- Form
- Size
- Circuit
- Structure
- How the results are deciphered
The digestive system includes an organ called the pancreas. It promotes the digestion of food. This means fatty, carbohydrate, protein foods. Thanks to this organ, carbohydrate metabolism in the body is regulated. With the development of various pathological processes or diseases, the risk of serious consequences for the pancreas increases.
Where is the organ located and what parts does it consist of?
The gland is located in the area behind the peritoneum, to the left and slightly behind the stomach. It is protected by ribs and consists of a head, tail and body, so scanning of the sections occurs from different points. At the heart of the organ are small lobules that produce digestive enzymes and pancreatic islets that release humoral substances into the blood. Pancreatic juice, which serves as an enzyme, enters the duodenum and takes part in the digestion process.
Preparatory activities
The scan should be done on an empty stomach. To do this, the patient must fulfill several requirements:
• 24 hours before the procedure, exclude “heavy foods” from the diet.
• Dinner should be no later than 18:00.
• To relieve bloating and reduce gas formation, you can take Espumisan.
You need to bring a diaper and a towel to the ultrasound scan. During the examination, the patient lies on the couch. The ideal option would be to perform an ultrasound in the morning. In some cases, the patient will need to drink water before the procedure.
When should you do an ultrasound of the pancreas?
The doctor may prescribe an ultrasound of the pancreas and other abdominal organs in the following cases:
- long-term pain in the epigastrium;
- recurrence of pain;
- painful reaction when palpating this area;
- presence of palpable formations;
- identification of possible complications of previously diagnosed chronic or acute pancreatitis;
- assumption of the presence of an abscess, hematoma, stone, cyst or tumor of the pancreas;
- newly diagnosed diabetes mellitus;
- additional examination after deformation of the posterior wall of the stomach detected by gastroscopy;
- detection of changes in the shape of the duodenum during X-ray examination.
This examination can be prescribed to adults and children both for emergency reasons and on a routine basis. Modern equipment makes it possible to conduct research at the patient’s bedside.
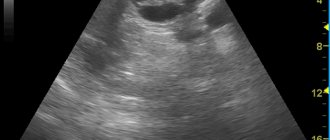
The essence of the study
The essence of the method is the registration of waves (echoes) reflected from organs by a sensor. Fabrics with different densities reflect them differently. The information is displayed on the screen in the form of a picture, where areas with higher density appear lighter.
The examination is carried out with the patient lying on his back, the examination begins with the identification of large vessels located in the abdominal cavity - this serves as a guide to determine the position of the gland. The position of the gland relative to the spine is also determined.
The main part of the study is carried out at maximum inspiration.
It may be necessary to examine in other projections, in the position on the left and right side, as well as in an upright position.
The examination is completely safe and painless.
During the examination, the ultrasound specialist fills out a standard protocol form, which indicates the size of the gland and its parts, density, uniformity of structure, clarity of the contours of the organ and ducts, and the presence of areas with altered density. If necessary, photographs can be attached to the protocol.
How is the research going?
First, the patient lies on his back, then he turns on his left side. In this position, the tail of the gland is scanned. After this, he turns on his right side. To examine the condition of the head and body of the gland, the doctor asks the patient to take a semi-sitting position.
As landmarks for detecting the pancreas, the sonologist uses the aorta with the inferior vena cava, superior and inferior mesenteric arteries, etc. There is a special program to determine the size of the organ. Even if all the indicators do not deviate from the norm, the doctor provides a detailed breakdown of the data in the conclusion.
The density of pancreatic tissue (echogenicity) depends on the age and body weight of the patient. Over the years, it decreases and acquires signs of hyperechogenicity. Normally, the structure of the gland is homogeneous. Proper preparation facilitates good viewing of all parts of the organ during the examination.
Form
During an ultrasound examination, the shape and deviation from the norm are determined. If there are no problems, the organ will have an S shape. In some situations, it is possible to identify pathology that is expressed in a disturbed form. The organ can be ring-shaped, spiral, split, or additional in shape. The anomaly detected by ultrasound is an isolated pancreatic defect or part of a severe pathological process.
In most cases, ultrasound can reveal only indirect symptoms. We are talking about a narrowing or additional duct. In such a situation, the doctor may prescribe another study to exclude or confirm the deviation.
Pathological changes
- An abscess (abscess) of the pancreas looks like a pocket or bag filled with sequesters and heterogeneous fluid. As the patient's body position changes, the level of fullness changes.
- Acute or chronic pancreatitis, causing changes in the structure of a diffuse or focal nature. At the same time, the tissue density is reduced, the contours of the organ are not clear. The size of the gland and its ducts is higher than normal. Based on these changes, the doctor diagnoses pancreatitis.
- The appearance of necrotic foci and cysts further provokes the complete melting of pancreatic tissue (pancreatic necrosis). This appears as poorly structured hypoechoic areas.
- One of the consequences of pancreatic necrosis is the formation of many purulent abscesses, which, merging, form large areas of pus and sequestration.
- False cystic formations on the screen look like anechoic cavities filled with fluid.
- Tumors on ultrasound look like round or oval formations of low density and heterogeneous structure, abundantly covered with a network of blood vessels. If cancer is suspected, all parts of the gland must be examined very carefully. If the focus of a malignant tumor is in the head, then the sign will be jaundice. Ultrasound data also allows you to diagnose the type of cancer.
Decoding
The essence of the pancreas ultrasound procedure is that the dense organ reflects ultrasound waves, which are converted into electrical impulses - the doctor sees the image on the computer screen. It is by this that he judges the structure and functioning of the digestive structure.
Ultrasound of the pancreas allows you to evaluate the following parameters:
- size - when they increase, an acute inflammatory process can be assumed, while when they decrease, a chronic course of pancreatitis can be assumed;
- shape and contours - clear delineation and smooth transition from the body of the organ to its tail and head, without jaggedness or discontinuity;
- structure – dense, homogeneous;
- echogenicity - reflection of ultrasonic waves, similar to that of the liver;
- structure of ducts - diameter, expansions, additional inclusions;
- the location of the organ relative to large vessels, as well as the spine.
All of the above parameters allow the doctor, who evaluates the ultrasound results, to get a complete picture of the condition and functioning of the pancreas.

Indications for ultrasound
Ultrasound examination of the pancreas is usually included in a comprehensive examination of all abdominal organs. After all, it is closely related to the functions of other internal organs, mainly the liver. The indication for research is any pathological condition of the digestive system. Many diseases can occur with hidden or completely erased clinical signs. Therefore, once a year it is necessary to conduct an ultrasound examination of the abdominal cavity for the early detection of many diseases.

The most common conditions for which an ultrasound is recommended:
- prolonged or periodic pain, discomfort in the upper abdomen or left hypochondrium;
- tension in the anterior abdominal wall or local pain in the epigastric region, which was detected by palpation;
- frequent bloating (flatulence), nausea and vomiting that does not provide relief;
- diarrhea (stool disorders), constipation, detection of undigested parts of food in the stool;
- presence of low-grade fever for a long time;
- when observing the patient's yellowness of the skin and mucous membranes, deviations of laboratory parameters from the norm;
- with a sharp increase in blood sugar levels and an unreasonable decrease in body weight;
- after an x-ray of the abdominal organs has been performed and changes in size, shape, structure, distortion of contours have been identified, and pneumatosis of the pancreas has been detected;
- if you suspect the presence of a cyst, tumor, hematoma, stones, or abscess in the gland.
Mandatory use for abdominal injuries and elective surgeries is indicated.
How to prepare for an ultrasound examination?
A routine ultrasound examination of the abdominal organs must be carried out on an empty stomach, the stomach must be empty. Otherwise, the reliability of the study is significantly reduced.
Imaging accuracy may be affected by increased gas production in the intestines. It needs to be minimized and intestinal motility improved.
Therefore, on the eve of a scheduled ultrasound, a gentle diet is recommended for 2-3 days, avoiding legumes, black bread, cabbage, carbonated drinks, and sweets. The last meal should be no later than 19 hours before the test day.
Preparation for an ultrasound of the pancreas and neighboring organs may include taking activated charcoal, laxatives, enzymes and drugs that reduce gas formation.
In emergency cases, ultrasound can be performed without preparation.
Interpretation of ultrasound of the pancreas
In the case of normal indicators, no questions arise. If the laboratory parameters are also without deviations, we can talk about the correct functioning of the pancreas.
A diagnostic sign of acute pancreatitis is an increase in size and a decrease in the echo density of the gland due to edema.
In the case of chronic pancreatitis and cancer, echo density is increased as a result of replacement of glandular tissue with fibrous or tumor tissue. Also, in these conditions, an increase in the size of the entire gland or its individual parts is detected.
The expansion of the Wirsung duct, as well as the lack of its response to the introduction of secretin, also signals an inflammatory process.
In cases of impaired blood supply and atrophy, a decrease in the size of the gland is noted.
With pancreatic cancer, there may be an increase in individual segments, uneven structure, uneven contours, as well as depressions on the surface of the liver, compression or displacement of the aorta and inferior vena cava.
If a tumor is not visible, the doctor can assume its presence by the deviation of the tail of the gland.
The presence of fluid in cysts is determined by the observed changes in formation at different body positions.
Ultrasound visualizes areas of necrosis, abscess, and blockage of ducts with stones.
Neighboring organs must be examined - liver, spleen, duodenum, duct and vascular system. The presence of a pathological process in any of them can be the cause or consequence of pancreatic disease.
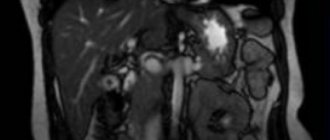
Normal size of the pancreas on MRI
Organ parameters are variable:
| Department | Dimensions (mm) |
| Head | 11- 35 |
| Body | 4- 30 |
| Tail | 7- 30 |
The concept of normal on magnetic resonance images is relative. Sizes depend on gender, height, age, food load. A slight deviation from generally accepted indicators, provided the structure of the organ parenchyma is normal and functions are intact, is not considered a pathology. The length of the pancreas is 15-23 cm, width 4.5-6 cm, weight about 70-80 grams.
Normally, the organ is not enlarged, the contours are clear, even, and the dimensions correspond to the person’s build. The pancreatic duct is not dilated, the surrounding tissue is without any features. No changes in the MR signal were detected.