Is it possible to take dental x-rays during pregnancy?
The condition of the teeth and oral cavity often seems to us to be something of secondary importance. Meanwhile, our success depends on it (after all, when communicating with people, bad teeth and bad breath are of great importance), the health of our internal organs (since the infection quickly moves down the esophagus) and well-being (many consider toothache simply unbearable). Therefore, it is necessary to take care of your teeth all the time. If everything is not in order in your oral cavity, then with the onset of pregnancy, be sure to only expect it to worsen. And even with relatively healthy teeth, it is often impossible to avoid their treatment: the developing fetus draws a lot of calcium from the mother’s body, and if there was not enough of it before, then you can even say goodbye to the teeth.
In a word, there is a high probability that during the period of bearing your baby you will have to see a dentist and, perhaps, be faced with a choice: to take a dental x-ray during pregnancy or not.
There is no consensus among dentists themselves on this issue. While some of them reassure their patients that modern dental x-rays during pregnancy do not harm either the woman or the child, others continue to defend the point of view that has been established over the years: there is no such thing as a harmless x-ray.
Each specialist will have his own reasons why he speaks and thinks this way and not otherwise. And it can be difficult for an excited expectant mother to decide which side to cling to.
General information and advice for all pregnant women during the coronavirus pandemic
Information for pregnant women and their families.
This information is not intended to meet your specific individual health care needs based on your medical condition. This information is not a clinical diagnosis of your health condition. If you are concerned about your health or general well-being, we strongly encourage you to contact your healthcare provider if necessary.
General information and recommendations for all pregnant women during the coronavirus pandemic.
Question: What effect does coronavirus have on pregnant women?
In general, pregnant women are no more likely to become seriously ill than other healthy adults if they become infected with coronavirus. The vast majority of pregnant women are expected to experience only mild to moderate cold/flu symptoms. Cough, fever, shortness of breath, headache and loss of smell are suspected symptoms of coronavirus infection.
Severe complications such as pneumonia are more common in older adults, people with weakened immune systems, or people with long-term chronic illnesses. There is still no evidence that pregnant women who become infected with coronavirus are at greater risk of developing serious complications than any other healthy people. Our advice remains the same: if you feel your health is getting worse or not getting better, you should contact your obstetrician/gynecologist or antenatal clinic.
Question: What effect will coronavirus have on my child if I am diagnosed with this infection?
Because this is a very new virus, we are just beginning to learn about it. There is no evidence to suggest an increased risk of miscarriage.
Emerging evidence suggests that transmission from a woman to her baby during pregnancy or childbirth (vertical transmission) is likely. There are two case reports in which this seems likely, but it is encouraging that both children have been released from hospital and are healthy. In all previously reported cases worldwide, infection was detected at least 30 hours after birth. It is important to emphasize that in all registered cases of coronavirus development in newborns, the child was healthy after birth.
Given current evidence, it is considered unlikely that if you are infected with coronavirus it will cause problems with your baby's development.
In China, some babies are being born prematurely to women with coronavirus symptoms. However, it is unclear whether the coronavirus caused these premature births, or whether the delivery was carried out earlier in accordance with the doctor's decision, for the benefit of the women's health.
Question: What can I do to reduce my risk of contracting coronavirus?
The most important thing to do is to follow the general requirements. For pregnant women and other members of their families, this includes:
regular hand washing;
use a tissue when you or someone in your household coughs or sneezes, throw it away and wash your hands;
Avoid contact with anyone showing symptoms of coronavirus. These symptoms include fever and/or cough;
Avoid using public transport if possible;
work from home if possible;
avoid visiting public places, as the infection spreads easily in closed spaces;
Avoid meeting friends and relatives. Keep in touch using remote technologies such as telephone, internet and social media;
Use telephone or online services to contact your doctor or other essential services.
Question: I'm pregnant, what should I do?
As a precaution, you should follow general health advice about social distancing.
Stay away from public places and avoid those with symptoms of acute respiratory infection when going out to buy food, exercise and attend antenatal clinic appointments.
If you are in the third trimester of pregnancy (over 28 weeks), you should be especially careful about social distancing and minimizing any contact with other people.
Question: Should I attend my prenatal and postnatal appointments at an antenatal clinic?
Yes. When you are healthy, it is indeed very important that you continue with your scheduled medical visits.
If you have symptoms of possible coronavirus infection, you should contact your doctor to postpone routine visits until after your isolation period.
If you are currently healthy and have not had any complications during previous pregnancies, you may find the following practical advice helpful:
If you are due for a routine examination or visit in the coming days, please contact your antenatal clinic to obtain and agree a plan for your follow-up care. Visiting times may change.
If you have been advised to attend a test or make an appointment at an antenatal clinic, this is because the need for this appointment is greater than the risk of contracting coronavirus. Antenatal care is essential to maintaining a healthy pregnancy, so we strongly encourage you to adhere to appointment times if you are asked to do so. If you have any concerns about this, please discuss them with your OB/GYN doctor.
Regardless of your personal situation, please consider the following:
The maternal and child health system is important and has been developed over many years to reduce the likelihood of possible complications in women and children. The risks of not attending antenatal care include harm to you, your baby or both of you, also in the context of coronavirus. It is important that you keep in touch with your antenatal clinic and continue to attend scheduled appointments when you are feeling well. If you have any concerns, please contact your OB/GYN physician, but please note that medical staff are working harder right now.
If you have symptoms of coronavirus, please contact your antenatal clinic and they will arrange the correct place and time for you to visit. You will be asked to come to your appointment alone or to keep the number of people with you to one. We ask that children not accompany you during this time.
You may need to reduce the number of prenatal visits. Your obstetrician-gynecologist will tell you about this. We assure you that this change will be made as safely as possible, taking into account available evidence regarding the safe number of visits required. Please do not reduce the number of visits without first discussing this with your doctor.
Question: What should I do if I get a fever or temperature, or both, while I'm pregnant?
If you have a fever or cough, or both, during pregnancy, you should contact your doctor for advice about the isolation you should follow in accordance with current regulations. However, please also be aware of other possible causes of fever during pregnancy. These include bladder infections (cystitis) and other conditions. If you have any burning or discomfort when urinating, or any unusual vaginal discharge, or have any concerns about your baby's movements, contact your healthcare provider, who will be able to provide further advice.
Question: What should I do if I think I may have or have been exposed to coronavirus?
You should contact your antenatal clinic to tell them that you have symptoms suggestive of coronavirus, especially if you have an appointment within the next 7 days.
Question: How will I get tested for coronavirus?
The process of diagnosing coronavirus infection is changing rapidly. If you do need to take a test, you will take it just like everyone else, regardless of whether you are pregnant.
Question: What should I do if I test positive for coronavirus?
If you test positive for coronavirus, you should contact your antenatal clinic to tell them about your diagnosis. If you have no symptoms or mild symptoms, you will be advised to recover at home. If you have more severe symptoms, you may be sent to hospital for treatment.
Question: Can I pass coronavirus to my child?
Because this is a new virus, there is limited data on the care of women with coronavirus infection when they have just given birth. A small number of babies have been diagnosed with coronavirus shortly after birth, so it is possible that infection may have occurred in the womb, but it is not yet known exactly when transmission occurred before or after birth. The healthcare team will maintain strict infection control measures during your birth process and monitor your baby closely.
Question: Will my child be tested for coronavirus?
If you are confirmed or suspected of having coronavirus when your baby is born, doctors who specialize in newborn care (neonatal doctors) will examine your baby and advise you about its care, including whether it needs testing.
Question: Will I be able to breastfeed my baby if I have suspected or confirmed coronavirus?
Yes. There is no evidence that the virus can be carried or transmitted in breast milk. The well-established benefits of breastfeeding and the protection it provides babies outweigh any potential risks of coronavirus transmission through breast milk. As long as your baby is healthy and does not require care in the neonatal unit, you will remain together after the birth.
The main risk of breastfeeding is the close contact between you and your baby, so if you cough or sneeze, it can contain droplets that are contaminated with the virus, leading to infection of the baby after birth.
A discussion about the risks and benefits of breastfeeding should take place between you and your neonatologist.
When you or anyone else feeds your baby, it is recommended that you take the following precautions:
wash your hands before touching your baby, breast pump or bottles;
Try not to cough or sneeze on your baby while breastfeeding;
consider wearing a mask while breastfeeding;
Follow the recommendations for cleaning the breast pump after each use;
If you decide to feed your baby formula or expressed milk, it is recommended that you strictly adhere to sterilization recommendations. If you express breast milk in hospital, you should use a special breast pump.
Question: Is there an increased risk for me or my baby after giving birth?
There is no evidence that healthy women who have recently given birth are at increased risk of contracting coronavirus. A newly pregnant woman's immune system is considered normal unless she has other forms of infection or underlying disease. You should eat well, exercise moderately, and ensure social distancing is maintained. Children, including newborns, do not appear to be at high risk of becoming seriously ill from the virus. However, careful hygiene is important for family members living in the house. Anyone entering the home should follow standard hygiene precautions, including hand washing, and be careful when handling your child if they have symptoms of any illness, including coronavirus.
It is important that your baby eats well and gains weight, and if you have any concerns please contact your doctor.
Don't delay seeking medical care if you have concerns about your child's health during the pandemic. Call your doctor if your child has a fever, lethargy, irritability, poor appetite, or any other symptoms that concern you.
Modern methods are quite safe
Recently, more and more dentists are offering dental x-rays to pregnant women when they come to see them. The photograph definitely has a number of advantages over blind tooth treatment. Not every dentist has the gift of clairvoyance to be firmly sure where and how the canals lie and what is going on in this diseased tooth. It’s better to take an x-ray and do the job right away with high quality than to open the fillings later and again torment the tooth, the patient, and yourself as well.
Perhaps it is difficult to disagree with this, but not when a pregnant woman comes to the dentist. After all, even if the radiation dose is minimal, pregnancy is still not the time for experiments and such influences. At least that's what they always thought, it seems.
But today this point of view is undergoing some changes. Since visiographs began to appear in dental offices, dental specialists offer dental x-rays to pregnant women without much concern and explain why.
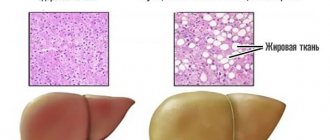
Firstly, the beam of an electronic radiovisiograph is narrowly directed: it passes only through a specific tooth, without spreading to nearby tissues and areas. Secondly, the ray passing through the tooth cannot in any way enter the stomach or somehow affect the life developing inside it. Thirdly, the device emits microdoses (the effect lasts literally a split second) equal to the normal background radiation. Moreover, experts say that the dose of radiation received while exposed to the rays of the summer sun exceeds that emitted by the visiograph, so there is no harm in talking about it in principle. Well, fourthly, what we have already mentioned: an X-ray of a tooth during pregnancy allows the dentist to do the job efficiently the first time (although practice, unfortunately, shows that this is not always the case).
Dentists use simple mathematical calculations to defend their point of view. X-rays are truly unsafe for the unborn child. But, according to scientific data, a defect in fetal development occurs in 4-5% of cases only with a radiation dose of 1 rad. If you take several pictures in a row to cover the entire oral cavity (in practice this is not necessary), then the woman will receive 0.0001 rad of radiation.
And modern equipment generally allows dental x-rays to be taken during pregnancy, even without the use of special protection. But not all dentists believe in absolute safety (after all, the radiation dose, although minimal, is not zero) and, in the old fashioned way, recommend postponing dental treatment to the postpartum period if the situation can wait.
Introduction
Fluorography is a type of x-ray examination that produces a reduced image of organs. We have prescribed that every person over 14 years of age undergo an annual chest fluorography (FXF). With FLGOGK, X-ray radiation is 40% less than with radiography. The effect of X-ray radiation on a potential pregnancy is a very delicate issue and requires a strictly individual approach.
This type of radiation can destroy DNA or promote the formation of free radicals, which leads to teratogenesis (fetal malformations), carcinogenesis (growth of tumors) and mutations (changes in DNA).
These changes are observed when exposed to high doses of X-ray radiation and prolonged exposure. For example, after a nuclear power plant accident or a nuclear bomb test. During diagnostic studies, the doses of ionizing radiation are negligible and, according to doctors, are safe. It will help you more or less navigate the doses.
.
Still, I would like to exclude even the potential risk during pregnancy.
In the case of routine fluorography, everything is simple. If you do not know the date of ovulation, use contraception in the cycle in which a medical examination is planned, and leave conception for the next time. Knowing the date of ovulation, you can undergo fluorography before its onset, then there is no need for contraception.
And if the disease has an acute or sudden onset. For example, an injury, but the woman does not yet know about pregnancy and an x-ray or fluorography was taken? Tell your doctor who is caring for your pregnancy about this.
Neither fluorography nor x-rays during pregnancy are indications for medical abortion.
When is it better to refrain from dental x-rays during pregnancy?
American scientists conducted studies on the basis of which they came to the conclusion that undergoing dental x-rays during pregnancy potentially increases the risk of having a child with insufficient body weight by 5%.
Not all colleagues agree with the Americans, but still many dental specialists prefer to play it safe once again. The fact is that it has not been scientifically proven that dental x-rays during pregnancy are truly harmless. In the same way, on the contrary - that it does some harm. Therefore, undergoing an x-ray is considered relatively safe by default. However, especially careful dentists try to delay such a diagnosis as much as possible if time is of the essence.
The human factor also plays a role here: if something happens to the child of a woman undergoing an x-ray in a dental clinic in the future, then, it is possible, the harmlessness of the x-ray will have to be proven in court.
Figures and facts from America
According to the American Academy of Family Physicians, to receive a damaging dose of X-ray radiation, a pregnant woman must undergo:
- 50,000 dental images;
- 5000 x-rays of the upper or lower limb;
- 2500 photographs of the skull;
- 555 studies of the thoracic spine;
- 250 mammograms;
- 125 x-rays of the pelvis;
- 23 hip shots;
- 20 x-rays of the abdominal cavity;
- 13 x-rays of the sacral spine;
- 3 intravenous pyelograms (examination of the kidneys with intravenous contrast);
- 1 x-ray computed tomography;
X-ray examination is recommended to be done only if there is an urgent need or there are no other alternative diagnostic procedures. This is the opinion of American experts.
What can be the consequences of a dental x-ray during pregnancy?
It is advisable to resort to x-rays and dental treatment during pregnancy only if the source of inflammation threatens the development of infection in the oral cavity (this certainly causes some harm to the fetus). The specialist makes a decision separately in each individual case. If treatment turns out to be necessary, it is best to choose the second trimester of pregnancy (after the 16th week).
You must notify the dental clinic staff about your pregnancy, even if it is only possible. In the case of an X-ray of a tooth, it is necessary to use special protection - a lead apron, which covers the area of the chest, abdomen and pelvis, creating armor for X-rays.
If there is a visiograph in your city, then it is better to undergo diagnostics using it. Unlike outdated devices, it allows you to take up to 15 pictures at a time without harm to the body (of course, it is not at all necessary that there will be a need for this), since it emits a dose 10 times less than the radiographs we are used to.
Well, of course, the best thing would be to properly care for the oral cavity and provide the body with a sufficient amount of calcium (preferably of natural, plant origin) so that the question of whether it is possible to take dental x-rays during pregnancy does not arise at all. Be healthy!
Category Pregnant Published by kosmetik-dent
Let's weigh the risks first
At the very beginning, in the early stages, up to 5 weeks of pregnancy, the “All or nothing” law applies. Any damage to the embryo causes its death; on the other hand, it is not so easy to damage it. Nature has provided many degrees of protection for nascent life. However, during this period there is a high risk of miscarriage, under the influence of x-ray radiation, and if the pregnancy continues, then everything is fine. The X-ray did not result in any adverse effects. The expectant mother can relax.
The highest risk of congenital malformations of the fetus is the period of organ formation - organogenesis. From the 5th to the 16-17th week of pregnancy. Damage, most often to the nervous system, has been reported from exposure to significant doses of radiation.
After the 20th week of pregnancy, the risk to the fetus is equal to the risk to the woman. That is, if necessary, you can safely go for an x-ray?
So what should we do?!
First of all, you should ask your doctor these three questions:
- Is there an examination method that will replace x-ray/fluorography?
- What happens if we don't do x-rays/fluorography?
- Can the diagnostic procedure wait until the eighteenth week of pregnancy or until the baby is born?
Then, if fluorography is necessary and irreplaceable, try to find a clinic with a digital fluorograph. In digital devices, the radiation intensity is 5-10 times lower than in old analog fluorographs.
If we haven’t found it, we still go for the procedure.
The health of the mother is the most important criterion for the health of her unborn child!
Let's put on protection! Ask the radiologist to put a protective apron on you. If you don’t know your status or suspect early pregnancy, say that you may be pregnant. Additional protection wouldn't hurt.
If an older child needs an x-ray and the mother is pregnant, ask someone close to you to be present during the procedure. If you are not close, warn the radiologist about your pregnancy and be sure to wear a protective apron.