Ultrasound diagnostics is a highly accurate, painless and accessible method of studying the body in all respects, actively used in various fields of medicine. Ultrasound also occupies an important place in ophthalmological practice - it is one of the main tools that complements generally accepted methods for diagnosing eye pathologies.
Ultrasound research is based on the principle of echolocation. The eyeball is a set of environments with different acoustic impedances. By assessing the characteristics of the reflection of ultrasonic waves from various intraocular structures, it is possible to obtain information about their structure and determine normal and pathologically altered biological environments.
Ultrasound diagnostics allows for highly accurate measurements of the eyeball, obtaining information about the state of the anatomical and optical elements of the eye and assessing the nature of blood flow in the orbital vessels.
Possibilities of ultrasound diagnostics in ophthalmology
Ultrasound of the eye differs from other methods of ophthalmological diagnostics in its versatility - it is used to detect a wide range of eye diseases. Ultrasound allows you to assess both the general condition of the internal structures of the eye and measure its specific biometric parameters.
The main indications for an eye ultrasound are:
- closed eye injuries and damage to the optic nerve;
- progressive deterioration of vision;
- retinal disinsertion;
- pathology of the ciliary body;
- entry of foreign bodies into the eye (including those that are not detected by x-ray);
- clouding of optical media of various nature;
- suspicions of intraocular neoplasms, etc.
Ultrasound scanning is of particular value in the dynamic assessment of treatment results. It is used in calculating the optical power of artificial lenses, as well as for measuring and differentiating intraocular tumors. Ultrasound diagnostics is an indispensable tool in preparation for some ophthalmological operations.
How is the research going?
Each eye is examined separately in just one visit to the ophthalmologist. The patient only needs to place his chin on a special panel and fix his gaze on the luminous mark. The device scans all the necessary parameters and then produces printed results. It takes only 10 minutes to measure the radius of curvature of the cornea, the length of the eye axis, the diameter of the cornea and pupil and other parameters.
The measurement is carried out in a non-contact manner, so the patient does not experience pain or discomfort. He does not need to prepare for the procedure in any way; he just needs to make an appointment with an ophthalmologist. When measuring, there is no risk of infection, and the results are as accurate as possible, which greatly simplifies the selection of the most suitable artificial lens parameters.
Most often, the procedure is used when installing an artificial lens. This operation, in turn, is performed to treat cataracts and correct myopia and farsightedness. Given the large number of people suffering from these pathologies, biometrics is a fairly popular service.
Ultrasound eye diagnostic methods: scanning modes A and B
In ophthalmological practice, several ultrasound diagnostic methods (scanning modes) are used, each of them has its own technical features, differs in diagnostic capabilities and is intended for specific medical cases.
Ultrasound in A-mode . Scanning the eye in one-dimensional mode. The data on the monitor is displayed in the form of a graph, based on which the specialist assesses the biometric parameters of the eye. Ultrasound scanning in A-mode is classified into a separate direction - echobiometry.
Examination in A-mode allows you to accurately measure the axial length of the eye, the depth of its anterior chamber, and lens parameters. These data are crucial in preparing for cataract extraction, for accurately calculating the optical power of an artificial lens, and in diagnosing refractive errors. Ultrasound diagnostics in A-mode also makes it possible to detect and evaluate intraocular tumors.
Ultrasound in B-mode . Advanced scanning method. With its help, the monitor no longer produces a graph, but a two-dimensional image detailing the internal structures of the eyeball: lens, retina, eye muscles, etc. Research in B-mode allows highly accurate assessment and differentiation of intraocular changes: determining the nature of the pathology, its shape , length. Unlike the static A-mode, B-scan displays the intraocular picture in dynamics, which significantly expands its diagnostic potential.
Along with these two methods, which are considered to be the gold standard of ophthalmological diagnostics, other scanning modes are also used:
Combined method is a mode that combines the capabilities of A- and B-diagnostics.
Ultrasound biomicroscopy is an ultrasound method that allows high-resolution study of the structures of the anterior segment of the eye - we are talking about the cornea, iris, lens, and anterior chamber angle.
Three-dimensional echography is a highly informative method that provides three-dimensional acoustic visualization of intraocular structures. The image is given in volume. It is broadcast in real time, which allows you to assess the general condition of the eye over time.
Doppler ultrasound is a method that allows one to evaluate blood flow parameters in the orbital vessels.
Interpretation of indicators, normal indicators
After biometrics, the ophthalmologist receives data on the parameters of the eyeball. He compares them with normal values, determining the healthy or pathological condition of the eyes. Therefore, the following standards were identified:
- the length of the ocular axis of adult patients over 18 years of age is 23-24 mm;
- the length of the ocular axis in children under 4 years of age is 20-22 mm;
- the length of the ocular axis of patients from 4 to 18 years is 22-23 mm.
The identified deviations in the listed parameters indicate the development of the following pathologies:
- farsightedness – decrease by 1-2 mm;
- myopia – an increase of 1 mm or more.
The parameters of other areas of the eye are highlighted:
- The normal thickness of the lens is 4.26 mm, volume – 230 mm. cubic;
- anterior chamber depth – 2.57 mm;
- refractive power of the cornea – 48.22 mm.
A slight increase or decrease in the indicator does not always indicate the development of pathology. This can only be judged if a full diagnosis has been carried out, consisting of several tests.
How is an ultrasound examination of the eyes performed?
The procedure is carried out in a sitting or lying position. It does not require any special preparation and its duration on average ranges from 15 to 30 minutes.
Diagnostics in A-mode is carried out by contact method. The patient is with his eyes open. The sterile probe of the ultrasound machine comes into contact with the eye and is slowly moved across the surface. Tear fluid acts as a natural contact medium. To reduce discomfort and lacrimation due to direct contact of the sensor with the eye, an anesthetic drug is instilled into the patient before the procedure.
Diagnosis in B-mode is carried out with eyes closed. An easily washable water-soluble gel is applied to the eyelids, acting as a contact medium. The specialist moves the sensor across the eyelid, periodically indicating what actions the patient needs to perform with his eyes. The procedure does not involve the use of an anesthetic.
Features of the procedure
- Biometrics is completely safe for people of any age.
- No anesthesia or special drops are used during the study. The patient does not undergo any additional preparation.
- There are no preliminary measures or restrictions.
- The scan is completed in just a few minutes.
- With highly accurate results and personalized values, the device provides surgeons with the ideal conditions to achieve excellent surgical results.
- There is no penetration into the eye structure; the procedure is non-contact.
- The study is carried out on one device and in one session. The patient does not need to go somewhere or visit an ophthalmologist on another day.
- For the reliability of the indicators, the transparency of the optical media is necessary. In case of cloudiness of biological tissues, in most cases, instead of biometry, an ultrasound examination of the eye is prescribed.
- Biometric results can be stored in the database for a long time.
Combination of ultrasound with other diagnostic methods
The high information content of ultrasound does not exclude the need for additional diagnostic methods. In general cases, ultrasound is preceded by taking an anamnesis and conducting a general clinical and ophthalmological examination by the doctor.
If the presence of a foreign object is suspected, an x-ray of the eye is first taken. If the patient is suspected of having intraocular tumors, ultrasound is preceded by diaphanoscopy of the eyeball. To confirm the presence of a space-occupying lesion in the orbit, exophthalmometry and radiography are additionally performed.
Fill out an application on the website, we will contact you as soon as possible and answer all your questions.
Make an appointment
Biometrics of the eye: indications for performance
The study must be carried out before surgical, laser operations, or implantation. For premature babies, the study is carried out at 6 months and 1 year. Up to 5 years - with deterioration of vision, congenital lesions, the appearance of opaque tears, suspected ophthalmological pathologies. Indications for examination are:
- control over developing myopia;
- ophthalmological diseases (cataracts, glaucoma, etc.);
- keratoconus (deformation, thinning of the cornea);
- selection of contact lenses;
- postoperative keratectasia;
- examination of the cornea after transplantation;
- rapid eye fatigue;
- rapid deterioration of vision;
- heaviness of the eyelids when blinking;
- frequent headaches radiating to the eyes;
- deformation or clouding of the cornea;
- distorted, doubled image;
- suspected retinal detachment;
- progressive myopia;
- diagnosis of oncological diseases.
Eye biometrics is carried out as a preventative measure for eye diseases. The method is necessarily used for diabetes mellitus, age-related macular degeneration, and foreign objects getting inside.
Results and discussion
Currently, a high level of accuracy in measuring biometric parameters, the correct use of third-generation IOL calculation formulas and personalized IOL constants make it possible to obtain a planned postoperative refraction of up to ±0.5 diopters and higher, up to absolute. This statement is quite true not only for uncomplicated cataract surgery, but also for avitreal eyes after removal of packing agents. Unfortunately, we have to admit that, despite certain existing recommendations, none of the methods for assessing the value of PPV for avitreal eyes with silicone tamponade can provide guaranteed measurement accuracy.
When we tried to measure PPV in an eye with a silicone tamponade in the standard mode using ultrasound, we obtained values that exceeded the real ones by 10 mm or more, using IOL-Master - by 0.7-2 mm. An error in measuring the PZ value of 1 mm induces an error in postoperative refraction from 1.75 to 3.75 diopters depending on the length of the eye.
Of course, the modern technical level of cataract surgery allows us to quite simply and atraumatically replace an IOL or implant an additional IOL to correct a refractive error, however, this is an additional operation for the avitreal eye and the patient, which can be avoided if there are reliable values of the PZ value.
We continued our research despite K. Hoffer's statement at ASCRS 2012 that for eyes with silicone tamponade, “measurement with ultrasound is almost impossible” (“Almost impossible to measure with Ultrasound”) and the IOL-Master data should be used only as a guide.
Our previous clinical experience indicated that this interpretation of this problem is ambiguous. In addition, during a contextual search and analysis of the available literature, we were unable to find either published results of studies similar to ours, or references to their conduct.
Before discussing the results obtained, we consider it appropriate to present a clinical case illustrating the algorithm for selecting the most reliable data on the value of PZO from a certain range, designated by us as the “confidence band”.
Patient M
., history of operated retinal detachment, immature posterior capsular cataract, silicone tamponade.
The following data were obtained on a phakic eye with a silicone tamponade using modified biometric methods:
PZO at an ultrasonic speed of 980 m/s - 23.55 mm;
PZO at an ultrasonic speed of 1000 m/s - 23.8 mm;
PZO IOL-Master (Silikon Filled Eye mode) - 24.45 mm.
At the initial stages of research, a retrospective analysis of the results led us to some preliminary conclusions, which, with repeated subsequent confirmation, allowed us to form the following approach to the reliability of modified biometrics data:
1. Data obtained with modified ultrasonic biometry at an ultrasound speed of 980 m/s are significantly underestimated.
2. Data obtained with modified ultrasonic biometry at an ultrasound speed of 1000 m/s are close to real ones, but underestimated to a very small extent.
3. The data obtained with the IOL-Master in the “Silicon Filled Eye” mode is slightly overestimated.
Thus, the data that are closest to the real ones are in the range between the values obtained by the method of modified ultrasonic biometry at an ultrasound speed of 1000 m/s and IOL-Master optical biometry in the “Silikon Filled Eye” mode, which we called the “confidence band”.
Accordingly, in our case, we must select the value of the PZO in the range from 23.8 to 24.45 mm, or more precisely, up to 24.25 mm, if we bring the optical value of the PZO into line with the ultrasonic value. An explanation is necessary here, since in the IOL-Master the measurement takes place along the posterior border of the optically transparent neuroepithelium (the average thickness of which is 170 μm), its result should be on average 0.2 mm larger than the echobiometric value.
In clinical practice, with correct measurement, this difference varies from 0.1 to 0.3 (sometimes 0.4) mm. When we analyzed this parameter, which we carried out in a sample of 600 eyes with a range of PZ values from 22.5 to 25.0 mm, in 90% of cases a value of 0.2 mm was obtained.
Bringing the optical value of the PZO into correspondence with the ultrasonic value is necessary for the correct determination of the “confidence band”, since in the calculation we use echobiometric constants and the reference data are the ultrasonic values of the PZO.
For the calculation, a PZ value of 23.9 mm was selected.
Keratometry - 40.87/42.75 diopters.
To calculate the optical power of an IOL for “emmetropia” - 20.64 diopters.
Planned removal of the SM was performed with simultaneous phacoemulsification and implantation of a +20.0 D IOL.
On a pseudophakic eye with the SM already removed, the following data were obtained using standard biometric methods:
Ultrasound PZO (standard mode) - 23.9 mm;
PZO IOL-Master (standard mode) - 24.1 mm.
Obtained clinical refraction:
sph 0.0 diopters, cyl –2.5 diopters ax 102°.
The data obtained, which we have the right to consider as reliable as possible, in our opinion, indicate the sufficient consistency of the presented concept of the “band of reliability”.
In this work, it was not planned to analyze the obtained refractive results, however, it should be noted that in most cases the refraction of the target range was achieved.
The results of the studies are presented in the table.
Results of measuring the value of PZO before removal of SM using modified biometric methods and after removal of SM in standard modes
It should be noted that initially the thematic group included about 200 eyes; standardization according to the above parameters reduced this figure to 60, but in the table we present data from only 30 cases. This is due to the subsequent exclusion from the group of cases with paradoxically absurd data (for example, the ultrasound value of the PZO exceeds the optical value by 3.0 mm) and cases with the loss of one or more study points, which occurred due to the absence of the patient for the study and technical impossibility or inappropriateness of biometrics (opacity of optical media, acoustic artifacts, recurrence of retinal detachment).
However, the data presented, in our opinion, is sufficient to illustrate obvious trends and patterns.
When statistically analyzing the data presented in the table, the following results were obtained:
1. The values of the PZ value obtained using modified ultrasound biometry at an ultrasound speed of 980 m/s against the background of silicone tamponade, in comparison with similar (obviously reliable) data obtained after removal of the SM in the standard mode, had a stable tendency to be underestimated from 0. 0 to 1.5 mm (average 0.52 mm).
2. The values of the PZ value obtained using modified ultrasound biometry at an ultrasound speed of 1000 m/s against the background of a silicone tamponade, in comparison with similar (obviously reliable) data obtained after removal of the SM in the standard mode, were slightly less - in the range from 0 .0 to 0.5 mm (average 0.15 mm).
3. The values of the PZ value obtained using modified optical biometry on the IOL-Master in the “Silikon Filled Eye” mode against the background of silicone tamponade, in comparison with similar (obviously reliable) data obtained after removal of the SM in the standard mode, were greater - in range from 0.0 to 1.2 mm (average 0.3 mm).
Thus, the conducted studies confirmed our assumptions about the possibility of a fairly correct measurement of the value of PZO using modified ultrasound biometry against the background of silicone tamponade, and at an ultrasound speed of 1000 m/s, the data obtained are even closer to the true values than the data obtained using the modified mode on IOL-Master.
The use of modified ultrasonic biometry at an ultrasound speed of 980 m/s in parallel with a value of 1000 m/s may be considered inappropriate due to its obviously lower accuracy.
When bringing the optical value of the PZO into correspondence with the ultrasound value, we obtained a fairly narrow range of the “confidence band” (0.43 mm on average) between the data obtained by the method of modified ultrasonic biometry at an ultrasound speed of 1000 m/s and IOL-Master optical biometry in the “ Silikon Filled Eye”, which makes it possible to relatively safely select a value for the subsequent calculation of IOL optical power.
Optical biometrics
Optical biometric examination of the eye is primarily indicated for patients in ophthalmology clinics who need to undergo a more detailed diagnostic examination before undergoing laser vision correction.
Reference. To carry out diagnostics, an optical biometer is used - a device that measures all the necessary parameters of the eye without any contact with the organ.
Using a contactless biometric study, you can find out the following parameters:
- The depth of the anterior axis of the eyeball and determination of the dimensions of the eye axis;
- Keratometry is a thorough examination of all the necessary parameters of the cornea of the eye.
- Calculation of lens thickness . This parameter is necessary in order to determine the exact power of the intraocular lens before implanting it.
During the procedure, the patient does not experience discomfort or any unpleasant sensations. Diagnostics is carried out very quickly and is suitable for examining patients of any category with a wide variety of ophthalmological diseases.
If we take into account the level
of accuracy of this diagnostic method, then optical biometry is much better than the ultrasound examination method.
However, optical biometry of the eye also has one drawback - the procedure is not performed if there is even the slightest cloudiness ; the organ must be absolutely transparent. If even the slightest clouding is detected, the patient is sent for an ultrasound examination.
UDC 617.753.2
E.G. SOLODKOVA
Volgograd branch of the MNTK “Eye Microsurgery named after. acad. S.N. Fedorov Ministry of Health of the Russian Federation, 400138, Volgograd, st. Zemlyachki, 80
Solodkova Elena Gennadievna - head of the department of correction of refractive errors, tel. e-mail:
21 patients (42 eyes) with myopia were examined: 7 people (14 eyes) with mild myopia, 8 people with moderate myopia. (16 eyes), high degree - 7 patients (14 eyes). Analysis of pachymetric and biometric data of the eyeballs obtained using various methods in patients with myopia showed the absence of statistically significant differences between the measurement results (t<2.0; p>0.05). The research results are comparable to each other, correct and can be interchanged in clinical practice.
Key words: myopia, pachymetry, corneal biometry.
EG SOLODKOVA
The Volgograd Branch of the S. Fyodorov Eye Microsurgery Federal State Institution, 80 Zemlyachki Str., Volgograd, Russian Federation, 400138
Analysis of pachymetry and biometrics cornea results in patients with myopia
Solodkova EG ― Head of the Department of Refraction Abnormalities Correction, tel. (8442) 91-72-62, e-mail:
The study included 21 patients (42 eyes) with myopia: mild myopia - 7 people (14 eyes), moderate - 8 people (16 eyes), and high - 7 patients (14 eyes). The analysis of pachymetric and biometric data obtained by various methods in myopic patients showed no statistically significant difference between the measurements (t<2.0; p>0.05). The research results are comparable with each other, correct and can be used interchangeably in clinical practice.
Key words: myopia, pachymetry, corneal biometry.
There are various methods for assessing pachymetric and biometric parameters of the eye, based on various physical principles. The most common principle of ultrasound examination of the morphometric parameters of the eyeball is to register the ultrasound signal reflected from the interfaces of media with different densities [1-3]. The study is carried out using the applanation, contact method. The advantage of the method is its accessibility and ease of implementation, however, the accuracy of measurements may decrease due to varying degrees of compression of the cornea during applanation with the sensor. The ability to conduct a non-contact study of the morphological parameters of the eyeballs in conditions of reduced transparency of optical media is provided by the method of non-invasive coherent automatic optical biometry, which is based on the principle of non-contact measurement of biometric parameters using an infrared laser (wavelength 780 nm). Thus, the operation of the IOL Master 500 device (Carl Zeiss MediTec AG) is carried out [4-6].
The operating principle of the Scheimpflug analyzers Galilei G6 (Ziemer Ophthalmic Systems AG, Switzerland) and Sirius (Schwind Eye-tech-solutions GmbH & Co. KG, Germany) is similar, and consists in constructing a three-dimensional model of the structures of the anterior segment of the eye using the method of combined video cartoscopy. It is based on a combination of two technologies: the Placido disk and the Scheimpflug camera. The differences lie in the technical implementation of the task in the devices - the presence of two Scheimpflug chambers and a flat-shaped Placido disk in the Galilei G6 analyzer and one Scheimpflug chamber and a conical Placido disk in the Sirius analyzer [7-10]. Such a variety of technical approaches to the study of biometric and pachymetric parameters of the eyeball dictates the need to evaluate their accuracy in comparison with each other, as well as determine the range of their application.
The purpose of the work is to compare the values of pachymetric and biometric parameters of the eyeballs of patients with various degrees of myopia, obtained using various methods.
Material and methods
In the department of correction of refractive errors of the clinic of the Volgograd branch of the MNTK "Eye Microsurgery" named after. acad. S.N. Fedorov examined 21 patients (42 eyes) with myopia. Of these, 7 people (14 eyes) had mild myopia, 8 people had moderate myopia. (16 eyes), as well as with high myopia - 7 patients (14 eyes). The average age of the patients was 23.4 years. Men - 11 people, women - 10 people.
All patients underwent an extensive ophthalmological examination, including visometry with determination of BCVA and distance BCVA, autorefractometry, including in conditions of drug-induced cycloplegia with determination of the sphero-equivalent value of refraction, tonometry, ophthalmobiomicroscopy, fundus ophthalmoscopy with a three-mirror Goldmann lens. Ultrasound applanation keratopachymetry (Tomey AL-3000, Japan), keratotopographic examination with pachymetry using a Sirius Scheimpflug corneal analyzer (Schwind Eye-tech-solutions GmbH&Co. KG, Germany) and a Galilei G6 Scheimpflug analyzer (Ziemer Ophthalmic) were used to measure corneal thickness Systems AG, Switzerland). To measure the axial length of the eyeball, ultrasound applanation biometry, optical biometry using IOL Master 500 devices (Carl Zeiss MediTec AG) and a Scheimpflug analyzer Galilei G6 (Ziemer Ophthalmic Systems AG, Switzerland) were used.
Statistical processing of variation series was carried out using computer applications Microsoft Excel 2003, StatPlus 2009 and included calculation of arithmetic means (M) and standard errors of arithmetic means (m), standard deviation (σ). The work used methods of parametric statistics (Student's t-test). In general, differences were recognized as statistically significant if the level of significance (p) was more than 95.0% (p<0.05) or more than 99.0% (p<0.01); in other cases, the differences were considered statistically insignificant (p>0.05).
Results and discussion
Pachymetric indicators obtained by various methods are presented in Table 1.
Table 1.
Pachymetric parameters in patients with myopia, ( M±σ)
| Method/Group | Low myopia | Moderate myopia | High myopia |
| Ultrasonic pachymetry | 536,9±15,15* | 538,47±29,9* | 535,0±38,9* |
| Sirius | 540,3±15,7* | 542,13±27,18* | 534,8±47,59* |
| Galilei G6 | 547,9±16,59* | 546,9±29,13* | 543,8±41,5* |
Note: differences between average values marked with * are not statistically significant (t<2.0, p>0.05)
Ophthalmobiometric indicators obtained by various methods are presented in Table 2. Analysis of pachymetric and biometric data of the eyeballs obtained using various methods in patients with myopia showed the absence of statistically significant differences between the measurement results.
The minimum pachymetry and ophthalmobiometry values were obtained using ultrasound applanation examination, the maximum values were obtained using a Galilei G6 Scheimpflug analyzer (Fig. 1, 2). The obtained data are consistent with the literature data [6].
Picture 1.
Distribution of pachymetry values obtained by different methods
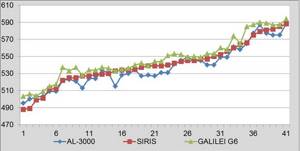
Figure 2.
Distribution of eye biometric values obtained by various methods
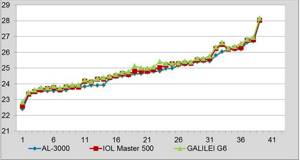
Table 2.
Ophthalmobiometric indicators in patients with myopia, ( M±σ)
| Method/Group | Low myopia | Moderate myopia | High myopia |
| Ultrasonic pachymetry | 24,1±0,8* | 25,3±0,8* | 26,45±1,13* |
| IOL Master 500 | 24,23±0,8* | 25,44±0,8* | 26,57±1,1* |
| Galilei G6 | 24,3±0,8* | 26,89±0,7* | 26,7±1,0* |
Note: differences between average values marked with * are not statistically significant (t<2.0, p>0.05)
The minimum values of pachymetry and ophthalmobiometry obtained using the applanation ultrasound method are due to compression of the cornea by the ultrasonic sensor; on the other hand, some overestimation of biometric parameters observed when using non-contact research methods can be explained by the reflection of infrared laser radiation not from the internal limiting membrane of the retina, but from the pigment epithelium.
The obtained research results are comparable to each other, correct and can be interchangeable in clinical practice, depending on various clinical situations.
LITERATURE
- Fridman F.E., Gundorova R.A., Kodzov S.B. Ultrasound in ophthalmology. - M.: Medicine, 1989. - P. 50.
- Eletheriadis H. IOL Master biometry: refractive results of 100 consecutive cases // Br. J. Ophthalmol. - 2003. - Vol. 87. ― P. 960-963.
- Huang J., Lu W., Savini G. Evaluation of corneal thickness using a Scheimpflug-Placido disk corneal analyzer and comparison with ultrasound pachymetry in eyes after laser in situ keratomileusis // Journal of Cataract and Refractive Surgery. - 2013. - Vol. 39, no. 7. - R. 1074-1080.
- Avetisov S.E., Voroshilova N.A., Ivanov M.N. Optical coherent biometry // Bulletin of Ophthalmology. - 2007. - No. 4. - pp. 46-47.
- Findl O., Kriechbaum K., Sacu S. Influence of operator experience on the performance of ultrasound biometry compared to optical biometry before cataract surgery // Journal of Cataract and Refractive Surgery. - 2003. - Vol. 29. ― No. 10. - R. 1950-1955.
- Utine CA, Altin F., Cakir H. Perente I. Comparison of anterior chamber depth measurements taken with the Pentacam, Orbscan IIz and IOL Master in myopic and emmetropic eyes // Acta Ophthalmologica. - 2009. - Vol. 87, no. 4. - R. 386-391.
- Read SA, Collins MJ Diurnal variation of corneal shape and thickness // Optometry and Vision Science. - 2009. - Vol. 86, no. 3. - R. 170-180.
- Savini G., Carbonelly M., Barboni P., Hoffer KJ Repeatability of automatic measurements performed by a dual Scheimpflug analyzer in unoperated and post-refractive surgery eyes // J. Cataract Refract. Surg. ― ― Vol. 37. ― P. 302-309.
- Shammas HJ, Hoffer KJ, Shammas MC Scheimpflug photography keratometry readings for routine intraocular lens power calculation // Journal of Cataract and Refractive Surgery. - 2009. - Vol. 35, No. 2. - R. 330-334.
- Sheng H., Bottjer CA, Bullimore MA Ocular component measurement using the Zeiss IOL Master // Optometry and Vision Science. - 2008. - Vol. 8, No. 1. - R. 27-34.
REFERENCES
- Fridman FE, Gundorova RA, Kodzov SB Ul'trazvuk v oftal'mologii . Moscow: Meditsina, 1989. P. 50.
- Eletheriadis H. IOL Master biometry: refractive results of 100 consecutive cases. Br. J. Ophthalmol, 2003, vol. 87, pp. 960-963.
- Huang J., Lu W., Savini G. Evaluation of corneal thickness using a Scheimpflug-Placido disk corneal analyzer and comparison with ultrasound pachymetry in eyes after laser in situ keratomileusis. Journal of Cataract and Refractive Surgery, 2013, vol. 39, no. 7, rr. 1074-1080.
- Avetisov SE, Voroshilova NA, Ivanov MN Optical coherence biometry Vestnik oftal'mologii, 2007, no. 4, pp. 46-47 (in Russ.).
- Findl O., Kriechbaum K., Sacu S. Influence of operator experience on the performance of ultrasound biometry compared to optical biometry before cataract surgery. Journal of Cataract and Refractive Surgery, 2003, vol. 29, no. 10, rr. 1950-1955.
- Utine CA, Altin F., Cakir H. Perente I. Comparison of anterior chamber depth measurements taken with the Pentacam, Orbscan IIz and IOL Master in myopic and emmetropic eyes. Acta Ophthalmologica, 2009, vol. 87, no. 4, rr. 386-391.
- Read SA, Collins MJ Diurnal variation of corneal shape and thickness. Optometry and Vision Science, 2009, vol. 86, no. 3, rr. 170-180.
- Savini G., Carbonelly M., Barboni P., Hoffer KJ Repeatability of automatic measurements performed by a dual Scheimpflug analyzer in unoperated and post-refractive surgery eyes. J. Cataract Refract. Surg, 2011, vol. 37, pp. 302-309.
- Shammas HJ, Hoffer KJ, Shammas MC Scheimpflug photography keratometry readings for routine intraocular lens power calculation. Journal of Cataract and Refractive Surgery, 2009, vol. 35, no. 2, rr. 330-334.
- Sheng H., Bottjer CA, Bullimore MA Ocular component measurement using the Zeiss IOL Master. Optometry and Vision Science, 2008, vol. 8, no. 1, rr. 27-34.
Ultrasound biometrics
Ultrasound examination of the eye is the diagnostic standard in ophthalmology. A and B methods are used to assess the condition of various structures of the eye that cannot be seen by optical methods. Ultrasound is safe to use and has virtually no contraindications.
How does ultrasound biometry work?
Ultrasound biometry using the A-method is a contact procedure that is used to determine the thickness of the cornea, lens, depth of the anterior chamber, and axial length of the eye. Before the examination, drops are instilled into the eye for pain relief and an ultrasound probe is applied to the cornea of the eye. All necessary parameters are displayed on the device screen, assessed by an ophthalmologist and recorded.
Ultrasound B-scan is performed for mature cataracts and opaque environments of the eye in order to determine the condition of the retina, choroid and optic nerve. The doctor applies a special gel to the patient's eyelid to facilitate the conduction of ultrasound waves. After this, a sensor is brought to the eye, through which the sound wave passes through the internal structures of the eye, is reflected from them, turns into an electrical signal and creates an image on the screen and is evaluated by the eye using a special program.
In our clinic, the examination takes only 3-5 minutes. We guarantee the accuracy of the measurement and the absence of discomfort for the patient. Ultrasound biometry is performed on the Compact Touch diagnostic system (Quantel medical, France)