What do world statistics say?
The disease is diagnosed in 4-12% of adult females. Representatives of the European and American Society of Reproductive Medicine claim that the disorder occurs more often, in 15-20% of women of fertile age. In cases of infertility in marriage, this figure reaches 22%.
Today, there is active debate regarding the diagnostic criteria for polycystic ovary syndrome and the in vitro fertilization (IVF) procedure. Experts around the world consider the use of hormonal drugs to be an integral stage of treatment, especially when planning IVF for polycystic syndrome (PCOS).
Many modern doctors say that this problem is related to excess weight. After IVF for polycystic ovary syndrome, overweight women become pregnant half as often. That is why in the USA treatment begins only after the patient’s weight has been reduced by 5-7%. This measure increases the chances of successful IVF for PCOS by an average of 15-20%.
What is IVF?
The presence of the word “in vitro” in the name of the technique implies that fertilization is carried out outside the body of the mother of the unborn baby. This assisted reproductive technology includes a whole range of different procedures that lasts about two weeks.
The effectiveness of the IVF program is on average 30-40%. Most couples need to undergo several procedures to achieve the desired pregnancy. If the first IVF cycle ends in failure, this is not a reason to give up. On the contrary, a reproductologist will take into account all the features of the first cycle and analyze each stage, which will allow the risks to be taken into account in subsequent cycles.
The result of using the technique depends on a number of factors, including:
- Woman's age
- Causes of infertility and its duration
- Associated factors: the presence of various pathologies and diseases of internal organs, the current condition of sexual partners, the condition of the endometrium, the quality of eggs, genetic factors, lifestyle, the state of the man’s health
Causes of polycystic disease
The causes of PCOS include:
- frequent stress, depression;
- endocrine system disorders;
- improper metabolism;
- chronic infections;
- overweight;
- hereditary predisposition.
The disease can also develop in women who live for a long time in regions with poor ecology.
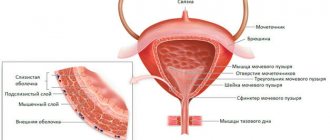
In the presence of one or more unfavorable factors, the ovarian capsules thicken and increase in size, under which numerous cystic formations begin to develop.
Advantages of carrying out the procedure at MEDSI
- Qualified specialists in the field of reproductive medicine.
Our doctors have extensive professional experience in Russia and abroad. They have all the necessary knowledge - Expert diagnostics.
To carry it out, clinics use advanced equipment that ensures high accuracy of all examinations. - Own laboratory.
It carries out all the necessary manipulations with biological material (analysis and processing of ejaculate, collection of eggs, fertilization, cultivation, etc.) - Preparation and implementation of IVF programs.
We have all the capabilities to solve problems associated with in vitro fertilization and provide an integrated approach to them - Providing a full range of services.
Our specialists provide not only the processes necessary for pregnancy, but also pregnancy management, as well as recovery after childbirth - Compliance with international standards.
Our laboratory provides optimal conditions for successful work with biomaterials (multi-stage air purification, maintaining pressure, temperature and humidity in rooms, constant automated monitoring of cultivation conditions) - Automated system for identifying biological material.
The FertiProof system is the first in Russia and guarantees the elimination of the human factor and “substitution” of biomaterial throughout all stages of the IVF program - Individual approach.
We offer an integrated approach and take into account all factors that may become barriers to the birth of a baby. The Center is staffed by a reproductive psychologist who will help ensure a confident path to results.
If you are planning to participate in the IVF program in Moscow, or want to find out the cost of medical care, call +7 (495) 7-800-500. Our specialist will answer all questions and make an appointment with a doctor.
Criteria and symptoms of the disease
Polycystic ovary syndrome is characterized by unpleasant symptoms that take the form of:
- excess of androgens;
- lack of ovulation;
- oily seborrhea;
- acne;
- baldness;
- hirsutism (male pattern hair growth).
Making a diagnosis of “polycystic disease” allows us to exclude other diseases, which include tumors of the ovaries, adrenal glands, Cushing’s syndrome, hyperprolactinemia, and hypothyroidism. When carrying out differential diagnostics, testosterone and thyroid-stimulating hormone are determined.
Against the background of polycystic ovary syndrome, the likelihood of developing pathologies of the heart and blood vessels increases (regardless of age). This is due to insulin resistance, a high risk of developing diabetes mellitus, dyslipidemia, arterial hypertension, and hypercoagulation. For this reason, women with a body mass index over 30, as well as a predisposition to diabetes and cardiovascular disorders, need to determine glucose tolerance, insulin levels, lipid profile and other diagnostic procedures.
The in vitro fertilization method may be prescribed to patients who have not improved within a year after surgery or drug therapy. Among these women, there are many who have succeeded in IVF for PCOS.
When is pregnancy confirmed?
The fact of conception can be confirmed after 14 days.
Pregnancy is determined using a special test that measures the content of the hCG hormone in the blood serum 10-14 days after the transfer. This hormone is synthesized only by embryonic cells. The first ultrasound is recommended to be performed a week after the day of the hCG test.
Important! In the future, the woman is also observed by specialists. If pregnancy occurs, it is supported by medications prescribed by the doctor. If the pregnancy test is negative, all medications must be stopped. Menstruation will come, which may differ from normal menstrual flow.
How is the syndrome treated?
When choosing a therapeutic strategy, doctors at Medical Plaza MC are guided by the woman’s reproductive plans. If future pregnancy is not envisaged, treatment will be aimed at regulating menstrual rhythm, eliminating symptoms of hirsutism, correcting metabolism, and preventing endometrial cancer. For women planning to become pregnant, therapy is indicated to treat infertility, mainly caused by absent ovulation.
If the patient is not overweight and is not interested in motherhood, the main treatment is the use of CHCs (combined hormonal contraceptives). These drugs include:
- Jess;
- Janine;
- Diana-35;
- Yarina;
- Belara;
- Midiana.
Before prescribing these drugs, screening for contraindications to drug therapy is carried out.
In women with overweight and varying degrees of obesity, the first stage of treatment is weight loss, which helps correct metabolic status, normalize the rhythm of menstruation and fertility. Such cases involve changing lifestyle, increasing physical activity, and adjusting diet.
Patients with hyperinsulinemia, glucose intolerance, and those susceptible to hyperstimulation syndrome are prescribed Metformin.
In the presence of anovulatory infertility, the main line of therapy becomes ovulation induction with antiestrogens. This rule applies to patients without intrauterine pathologies, with normal patency of the fallopian tubes and a healthy partner. Sometimes the method is combined with intrauterine insemination and requires at least 5 cycles.
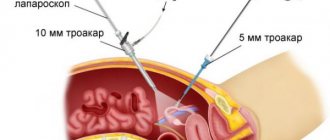
In case of insufficient effectiveness of conservative ovulation induction, there is a need for laparoscopy or ovarian cauterization. Thanks to surgical intervention, it is possible to identify and eliminate concomitant pathologies (in the form of adhesions, small forms of external genital endometriosis).
It is important to consider that ovarian surgery is only necessary to combat infertility with confirmed polycystic disease. Such manipulations do not correct the menstrual cycle and do not contribute to the recovery of patients with hyperandrogenism. It is also undesirable to perform repeated surgery.
After the operation, pregnancy occurs within 6 months or 1 year. If this type of treatment is still ineffective, it makes sense to turn to in vitro fertilization programs. In this case, preparation for IVF for PCOS, which consists of stimulating ovulation, becomes mandatory. Often, patients experience overly active growth of numerous small follicles that are unable to reach the required size and full maturity.
Sometimes laparoscopy or IVF for PCOS are used at the wrong time - too early, at the initial stage of diagnosis, or, conversely, too late. If in vitro fertilization programs are used too early at a young age, severe forms of ovarian hyperstimulation syndrome may occur. This is also fraught with multiple births and reproductive losses. If you turn to IVF late, the effectiveness of the procedure decreases due to prolonged previous therapy and the age factor.
Reasons for failure in IVF

Despite significant advances in the treatment of infertility over the past 30 years, the effectiveness of the best infertility treatment method today - IVF - remains, relative to patient expectations, low - 30-40%. The question: why good embryos do not want to take root in the uterus is still open.
The IVF program consists of several stages, and each of them must be successfully overcome in order to move on to the next one:
- growth and development of at least one follicle must begin
- follicles must grow to the required size (mature)
- Premature ovulation should not occur before follicle puncture
- During puncture, the eggs must be successfully retrieved from the follicles
- sperm must fertilize at least one egg
- the fertilized egg must begin to divide and develop
- the embryo must be implanted in the uterus
In this chain, implantation still remains a mystery to scientists - why doesn’t every embryo become a child? Using modern technology, we are successfully able to obtain embryos in the laboratory, but we still cannot control the implantation process. We don't know which embryo will become a baby, and this brings a lot of frustration for both the doctor and the patient.
Implantation is a very complex process. First of all, the embryo must continue to develop to the blastocyst stage and then emerge from its shell (zona pellucida). The hatched blastocyst must then implant into the endometrium of the uterus in a short period of time called the implantation window. The three main phases of implantation are known as opposition, adhesion and invasion. Opposition, or orientation of the embryo in the uterine cavity, begins at the moment when the uterine cavity is maximally reduced due to the absorption of the fluid in it by pinopodia (small tuberculate structures that appear on the outer membrane of the cells lining the uterus).
Blastocyst adhesion is a chain of biochemical reactions leading to its attachment to the endometrium. Many molecules such as cytokines, growth factors and integrins play an important role in this complex process during which the blastocyst and the maternal endometrium enter into a subtle dialogue. Invasion is a self-controlled process that allows the embryonic trophoblast (blastocyst cells that will later become placental cells) to penetrate deep into the decidual maternal tissue (endometrial cells that later form the maternal part of the placenta) and invade the endometrial bloodstream. This occurs through the production of special chemicals called proteinases. For successful implantation of the blastocyst, immune mechanisms are also very important, ensuring dialogue between the tissues of the mother and the embryo, which are genetically and immunologically different. Activated cells of decidual tissue and trophoblast cells produce a large amount of immunologically active substances that cause the necessary immune reactions.
How implantation is regulated and occurs remains a mystery, but it is worth noting that in humans the implantation process is surprisingly low in efficiency - nature is not always competent! An absolutely healthy married couple has only a 20-25% chance of conceiving a child in each menstrual cycle. Responsibility for such low efficiency lies both with the embryo itself and with disturbances in the embryo-edometrial dialogue.
Today we know that one of the main reasons for unsuccessful implantation is genetic pathologies of the embryo. Fundamental research in the field of implantation is of great interest, since, apparently, implantation is the main factor limiting the effectiveness of ART.
However, we still have a lot to learn before we can really control this process.
Analysis of a failed IVF cycle
If you don't get pregnant after your first IVF attempt, of course you will be very upset and disappointed. However, remember that this is not the end of the journey - it is just the beginning. After an unsuccessful IVF cycle, you will meet with your doctor and analyze what conclusions can be drawn. When analyzing an unsuccessful IVF attempt, the doctor pays special attention to important points that affect the success of treatment:
- Was your body optimally prepared for pregnancy? Of course, the fact of the presence of certain general and gynecological diseases does not always affect the onset of pregnancy, but on the other hand, a decrease in the ability to conceive in many diseases (somatic diseases, endometriosis, uterine fibroids, hydrosalpinx, etc.) cannot be ruled out. Therefore, it is necessary to prepare the body for conception and conduct IVF during a period outside of the exacerbation of any chronic diseases. An additional examination will probably be ordered to identify possible pathology.
- Was the ovarian response to stimulation good enough? Were the eggs of good quality? The optimal ovarian response to stimulation is considered to be the production of 5 to 15 eggs.
- How did fertilization go, how many eggs were fertilized and how?
- Were the resulting embryos of good quality and did they develop normally in the laboratory?
- Was the structure of the uterus and endometrium optimal?
- Has implantation occurred, as determined by a blood test for the hCG hormone two weeks after embryo transfer?
- Why didn’t pregnancy occur (although there is no answer to this question!)?
- Do I need to do any additional testing before my next IVF attempt?
- Do I need to do any treatment before my next IVF cycle?
- Can the same treatment regimen be repeated or does it need to be modified before trying again?
When can I start a repeat IVF cycle?
Even if you don't get pregnant, you shouldn't give up. Today, IVF is the most modern method of overcoming infertility, the latest technologies that modern medicine can offer (although this method is far from ideal, no one has yet come up with a better one in the world). And even if it doesn’t work out on the first try, success is possible with repeated attempts.
Repeated IVF cycle
Most doctors advise waiting at least one month before starting the next treatment cycle. Although it is medically possible to repeat the IVF cycle as early as next month, most patients need a break to gather their strength and regain their peace of mind before starting all over again. Typically, we recommend a two-month break before trying IVF again.
According to our observations, repeated IVF programs produce results in a higher percentage of cases. There are many reasons for this. The doctor already knows how the female body reacted to hormonal stimulation. Depending on the results of the previous cycle, the doctor may change the treatment regimen. For example, if the ovarian response to stimulation was insufficient, the doctor may increase the dose of the drug to stimulate superovulation or change the stimulation protocol. If fertilization does not occur, you may need ICSI. If the quality of the eggs was poor, the doctor may recommend the use of donor eggs. However, if the results of the previous cycle were satisfactory, the doctor may recommend repeating the same treatment regimen: all that many patients need to succeed in an IVF cycle is time and one more try.
It is interesting to note that couples undergoing a repeat IVF cycle are usually much calmer and their body responds better to taking hormonal medications. This may be due to the fact that they are already aware of all the necessary medical procedures and are better prepared for them. A psychological attitude, positive thinking, and belief in success really increase the chances of getting pregnant.
Other articles
June 26, 2009
Recommendations after IVF
Recommendations for lifestyle and nutrition after IVF
August 16, 2018
Scientific publications of specialists from the Embryo Center
List of major scientific publications by employees of the Embryo Center for Assisted Reproduction
July 12, 2019
Age-related infertility
Separately, we can highlight another factor of infertility - AGE.
A dangerous demographic trend has developed in European countries. Multiple methods of birth control, contraceptives, urbanization, plus our social activity lead to the fact that people are now getting married later and thinking about having children later. First education, career, and then children. And all this makes a woman hesitate to conceive a child.
© 2001 - 2021 "Embryo", ODO Belivpul. All rights reserved. Use of materials and photographs from the site is possible only with the permission of the copyright holder.
Services of artificial insemination, treatment of male and female infertility, endoscopic surgery, gynecology and family reproduction planning.
Idea, design and development of the ActiveMedia website
The essence of the method
In Vitro Fertilization
is a method of overcoming infertility in which the egg is fertilized by sperm outside the female body and transferred to the uterus after confirmation of fertilization.
IVF is carried out in several stages. First, ovulation and egg growth are stimulated using hormonal therapy, then they are collected, fertilized in a nutrient medium, and subsequently transferred to the uterine cavity. In case of infertility complicated by the pathological condition of the father's sperm or difficulties in the maturation of eggs, additional methods of reproductive technologies are used - ICSI, PIXI, laser hatching, cryoprotocol, etc. Are additional methods needed, or is classical IVF sufficient? Your personal reproductive specialist will find out all this during preliminary examination.
Further, pregnancy develops in the same way as during natural conception; the course of labor depends only on the characteristics of the pregnancy and the mother’s body.
Possible complications after the procedure
The hope for successful IVF after laparoscopy may not be realized for several months after the minimally invasive intervention. Despite the fact that for most patients the likelihood of becoming pregnant after the intervention increases by 1.5-2 times, some women still experience difficulties conceiving, since the causes of infertility have not been completely eliminated. The share of such unsuccessful operations is low - about 1%.
Unfortunately, doctors do not exclude the risk of complications, including those that arise as a result of the use of anesthesia or medical procedures. They are divided into three groups:
- Arising during the intervention. These include perforation of organs and bleeding. These problems are eliminated as part of the operation or require more serious interventions, for example, abdominal surgery (laparotomy). In the latter case, artificial conception is postponed to a later date (usually 9-12 months) until the walls of the organs are completely restored.
- Occurring on the first day after the procedure. These include bleeding, infection of the reproductive organs, and vascular thrombosis in the surgical field. If the doctor detects the presence of inflammatory processes, the woman is prescribed a course of antibiotics and physical therapy. In addition, many women experience digestive problems on the first day after surgery, which can be eliminated by following a diet and moderate physical activity.
- Distant, occurring several weeks after the intervention. These include the formation of adhesions of the wall of the uterus and fallopian tubes. Such consequences are typical for the removal of extensive foci of endometriosis inside the uterus, as a result of which large growths form on its walls, or they fuse together. Such pathologies are eliminated through repeated intervention.
Despite the abundance of possible problems, laparoscopy before IVF ends with them only in 2-5% of cases. Careful preparation for surgery and compliance with all, even minor, rules during recovery after the intervention help reduce the risk of their occurrence.
Contraindications to IVF
In addition to the indications for performing the procedure, there are also certain contraindications. Therefore, whether to do IVF or not should be decided in each specific case only by the attending physician. Before treatment, the woman undergoes a thorough examination to identify possible contraindications.
Main contraindications:
- Somatic pathology in which pregnancy is impossible.
- Psychical deviations.
- Developmental anomalies or acquired deformities of the uterus, in which implantation of embryos is problematic.
- Malignant or benign neoplasms of the uterus and appendages, which exclude hormonal preparation.
- Cancerous tumors of any location.
- Active inflammatory diseases of the reproductive system in men and women.
In any case, the issue of treatment for each specific couple is considered individually.