“The results of an ultrasound of the mammary glands revealed a formation suspicious for oncology,” “the results of mammography do not clearly exclude the presence of a malignant formation,” “a biopsy showed the presence of cancerous changes in the mammary gland and an extensive examination is required.” These are just a few of the worst words a woman can hear from her doctor.
The mammary glands consist of three main types of tissue - adipose, connective and glandular. Breast cancer (BC) is a malignant tumor of the mammary gland that develops from glandular tissue cells. Contrary to popular belief, breast cancer affects both women and men, but it is approximately 100 times more common in women.
- How does breast cancer occur?
- Types of Breast Cancer
- Causes and risk factors
- Symptoms
- Self-diagnosis
- Diagnosis by an oncologist-mammologist
- Stages of breast cancer
- Breast cancer treatment
- Prognosis for breast cancer
How does breast cancer occur?
Breast cancer develops in the same way as any other malignant tumor. One or more cells of glandular tissue, as a result of a mutation that has occurred in them, begin to divide abnormally quickly. They form a tumor that can grow into neighboring tissues and create secondary tumor foci - metastases.
Mutations that lead to breast cancer can be hereditary or acquired.
Common hereditary genetic causes are mutations in the BRCA1 and BRCA2 genes. BRCA1 mutation carriers have a 55–65% risk of developing breast cancer, and BRCA2 carriers have a 45% risk of developing breast cancer. Such genetic defects are inherited from parents to children and cause cancer in approximately 15% of cases.
Much more often, breast cancer occurs due to acquired mutations: they arise in the cells of the gland and are not inherited. For example, in 20% of cases, the number of copies of the gene encoding HER2, a receptor protein that is located on the surface of cells and stimulates their reproduction, is increased.
The “molecular genetic portrait” of a breast tumor is important when choosing the optimal treatment.
Can mammography cause cancer?
There is no evidence that x-rays or any other diagnostic method can cause or provoke cancer.
The stress that accompanies an x-ray examination does not pose a danger, and some types of x-rays are even included in the list of preventive methods. These include fluorography and mammography. Instead of being afraid of the research method, it is better to pay attention to the qualifications and experience of the doctor who will be entrusted with the description of the images. If a mammogram has already been described, but there is no confidence in the professionalism of the specialist, or there are doubts about the diagnosis, contact the Honest Medicine company for a second opinion from a mammologist-radiologist. Other articles from the section “Mammography: normal, cyst, cancer, mastopathy in pictures”
Types of Breast Cancer
Types of breast cancer are divided into two groups: ductal and glandular. Ductal cancer is more common. It can be intraepithelial (in situ) and invasive. Intracellular ductal breast cancer has a more favorable prognosis, it rarely metastasizes and is curable in 98% of cases. The invasive version of the tumor is prone to uncontrolled growth and generalization of the process.
Glandular cancer can be lobular (invasive lobular carcinoma) or grow from other cells of the glandular tissue. Lobular cancer is often characterized by multicentric growth. The rate of increase in size and timing of metastasis of forms of nodular breast cancer depend on the degree of differentiation of the breast tumor.
Ultrasound examination of the mammary glands
✅ Advantages
suitable for women of any age,
suitable for women with dense breasts,
suitable for pregnant women,
does not require special preparation and injections of contrast agents,
does not use x-rays.
❌ Flaws
can't take a picture of the whole breast,
does not recognize microcalcifications,
may not see deep structures in case of large breasts,
the results strongly depend on the professionalism of the doctor,
The ultrasound conclusion cannot be rechecked without a repeat examination.
Ultrasound requires a highly qualified specialist who will conduct the study and interpret the result. This is due to the nature of the study. If we draw an analogy with a laser and a flashlight, then an ultrasonic sensor is a laser. The sensor scans tissue in a narrowly targeted area; an inexperienced doctor may not cover the entire volume of the breast and miss tumors.
The result of an ultrasound depends on the ultrasound machine the doctor uses. The higher the class of equipment, the higher the accuracy and resolution of the sensor, the more auxiliary automatic functions it has.
Evgenia Piloyan, oncologist-mammologist, microsurgeon
The presence of elastography is an easy way to distinguish a top-level ultrasound device. Elastography allows you to calculate tissue density, which helps assess the nature of the tumor.
At the Mammology Center, doctors work on an expert-level ultrasound machine GE LOGIQ S7 XDClear.

General Electric LOGIQ line of ultrasound devices
Causes and risk factors
Unfortunately, scientists do not yet have complete information about the causes of breast cancer. There is a list of risk factors that affect the likelihood of cancer, but some people are diagnosed with the disease in the absence of these factors, while others remain healthy even if many of them are present. Nevertheless, scientists still associate the occurrence of malignant breast tumors with certain circumstances that most often precede its appearance. These include:
- Age. The majority of breast cancer cases occur in women aged 55 years and older.
- Heredity. If breast cancer is diagnosed in one of your close relatives, the risk doubles.
- History of breast cancer.
- Increased breast tissue density as determined by mammography.
- Some benign neoplasms in the mammary gland.
- Early onset of menstruation - before 12 years of age.
- Late menopause - after 55 years.
- Lack of children or late (after 35 years) first birth.
- Exposure to radiation, such as from radiation therapy given to treat another type of cancer.
- Smoking and drinking alcohol. If a woman consumes 28–42 g of ethyl alcohol daily, her risks increase by 20%.
- Excess weight and low physical activity.
- Use of hormonal drugs: oral contraceptives, hormone replacement therapy in postmenopause.
- Breast injuries.
- Diabetes.
- Work on a schedule with night shifts.

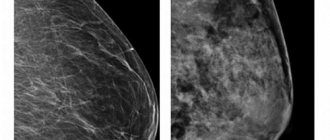
Digital mammography
Mammography is an examination of the breast using x-rays. A photograph of each breast is taken in two planes.
Mammography in our center
✅ Advantages
takes a picture of the entire breast in two planes,
microcalcifications are visible on the photographs,
does not require special preparation and injections of contrast agents,
one study can be analyzed by several specialists,
lends itself well to analysis by artificial intelligence.
❌ Flaws
not suitable for women with dense breasts,
not suitable for pregnant women.
Lesnyakov Anton, head of the Mammology Center
We are participating in clinical trials of artificial intelligence for mammogram analysis. The neural network double-checks the radiologists’ report, identifies missed tumors and marks all suspicious areas for further study.
Patients often ask about the dangers of X-ray radiation. On average, the radiation dose received during mammography is 0.3 millisievert (mSv). For comparison:
- during the year in the city a person receives 6 mSv,
- during an hour of flight on an airplane, a person receives 0.1 mSv,
- If the dose received during the year exceeds 50 mSv, the likelihood of developing cancer increases sharply.
A 2021 study published in the Annals of Internal Medicine found that only 0.125% of patients undergoing mammography each year develop cancer caused by the mammograph's X-ray radiation.
Symptoms
In the early stages, breast cancer usually does not manifest itself in any way. Most often, the tumor is discovered by the patients themselves or is detected accidentally during preventive studies.
Patients usually complain of the presence of a palpable formation and discharge from the nipple. Pain is a rare symptom of breast cancer, but pain syndrome can come to the fore at the stage of generalization of the process, especially when metastases spread to the bones.
Quite often, signs of breast cancer are detected, such as the appearance of asymmetry due to changes in the size of the affected gland. Reduction, upward displacement, deformation and wrinkling of the mammary gland can be observed in the scirrhous (fibrous) form of breast cancer. On the contrary, the breast on the affected side becomes enlarged due to the rapid growth of the formation or due to edema, which forms due to impaired lymph outflow.
When the tumor spreads into the subcutaneous tissue, skin changes may be observed. In this case, the following symptoms are revealed:
- “Platform” - the skin above the tumor becomes flattened; it is impossible to form a skin fold in this area.
- “Umbilization” - the skin of the mammary gland over the site of the lesion is wrinkled and retracted.
- “Lemon peel” is a characteristic appearance of the mammary gland due to lymphostasis.
Sometimes, when cancer spreads to the surface of the skin, signs such as redness and ulceration may be observed. The presence of these symptoms indicates that the process is neglected.
Changes in the nipple can also be detected, but only in the later stages. In this case, symptoms such as:
- Forga's sign - on the affected side the nipple is higher than on the healthy breast.
- Krause's sign - the nipple is thickened, the folds of the areola are noticeably pronounced.
Pathological discharge is a rather rare symptom, but in some cases it may be the only one detected during examination. The discharge is often bloody in nature, serous and purulent are less common.
Depending on the manifestations of the disease, different clinical forms of breast cancer are distinguished. In 75–80% of cases, the nodular form occurs. In the early stages, the only symptom is usually a painless lump in the breast. If you divide the breast into four parts by horizontal and vertical lines, then in half of the cases the tumor will be located in the upper outer part.
There are special forms of breast cancer with typical symptoms. These include:
- An edematous-infiltrative form, which is characterized by enlargement and swelling of the mammary gland, marbled skin color, and severe hyperemia.
- Mastitis-like is manifested by thickening of the affected mammary gland, increased body temperature.
- An erysipelas-like form, in which lesions are detected on the skin (sometimes ulcerations appear) that externally resemble erysipelas.
- The armored form is characterized by the presence of multiple nodes, due to which wrinkling and deformation of the mammary gland occurs.
- Paget's cancer affects the nipple and areola. It is characterized by thickening of the nipple, changes in the skin in the form of redness and thickening, and the formation of crusts and scales.
Breast cancer - types
According to the World Health Organization, breast tumors are divided into two groups:
- non-invasive breast cancer, i.e. carcinoma in situ (without basement membrane perforation);
- invasive breast cancer (the tumor has penetrated the basement membrane).
Non-invasive breast cancer - carcinoma in situ
Non-invasive breast cancer is also called carcinoma in situ and, unlike invasive cancer, does not penetrate the basement membrane of the epithelium (it remains localized and does not spread through the breast stroma).
Ductal carcinoma in situ arises from the epithelial cells of the milk duct and is the most common form of preinvasive breast cancer (80%), and in 10-20% of patients the changes are bilateral. This form of cancer most often occurs in women between 40 and 60 years of age.
In most women, small tumors do not cause visible changes and are not felt when examining the breast (no lump). They are usually discovered incidentally, on mammography or breast biopsy, when fibrocystic changes are suspected.
If the diagnosis is made early and the tumor is surgically removed, the prognosis for recovery is good. If no tumor is found, it is expected that half of women will develop invasive cancer (which penetrates the basement membrane).
Lobular carcinoma in situ
Lobular carcinoma in situ is a rare malignant tumor that is usually diagnosed incidentally during a breast biopsy performed for some other reason.
Lobular carcinoma in situ accounts for about 20% of preinvasive cancers or 3-5% of all breast cancers. This tumor occurs in younger women (breast cancer in young girls).
This tumor is not detected during a breast exam (there is no lump in the breast) and is usually not visible on a mammogram. The diagnosis is made solely on the basis of a breast biopsy.
Invasive breast cancer
Invasive breast cancer can arise from the epithelium of the tubules or lobules and is of two types:
- ductal;
- lobular.
Most cancers are of ductal origin (about 80%), so the term "invasive breast cancer" has become synonymous with this form of cancer. In 10% of cases it is lobular invasive cancer.
Ductal invasive breast cancer
Ductal invasive breast cancer arises from the epithelium of the excretory ducts. At an early stage, it manifests itself in the form of a compaction because it causes a strong reaction of the connective tissue, as the tumor penetrates into it through the basement membrane. The size of the growths varies, but on average most are diagnosed when they are about 2 cm in diameter.
Most of these tumors are diagnosed during a breast exam or mammogram. In advanced cases, they stick to the front wall of the chest and retract the skin or nipple.
Lobular invasive breast cancer
This tumor is formed by a malignant change of lobular carcinoma in situ. The increase in the number of newly diagnosed women over 50 years of age with this breast cancer is due to an increase in the number of women using hormone replacement therapy.
Most patients experience a lump in the breast, although in some the tumor does not interact with the connective tissue and no noticeable mass is palpable. This breast cancer tends to occur bilaterally (on both breasts).
The remaining 10% of malignant tumors are rare, special forms of breast cancer:
- Paget's disease of the breast
(Paget's disease of the nipple, Paget's cancer) - eczema on the nipple of the breast, redness of the nipple with itching of the nipple and retraction of the nipple. This condition resembles dermatitis, but due to the appearance of the nipple, we almost always find ductal carcinoma in the affected breast. - Medullary breast cancer
is a well-confined tumor and has a slightly better prognosis than invasive breast cancer. - Mucinous breast cancer
is a slow-growing tumor, usually found in older women (average age about 60 years), the prognosis is good, and it rarely metastasizes to the axillary lymph nodes. - Tubular breast cancer
is a rare form of invasive breast cancer with a very good prognosis; the tumor is usually small and rarely metastasizes to the axillary lymph nodes. Relapse of the disease is rare. - Invasive papillary breast cancer
- less than 1% of all breast tumors, often manifests as bleeding from the nipple and in this respect resembles benign papillomas. - Inflammatory breast cancer
is a rare type of breast cancer that causes inflammation of the entire breast (mastitis) and enlargement, often without a breast lump. Redness on the chest, chest pain and swollen breasts are visible. This form of cancer is extremely aggressive.
Breast cancer - symptoms
Breast cancer is a slow-growing tumor. It is believed that on average it takes 7 to 8 years for a 1 cm tumor to grow from the first malignant cell.
The most common symptom of breast cancer is a palpable, painless nodule in the breast (70-80%). Other symptoms include skin changes (wrinkled skin like an orange peel), bloody brown breast discharge (2-3%), breast pain (5%). Much less often, enlarged axillary lymph nodes or signs of distant metastases appear as the first symptom.
In Western countries, an increasing number of breast tumors are being detected in asymptomatic patients (women who do not have symptoms) using screening mammography. There is ample evidence that early treatment after screening mammography reduces mortality and improves survival by 30-40%.
Unfortunately, in 70% of cases, breast cancer is detected by the patient herself. Then the disease is often in an advanced stage.
There are some common clinical features for all histological types of breast cancer:
- Palpable lump (breast lump)
– A lump can be felt during a breast self-exam or during a routine physical examination. - Skin changes
– due to the reaction of the tumor with the connective tissue, the skin may retract. The growth of the tumor causes the lymphatic vessels to close and the skin to swell, causing the skin to appear wrinkled and thickened (orange skin). If the tumor affects the main duct, the nipple may become retracted. Some tumors can affect most of the lymphatic vessels of the breast, especially under the skin, and cause swelling, redness and tenderness of the breast, which we call inflammatory breast cancer. - Enlarged lymph nodes
– tumors spread by lymphatic route to regional lymph nodes, and which group of lymph nodes they will spread to depends on the location of the tumor. Most tumors spread to the axillary lymph nodes (axillary lymph nodes), some spread to the lymph nodes along the internal mammary artery, and some spread to the supraclavicular lymph nodes (lymph nodes above the collarbone). Lymph node involvement is one of the most important prognostic factors and predicts a worse prognosis in patients with breast cancer. - Distant metastases
- in addition to the lymphatic system, the tumor can spread through the blood (hematogenously) and give distant metastases. Breast cancer most often metastasizes to the lungs, liver, bones, brain and adrenal glands.
Self-diagnosis
It is worth checking the mammary gland yourself for the presence of nodules or any other changes once a month after menstruation. It is more convenient to carry out home diagnostics while taking a bath or while under the shower. You should tell your doctor about any changes that are discovered as soon as possible.
Procedure for performing breast self-examination:
- Undress from the waist up and stand in front of a mirror.
- Raise your hands up and place them behind your head. Carefully examine the mammary glands. Turn right, left side.
- Feel the mammary glands while standing with your index, middle and ring fingers folded together. Start at the upper outer part of the chest and move clockwise.
- Pinch the nipple with two fingers. Check to see if anything stands out.
- Feel the mammary glands again - now in a lying position.
70% of breast cancer cases are self-diagnosed by patients through breast self-examination.
Diagnosis by an oncologist-mammologist
History taking
Diagnosing breast cancer begins with a conversation. At this stage, it is important for the doctor to evaluate the complaints and find out whether cases of breast cancer have occurred in the family, and if so, how often. This helps to suspect a hereditary form of the disease associated with mutations in the BRCA1, BRCA2, NBS1, CHECK, TP53 genes.
Breast examination
Next, the doctor examines, palpates the mammary glands, checks to see if there are any nodes or lumps in them, or if the lymph nodes in the axillary, supraclavicular and subclavian areas are enlarged.
Instrumental diagnostics
After the examination, the doctor may refer the woman for a mammogram, an X-ray of the breast. Indications for this study include lumps in the mammary gland, changes in the skin, bleeding from the nipple, as well as any other symptoms that may indicate a malignant tumor. Ultrasound examination of the mammary glands is also used. Mammography and ultrasound are complementary methods, each of them has its own advantages:
| Mammography | Ultrasound of the mammary glands |
| Allows you to detect pathological changes in the mammary gland 1.5–2 years before the onset of symptoms. If there is bloody discharge from the nipple, ductography can be performed - X-ray with contrast of the milk ducts. This helps to obtain additional useful information. High sensitivity - accurate diagnosis of up to 90% of cases of breast tumors. Ability to detect microcalcifications up to 0.5 mm. | Safety - there is no effect on the body from x-rays. Well suited for high density breast tissue in young women (up to 35–45 years). Allows you to distinguish breast cysts (cavities with fluid) from solid tumors. Allows you to assess the condition of regional lymph nodes. Well suited for monitoring needle position during biopsy. |
Magnetic resonance imaging is a highly informative method for diagnosing malignant breast tumors. It is used for lobular cancer, when mammography and ultrasound are uninformative, as well as for assessing the size and location of the tumor, which helps determine the tactics of surgical treatment. MRI can be used to screen women who carry abnormal genes associated with an increased risk of breast cancer and have a strong family history.
The final diagnosis is determined by the results of a biopsy. You can obtain breast tumor tissue in different ways:
- Examination of nipple discharge - tumor cells may be found in it.
- In a fine-needle biopsy, a needle is inserted into the breast tumor under ultrasound or mammography guidance.
- During a trephine biopsy (CORE biopsy), a special instrument resembling a thick hollow needle is used. It allows you to obtain more breast tumor tissue and examine it in more detail.
- In a needle-gun biopsy, a needle is inserted into the exact location using a special gun.
- A stereotactic vacuum biopsy is almost as accurate as a breast cancer biopsy during surgery, but it can be performed under local anesthesia without the need for general anesthesia. The procedure is carried out using a Bard Magnum pistol and a vacuum apparatus.
- An excisional biopsy is performed during surgery. The entire tumor along with breast tissue is sent for examination.
- Sentinel biopsy is an examination of the sentinel lymph node during surgery. It helps determine whether the tumor has spread to regional lymph nodes and whether they should be removed.
Euroonco doctor S.M. Portnoy talks about the role of biopsy in diagnosing breast cancer:
Cytological and histological examinations are carried out in the laboratory, where the structure of individual cells and tissues is assessed. Molecular genetic studies are currently available: they help to identify mutations that caused malignant degeneration and to select optimal antitumor therapy.
A biopsy can determine whether a tumor is cancerous, as well as determine its type and stage. In addition, examination of the biopsy material provides an answer to the question of whether the tumor is hormone-dependent, which also affects the treatment regimen.
Assessing the extent of cancer spread in the body
Once cancer is diagnosed, it is important to determine its stage and understand how far it has spread. The following studies are used for this:
- Ultrasound and lymph node biopsy.
- Computed tomography and MRI - they help assess the size, location of the breast tumor, and lesions in other organs.
- Metastases in the liver are diagnosed using ultrasound.
- X-rays can help identify lesions in the lungs and bones.
- PET scanning is the modern “gold standard” for diagnosing metastases of malignant tumors.

Breast cancer - diagnosis
To diagnose cancer:
- An anamnesis is collected, and by interviewing the patient, the symptoms and duration of their action are found out. The doctor asks about the existence of possible risk factors, such as a family history of breast cancer, year of first and last menstruation, time of first birth and number of births, use of oral contraceptives or hormonal medications.
- The breast and lymph nodes (supraclavicular and axillary) are examined by inspection and palpation. During the examination, attention is paid to the size, shape and symmetry of the breasts, as well as possible changes in pigmentation, indentations in the skin or nipples. You should also pay attention to possible discharge from the nipple. Palpation determines the location of any changes, size, consistency (hard or soft), sensitivity, mobility to the surface and skin, as well as possible pain with suspicious changes in the breast.
- Mammography is an x-ray diagnostic examination of the breast. It is still the most accurate and widely used non-invasive method. Mammography is used for early detection and confirmation of diagnosis. In addition, mammography identifies possible multicentric tumors and clusters of microcalcifications specific to breast cancer. Today it is recommended that a woman have her first mammogram at age 40 (with a positive family history at age 35). Then mammograms are done every two years.
- Breast ultrasound is very often used to diagnose cancer. It is less sensitive and specific than mammography, especially in postmenopausal women. This method is indicated for young women in whom glandular tissue predominates in the breast and is very helpful in distinguishing breast cysts from solid tumors. The results of breast ultrasound depend on the phase of the menstrual cycle.
- Any suspicious breast changes require a biopsy. A breast biopsy is the removal of a tissue sample for pathological analysis, which means viewing under a microscope. The pathohistological result is the only reliable evidence of a malignant disease, such as breast cancer.
- In addition to a breast biopsy, it is necessary to determine the involvement of the lymph node draining the breast area (sentinel node). Determination of lymph node involvement is necessary to assess the stage of the disease.
Stages of breast cancer
Staging for breast cancer is based on the generally accepted TNM system. The T in this abbreviation indicates the size of the primary tumor:
- Tis is a “cancer in situ” that resides in the cells lining the milk ducts or lobules and does not invade adjacent tissue. This may be lobular, ductal, or Paget's carcinoma.
- T1—tumor diameter in greatest dimension is less than 2 cm.
- T2 - 2–5 cm.
- T3 - more than 5 cm.
- T4 is a tumor that has grown into the chest wall, skin, or inflammatory cancer.
The letter N indicates the presence of metastases in regional lymph nodes. N0 - there are no foci in the lymph nodes. N1, N2 and N3 - damage to different numbers of lymph nodes.
The letter M indicates the presence of distant metastases. One of two numbers can be indicated next to it: M0 - no distant metastases, M1 - distant metastases present.
Depending on the values of T, N and M, there are five main stages of breast cancer (within some of them there are substages):
- Stage 0: cancer in situ.
- Stage I: tumor in the mammary gland up to 2 cm in diameter.
- Stage II: a tumor in the mammary gland with a diameter of up to 5 cm or more, there may be metastases in the axillary lymph nodes on the affected side.
- Stage III: a tumor in the mammary gland up to 5 cm or more, can grow into the chest wall or into the skin, there are foci in the regional lymph nodes.
- Stage IV: The tumor can be of any size, it does not matter whether regional lymph nodes are affected. If distant metastases are detected, stage IV cancer is always diagnosed.
Breast cancer classification parameters
The main elements of the breast are lobules with glands that produce mother's milk, as well as ducts that deliver it to the nipple. The tissues are penetrated by blood and lymphatic vessels responsible for supplying the mammary gland (MG) with nutrients and removing waste products. The disease begins when normal cells in a woman's body begin to divide uncontrollably, and the process of their death is disrupted. Types of breast cancer are classified according to different criteria.
Based on the location of the primary node, oncological pathologies are divided into neoplasms:
- pacifier;
- areolas;
- axillary area.
Depending on the quadrant of location, malignant nodes are:
- upper internal;
- upper-outer;
- lower internal;
- lower outer.
Up to 50% of primary tumors in women are formed in the upper outer quadrant of the mammary gland, about 20% - in the areola or central part of the breast.
Experts classify breast cancer of unspecified location and beyond the boundaries of individual regions into separate groups.
Tumor primary nodes can be ductal or lobular, based on the tissue of which element of the organ structure began to degenerate.
In addition to location, the classification of the disease according to parameters such as:
- histological structure;
- stage of development;
- form;
- molecular taxonomy.
Malignant neoplasms are also differentiated by the degree of aggressiveness of the impact and the speed of spread.
Metastasis
Regardless of the location of the primary node, cancer can be:
- non-invasive - the tumor grows, but does not leave the borders of the affected part of the organ;
- invasive - a malignant neoplasm grows beyond the boundaries of the lobule (or milk duct), its metastases first “capture” healthy parts of the breast, then other organs and systems.
Malignant cells “spread” throughout the body from the gland in two ways:
- lymphogenous - through lymphatic vessels;
- hematogenous - with the bloodstream.
First, metastases affect regional lymph nodes under the shoulder blades, armpits, sternum or collarbone area. Then they appear in distant areas of the lymphatic system, grow into the skin, soft and bone tissues.
At the terminal stage, malignant cells are found in almost all internal organs of the human body. Metastases from the primary node often spread hematogenously to:
- liver;
- brain;
- spine;
- pleura;
- lungs;
- ovaries;
- bones of the pelvis, hips.
When the development of breast cancer ends with the abnormal tissues being separated from the “maternal” node and transferred to other parts of the woman’s body, the disease is called metastatic.
If the primary pathogenic node forms again after treatment in the second mammary gland, in the same place, nearby tissues or organs, we are talking about a recurrent type of cancer.
Both forms of pathology are late-stage diseases; metastases can appear months or even years after the end of treatment. Relapse occurs in approximately 30% of women treated in the early stages of the disease. The average time for local “return” of oncology is five years. The risk of reappearance of the tumor is especially high in the first 24 months.
Non-invasive breast cancer can become invasive as the size of the tumor increases. It is very important to monitor the intensity of its growth, start treatment on time, and stop metastasis.
Experts distinguish three degrees of doubling in the size of carcinomas in women:
- high – the abnormal primary node grows twice in three months or less;
- average – doubles over a period of time from 3 to 12 months;
- low – doubling lasts more than a year.
Tumor cells undergo separate differentiation. In medical documents, the parameter is designated by the Latin letter “G”. Doctors distinguish three degrees of danger of breast cancer:
- highly differentiated (G1) - malignant cells are similar to natural ones, divide slowly, and have a low potential for metastasis;
- moderately differentiated (G2) - pathologically altered structures retain the characteristics of normal ones, multiply at an average speed, and are more prone to spread than the previous group;
- low-differentiated (G3) - cells are practically devoid of healthy signs, quickly divide, and have a high potential for the formation of metastases. They are a sign of cancer with an aggressive, rapid, life-threatening course.
Determining the type of malignant cells and the location of the primary tumor helps predict the possible spread of metastases.
Breast cancer treatment
The treatment regimen for breast cancer should be selected individually for each patient, taking into account factors such as tumor type, stage, and sensitivity of the tumor to hormonal therapy. The general condition of the patient is also taken into account. If the tumor is detected in the early stages and the correct management tactics are chosen, then the chance of completely curing breast cancer is very high.
Surgical method
The surgical method is the dominant one in the treatment of breast cancer. If the tumor is detected early, it is possible to perform an organ-preserving operation—sectoral resection. Performing such an intervention is accompanied by an increased risk of local recurrence, and therefore it is combined with other methods, for example, radiation therapy.
In later stages, breast cancer is treated with a mastectomy—removal of the entire breast along with nearby lymph nodes. The doctor may also decide to remove the second breast if there is a high risk of developing a malignant tumor in it.
A sentinel biopsy, or sentinel lymph node biopsy, may be performed to determine whether cancer cells have spread to the lymph nodes and to determine the extent of surgery . During surgery, a radiopharmaceutical or fluorescent dye is injected into the tumor to help visualize the lymph node that first receives lymph from the breast tissue. It is removed and histological examination is performed. If no tumor cells are found in the sentinel lymph node, you can limit yourself to removing the lesion in the mammary gland. Otherwise, excision of regional lymph nodes is indicated.

Radiation therapy
In order to improve the immediate and long-term results of surgery for breast cancer, radiation therapy is used as an auxiliary method. It can be used in the preoperative period to reduce the degree of malignancy of the breast tumor, damage and regression of micrometastases. However, more often radiation therapy is used after surgery, when it is necessary to destroy cancer cells that may have remained in the body.
Chemotherapy
To treat breast cancer, chemotherapy is used before or after surgery with the aim of complete cure, prolonging life and improving its quality, or to reduce the volume of surgery. Each chemotherapy drug only affects cells in a specific phase of the cell cycle. Therefore, the most effective prescription is polychemotherapy - a combination of several drugs that have different effectiveness and mechanism of action.
Euroonko clinics use the most modern, original European and American chemotherapy drugs for the treatment of breast cancer. We have the opportunity to create a “molecular fingerprint” of the tumor and, based on its analysis, select the most effective and safe combinations of drugs.
Drug therapy: hormonal and targeted drugs
A malignant breast tumor is recognized as hormone-sensitive if more than 10% of the cells in its composition have receptors for estrogen or progesterone. In this case, hormonal therapy is used. The more the tumor has hormonal receptors, the more effective such treatment will be.
This type of therapy includes several methods that stop the production of hormones and block their flow. Today, drugs from the group of non-steroidal antihormones are increasingly used, which affect only the breast tumor and do not affect the mechanisms of hormone formation throughout the body. Therapy with hormonal drugs is prescribed both in the postoperative period to reduce the risk of recurrence, and as an independent treatment for inoperable breast tumors to control their growth.
Targeted therapy is also used to treat breast cancer—drugs that target specific target molecules in tumor cells and have minimal effects on healthy cells in the body. Targeted therapy is used alone or in combination with other treatments.
Prognosis for breast cancer
If breast cancer is diagnosed in the early stages (0-I), the five-year survival rate approaches 100%. That is, we can say that it is possible to cure almost all patients. Further, depending on the stage, the prognosis for five-year survival worsens:
- At stage II - 93%.
- At stage III - 72%.
- At stage IV - 22%.
The combination of breast cancer treatment methods available to oncologists allows in most cases to achieve remission of the disease or, at a minimum, prolong life while maintaining its quality. The effectiveness of treatment in general directly depends on whether treatment was started in a timely manner.
The maximum effectiveness of antitumor treatment is achieved only if it is carried out in accordance with international protocols and takes into account the individual characteristics of each patient. This is exactly how Euroonco oncologists prescribe treatment.
| More information about breast cancer treatment at Euroonco: | |
| Surgeons-oncologists-mammologists | from 5100 rub. |
| Removal of a breast tumor | from 92,000 rub. |
| Emergency oncology care | from 11000 rub. |
Book a consultation 24 hours a day
+7+7+78
Breast cancer - incidence
Breast cancer is the most common malignant neoplasm in women (affects one in 100). It is rare in men.
In approximately 80% of new cases, the disease is detected at an early stage, and approximately 20% of patients have advanced disease with metastases at the time of diagnosis.
The incidence of breast cancer has been increasing in recent decades, while mortality in developed countries has been decreasing. This is facilitated by earlier detection of pathology and increased effectiveness of treatment.
It is believed that one in eight women is susceptible to breast cancer.
The disease is rare in women under 40 years of age, and in young girls it is less than 1%.