gum of a tooth are quite serious.
- A dental cyst in the maxillary sinus: can only be diagnosed with the help of special equipment, since otherwise it is impossible to notice even a large dental cyst in the maxillary sinus. With an advanced dental cyst, sinusitis can become a sad and very unpleasant consequence.
- Cyst under the crown of a tooth: most often this is a cyst after dental treatment that was unsuccessful. In this case, a bubble is formed when the crown is installed incorrectly - as a result of the accumulation of food and the proliferation of bacteria. It is quite difficult to detect this type of cyst at an early stage. To treat a tooth cyst with a crown, the latter will need to be removed.
- Wisdom tooth cyst: appears as a result of difficult eruption or chronic inflammation of the “eights”. The only treatment option is to remove the affected tooth.
The cyst of the front tooth should be specially noted. In general, the disease does not differ greatly from other types, however, due to the fact that the teeth in the anterior section are much narrower, this affects the volume of the surrounding soft tissues. Therefore, an upper tooth cyst (or a lower tooth cyst) in the front part of the jaw has much less room for localization, and it begins to come out only in the gum area. For comparison, a cyst on the back teeth can form a fistulous tract even through the cheek or neck.
According to the reasons for their appearance, the following types of cysts are distinguished:
- Radicular
or odontogenic dental cyst: the most common type. It is formed in the upper third of the dental root from a granuloma - as a result of pulp necrosis and periapical (at the root apex) inflammation. The diameter of a radicular dental cyst varies from 2 mm to 3 cm. If there is no secondary inflammation, the disease is asymptomatic, there is no displacement of teeth or effects on bone tissue. - Residual
: a cyst after tooth extraction, formed in a situation where the root apex was not completely removed or a granuloma formed in the area of the missing tooth. A cyst after tooth extraction has the same properties as a radicular one. - Keratocyst
, also called primary and primordial: formed due to a developmental disorder. No tooth is immune from this, but most often it is a cyst due to inflammation in the area of the premolars and third molar of the lower jaw. With its development, the likelihood of relapse is high. - Teething cyst
, or retention cyst: is formed during the period of replacement of primary dental units with permanent ones. A tooth retention cyst looks like a bluish swelling that contains blood inside. In most cases, the fistula is formed due to slow eruption and can open at any time. - Follicular
: formed in a situation where a tooth for some reason cannot erupt and grows inside the soft tissue. As a result, a cyst forms on the gum around the tooth. Such a cyst grows quickly, can move to other teeth and is fraught with extensive damage to them. With the development of a follicular dental cyst, complications can be expressed in the tilting of adjacent teeth, displacement of unerupted teeth, and root resorption. - Lateral periodontal
: the exact causes of occurrence are not fully determined. As a rule, these are small cysts associated with the lateral surface of the tooth root. - Calcifying odontogenic
: formed in the area of the supporting surface mainly of the lower jaw. The reasons for its appearance are also not fully understood.

How to choose a cyst treatment method? Who chooses it and what does it depend on?
The choice of treatment method for the cyst is made by the dentist, according to the specific clinical situation. The method depends on:
- preservation of tooth tissue (if the tooth cannot be restored after treatment of the cyst, choose a surgical method with removal of the cyst);
- on the anatomy of root canals and the ability to process them efficiently;
- from the availability of good equipment and equipment in the clinic (for example, a dental microscope, etc.), which allows you to go through root canals and process them efficiently;
- on the patient’s health and the presence of chronic diseases;
- on the duration of existence of the cyst;
- on the skills of a particular specialist.
How to reduce the risk of cysts
The risk of cysts is reduced if prevention is carried out correctly:
- visit the dentist to examine your teeth and gums twice a year, do not delay the treatment of caries and other diseases;
- carefully carry out dental and oral hygiene;
- maintain immunity to avoid infectious diseases that cause cysts.
If you still need treatment, the doctors of the Mazot clinic will help you. They have advanced equipment, including laser, and are able to carry out all dental manipulations.
Specialists will deal with the cyst and do everything to ensure that the patient avoids surgery. Make an appointment
How successful is the prognosis for treatment of cysts and what does it depend on?
Surgical and therapeutic methods of treatment give excellent results, provided they are performed correctly and with high quality.
The success of treatment (and this is what we call the preservation of the causative tooth and the complete disappearance of the cyst) also depends on the following factors:
- on the anatomy of root canals and the ability to process them efficiently;
- from the availability of good equipment and equipment in the clinic (for example, a dental microscope, etc.), which allows you to go through root canals and process them efficiently;
- on the patient’s health and the presence of chronic diseases;
- duration of existence of the cyst;
- on the skills, abilities and experience of a particular specialist.
Are folk remedies effective in treating dental cysts?
Because of the fear of pain when visiting the dentist's office, some people try to cure a cyst on their own and look for recipes for this of all kinds of folk remedies, learning them from friends or reading them on the Internet. Doing this is not only useless, but also unsafe. It is important to understand that the formation of a cyst is always provoked by infection of the root canals of the tooth, and in some cases, the most modern and potent professional pharmaceuticals are useless against the infection. In addition, high-quality treatment of dental cysts always involves removing the affected tissue and thoroughly flushing the canals. Without these manipulations, the cyst will not disappear anywhere - on the contrary, it will only grow.
If the cyst grows significantly, it is impossible to remove it and save the tooth. In addition, as the inflammatory process progresses, other negative health consequences may occur. Therefore, even with the initial symptoms of the appearance of a formation, you should not hesitate. Call and make an appointment with the specialists of our dental clinic in Moscow - Vanstom! We are located in the center of Moscow, next to the Baumanskaya metro station.
What happens if a tooth with a cyst is not treated? What's wrong with a cyst? Consequences of a tooth root cyst
- The cyst is prone to growth, and as it grows, it destroys the surrounding bone and disrupts anatomical formations (for example, the lower wall of the maxillary sinus, provoking the development of sinusitis, etc.).
- The cyst can fester, and the inflammatory process spreads into the surrounding spaces, causing serious complications that threaten the patient’s life (abscesses, phlegmon, etc.).
- As the cyst grows, it can push away neighboring teeth and significantly change their position.
- The cyst can lead to a pathological fracture of the jaw if it reaches a very large size.
- The cyst can eventually lead to tooth loss.
Traditional methods of treating cysts
It is necessary to understand that a cyst is not just inflamed tissue in which you can overcome the inflammation and everything will heal on its own. A cyst is a formation that arises from tissues that are not in the place where they are supposed to be. Any anti-inflammatory drugs (or traditional methods) can relieve an exacerbation, but it is impossible to remove foreign tissue. In addition, active treatment with traditional methods can lead to a “blurred” picture of the disease and difficulty in diagnosing and choosing the optimal treatment tactics.
After treatment of a cyst, the tooth hurts, is this possible? And if so, what time is considered the norm?
Of course, immediately after treatment the tooth may bother the patient, this is natural. However, this does not always happen.
Normally, after treatment of a tooth with a cyst, the tooth either does not hurt at all or bothers you for 1-2 days.
If after dental treatment the pain persists and does not decrease for more than 2 days, we advise you to inform your doctor about this.
During treatment, an exacerbation of the inflammatory process may occur, which passes over time and this does not mean that the treatment is unsuccessful. The presence of an exacerbation depends on how aggressive the microbial flora lived in the root canal and on the patient’s immune strength.
Pain after treatment is stronger if the tooth began to be treated during an exacerbation of the inflammatory process. Therefore, our advice to you, dear patients, is not to let it get to the point where pain occurs (as most people mistakenly do). Start treatment while nothing hurts, during a calm period. It will be easier for you, and there may be no pain at all after the intervention.
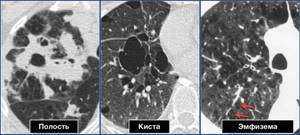
Cysts, cavities, emphysema - differential diagnosis
Radiologists use a variety of terms to describe low-density lung changes or areas of clearing such as cysts, cavities, pneumatoceles, emphysema, bullae, honeycombing, and others.
A large number of terms makes it difficult to generally understand the pathological process in the lungs, so it is more practical to use the following terms.
- Cavity - pathological cavity formation with thick walls
- Cyst is a pathological cavity formation with thin walls
- Emphysema is a pathological cavity formation with invisible walls
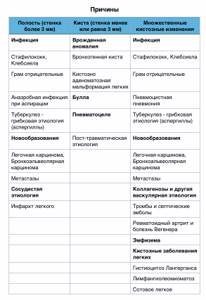
Cavities occur due to necrosis in formations or areas of consolidation. Sometimes it is difficult to distinguish a cyst from a cavity. Also, after treatment of the patient, the cavity in the lung turns into a cyst, and vice versa, the cyst can become infected and visualized as a cavity. There are cases when emphysematous bullae have visible walls, the thickness of which is up to 1 mm. To make a differential diagnosis in this case, the surrounding pulmonary parenchyma should be assessed. Imaging of pulmonary cysts does not reveal concomitant emphysema. Cysts usually contain air, less often fluid and a solid component. This term is most often used to describe thin-walled air spaces in the lungs of patients with lymphangioleiomyomatosis or histiocytosis. Thicker cyst walls are found in patients with honeycomb lung, which is a sign of advanced fibrosis.
CAVITIES
Pneumonia
In virulent pyogenic infections an abscess may form within the consolidated lung as a result of necrosis due to vasculitis and thrombosis.
When patients cough up pus, cavities can be identified on x-rays. As a rule, the condition of these patients is assessed as poor.
In granulomatous diseases such as tuberculosis, cavities are also detected, but the patient often feels satisfactory.
Cavities are not detected in pneumonia of viral etiology and mycoplasma, and are also rarely visualized in streptococcal pneumonia.
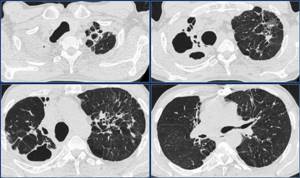
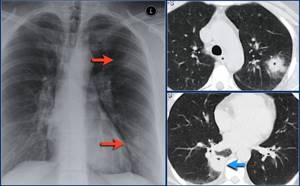
Below are images of a young patient with pneumonia. One month after treatment, follow-up images show that the consolidation and cavity have resolved.

Pneumonia
Below is another example of cavity pneumonia.
Note the lesion in the lung parenchyma, which is clearly visible on CT.
Follow-up images one year later show minimal changes on the radiograph.

Tuberculosis
Primary tuberculosis is usually clinically asymptomatic and asymptomatic for a long time.
The immunity of 5% of infected people does not cope well, which is favorable for the development of the disease.
Secondary tuberculosis develops in 5% of cases in latent carriers, which on an x-ray often appears as consolidation with a decay cavity mainly in the upper and lower lobes of the lungs. Milliary tuberculosis is the result of hematogenous spread of the disease.
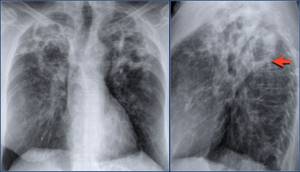
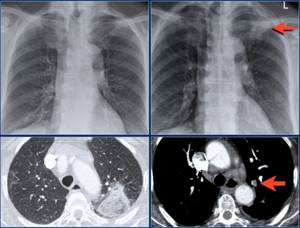
Below is a patient with secondary tuberculosis with a decay cavity in the upper lobe of the left lung.
Tuberculosis
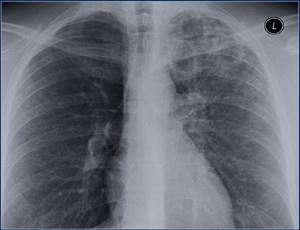
Please evaluate the images first and then continue reading.
Found:
- Cavities in the upper lobe of the right lung
- Multiple, ill-defined densities, likely small consolidations.
X-ray of the same patient several years later.
- Atelectasis of the upper lobe of the right lung
- Tracheal deviation
- Cavity and fibrous changes in the upper lobe.
- Minimal fibrosis and cavitation are visualized in the upper lobe of the left lung.
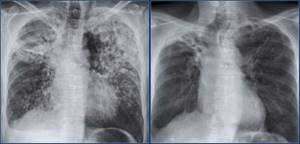
Changes are best assessed on CT.
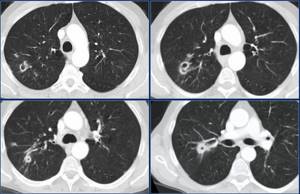
Below is the same patient as above.
Note the cavity in the right lung. The left lung most likely has traction bronchiectasis due to fibrosis.
Non-tuberculous mycobacteriosis
Nontuberculous mycobacterium, also known as atypical mycobacterium. Below is a patient with a bilateral pathological process in the upper lobes of the lungs, which is caused by infection with non-tuberculous mycobacterium. Pay attention to the fluid content (pus) in the cavity (indicated by the arrow).
Below is another patient with lung damage from an atypical mycobacterium. Note the nodules and cavitation and continue to evaluate the CT image.
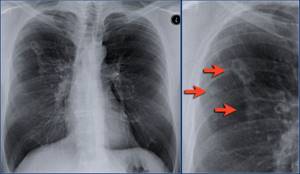
CT visualizes multiple small cavities.
Septic pneumonia
Septic pneumonia is visualized as multiple mild lesions. In 50% cavities are detected. CT images reveal many more pathological changes than radiographs. Typically, these changes are localized along the periphery of the lungs, adjacent to the pleura. The air bronchogram symptom and the feeding vessel symptom are also visualized. Although many argue about the latter.
Below is a patient with septic pneumonia. The x-ray shows two subtle high-density changes in the left lung, which are most likely consolidation.
Below are repeat images of the same patient showing small cysts.

Pulmonary cancer
In 10% of lung cancer cases, cavities form, which is most typical for squamous cell carcinoma.
In small cell carcinoma, cavities do not form. Bronchoalveolar cancer (adenocarcinoma in situ) rarely develops cavities.
Below is an x-ray showing a large cavity in a patient with lung cancer.

Pulmonary infarction
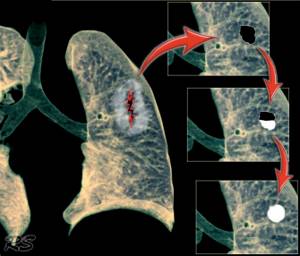
Pulmonary embolism does not typically manifest as pulmonary consolidation on a radiograph. Consolidation is usually the result of pulmonary infarction and alveolar hemorrhage. In this case, a cyst forms in the area of the infarction.
Below is an x-ray that is normal. The arrow indicates a triangular change in high-density pulmonary parenchyma, the cause of which is pulmonary embolism. On CT, these changes are segmental consolidation.
Below is the same patient in pictures a year later, whose cysts are detected. Thick walls are presumably due to an infected cyst.

PNEUMATOCELE
Pneumatoceles are thin-walled, air-filled cysts of the lung that usually do not require surgery unless there is difficulty breathing due to compression of the lung or rupture of the cysts into the pleural cavity. Pneumatocele most often develops in very young children with pneumonia caused by Staphylococcus aureus.
Pathology. Necrosis and melting of the pulmonary parenchyma leads to the development of pneumatocele. Staphylococcal pneumonia causes a severe inflammatory process, associated in part with the powerful destructive effect of staphylococcal exotoxin on lung tissue. Air escapes through the destroyed walls of the alveoli subpleurally, resulting in the formation of a typical thin-walled cyst.
Below is an illustration of the mechanism of pneumatocele formation in trauma. Due to the fluid in the cyst, these changes will appear similar to a solitary pulmonary lesion (nodule) on imaging.
Source
- Radiology Assistant
- Thoracic Imaging: Pulmonary And Cardiovascular Radiologyby Richard Webb and Charles Higgins
- Chest Radiology: Plain Film Patterns and Differential Diagnoses sixth editionby James C. Reed
- The Chest X-Ray: A Survival Guideby Gerald De Lacey, Simon Morley and Laurence Berman
- The Comet Tail Signby Vince A. Partap November 1999 Radiology,213, 553-554.
- Acute Pulmonary Thromboembolism: A Historical Perspectiveby Sudhakar NJ Pipavath1 and J. David Godwin. AJR September 2008 vol. 191 no. 3 639-641.
- Guidelines for Management of Small Pulmonary Nodules Detected on CT Scans: A Statement from the Fleischner Society by Heber MacMahon et al.Radiology 2005; 237:395-400
- Pulmonary septic emboli: diagnosis with CT.by JE Kuhlman, , EK Fishman, and , C TeigenRadiology 1990, volume 174, issue 1.
- High-Resolution MDCT of Pulmonary Septic Embolism: Evaluation of the Feeding Vessel Signby Jonathan Dodd et al AJR 2006; 187:623-629
- Pulmonary Tuberculosis: Up-to-Date Imaging and Managementby Yeon Joo Jeong et alAJR 2008; 191:834-844
- Bronchial Atresiaby Matthew G. Gipson et al September 2009 RadioGraphics,29, 1531-1535.
- Fleischner Society: Glossary of Terms for Thoracic Imaging