A radiograph (x-ray) of the cervical spine is performed to investigate the cause of neck pain, especially after injury or in cases of chronic neck pain with upper limb symptoms, numbness or tingling. Due to the structural features of this part of the spine, it is very labile and vulnerable to various pathologies. Any sudden movement or awkward position can lead to severe pain, disruption of anatomical structures and the onset of degenerative processes. Of all diagnostic methods, the most common is radiography of the cervical spine, which shows how vulnerable this area of the human body is. This is the safest and highest quality diagnostic method.
Interpretation of results
In cases of trauma, an X-ray of the cervical spine is usually immediately interpreted by a traumatologist or surgeon. Sometimes a radiologist may also be asked to interpret the images.
Non-emergency X-rays of the cervical spine are recorded by a radiologist and a report is usually sent to the physician who ordered the examination. The radiologist usually describes the position of the vertebrae and the presence or absence of signs of pathological changes usually associated with normal aging and known as degenerative changes or osteoarthritis.
What does a spine x-ray show?
An X-ray of the spine can detect:
- pathological or physiological curvature of the spinal column;
- changes in the structure of vertebral bone tissue;
- tumor processes (for example, metastases to the spinal column);
- damage to articular surfaces;
- violation of the integrity or symmetry of the vertebrae;
- accumulation of fluid in joint cavities;
- changes in the vertebral discs;
- bone growths.
The essence of the procedure and indications
Radiography is called an instrumental study based on the use of x-rays. This method is inexpensive and at the same time very informative.
An X-ray of the cervical vertebrae will help identify the following diseases:
- pathological lordosis of the cervical spine;
- pathological kyphosis;
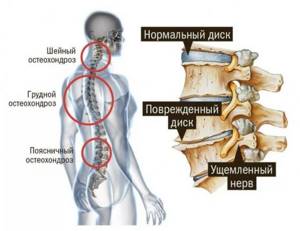
- osteochondrosis of the cervical spine;
- intervertebral hernia, protrusion (indirect signs);
- consequences of injury.
- broken bones
- swelling in or near the trachea
- thinning of the neck bones due to osteoporosis
- bone tumors or cysts
- chronic wear and tear of the discs and joints of the neck, called cervical spondylosis
- joint dislocations
- abnormal growths on the bones called osteophytes
- spinal deformities
- swelling around the vocal cords, called croup
- inflammation of the epiglottis, called epiglottitis
- a foreign object that is stuck in the throat or airway
- enlarged tonsils and adenoids
A correct diagnosis allows you to prescribe adequate treatment to avoid complications and irreversible processes, such as compression of the spinal cord. This is fraught with systemic disorders that can lead to partial or complete paralysis.
X-ray of the cervical vertebrae is indicated for the following symptoms:
- headache;
- feeling of stiffness in the neck;
- noise in ears;
- pressure surge;
- numbness and tingling in the hands;
- shortness of breath;
- severe dizziness.
X-ray examination helps to determine the pathology of the bone apparatus only. If there is damage to soft tissues, then it is necessary to use other research methods such as MRI or CT.
What diseases can be detected by a spinal x-ray?
An X-ray of the spine helps diagnose the following diseases and pathologies:
- spinal injuries (fractures, vertebral dislocation, subluxation);
- compression (compression) of the vertebrae;
- curvature of the spinal column (scoliosis, lordosis, kyphosis);
- osteochondrosis;
- osteoporosis;
- degenerative changes of the spine (for example, osteoarthritis);
- spinal tuberculosis;
- tumor changes;
- congenital anomalies of the spine;
- systemic diseases (rheumatoid arthritis, ankylosing spondylitis, etc.).
Where can an x-ray be taken?
Most hospitals have digital x-ray equipment. The patient receives a very small dose of radiation that is safe for his health. Therefore, the examination can be prescribed for both elderly and children. Pregnant women usually do not have x-rays except in some emergency cases. Diagnostics are carried out in special rooms protected by screens that prevent the penetration of X-rays beyond their boundaries. Internal organs are also protected with lead aprons.
Preparing for X-rays
There is no need to pre-prepare the patient for the test procedure. It is enough to remove clothes from the upper part of the body and remove all metal elements: jewelry, cufflinks, fasteners, removable dentures. When undergoing routine radiography, the patient should be familiar with these requirements in advance so that he can choose clothes that are easily removed and leave all jewelry at home.
Why is it necessary to remove all metal objects? Metal is not capable of transmitting X-rays, so the results of the study may be unreliable.
Preparation and procedure
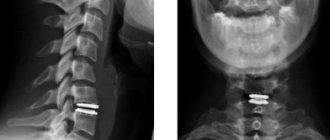
The preparation is very simple: the patient must undress to the waist and remove jewelry with metal, as they can deteriorate the quality of the image. Typically, X-rays of the cervical spine are prescribed in two projections: anterior and lateral. Sometimes a picture is taken of the front of the cervical vertebrae, through the open mouth.
For a high-quality and clear image, the patient must take the correct position and lie completely still during the examination. The procedure takes no more than 20 minutes and does not bring any discomfort to the patient.
It is important to take x-rays of the cervical spine in two projections, because the image shows a two-dimensional image of the patient's body. To obtain a clear and objective picture of the disease, the doctor compares two images of the same part of the spine.
Indications for use

The neck is the most mobile and flexible part of the spine. In this zone there are vessels that supply the brain, as well as nerve bundles that provide the functionality of the upper half of the human body. Therefore, when the first symptoms appear that indicate pathology of the cervical spine, you should immediately consult a doctor in order to make an accurate diagnosis and prescribe effective therapy.
There are a number of symptoms, upon identification of which the doctor prescribes this type of study to the patient. These symptoms include:
- neck pain that gets worse with movement;
- limited head mobility;
- constant headaches, throbbing pain when bending or moving the neck;
- impaired functionality of the upper extremities – numbness, weakness;
- crunch in the neck when moving;
- gait disturbance;
- injuries to the neck, head and shoulder complex;
- a history of degenerative spinal diseases;
- the development of an infection in the body that can pathologically affect the spine.
In some cases, radiography is the only way to establish the correct diagnosis, because many ailments and pathologies have similar symptoms.
X-ray of the neck with functional tests
If there are signs of instability of the motion segments (listhesis) or the likelihood of deformation of the spinal canal, an additional x-ray of the cervical spine with functional tests may be prescribed.
A functional test is an additional procedure used in examining internal organs, allowing a more detailed and informative diagnosis to be made.
In the study of the musculoskeletal system, only mechanical functional tests are used. This means that x-rays of the cervical spine are taken with the patient in full flexion and extension of the neck. This research method allows you to more accurately determine the degree of instability of the motor segments of the spine.
Equipment
In our clinic, neck x-rays and other types of x-ray examinations are performed using modern digital equipment. Digitizing images allows you to achieve impeccable clarity of the picture and make the pictures extremely reliable. With their help, an orthopedist or neurologist can make an accurate diagnosis and prescribe adequate treatment. In addition, innovative equipment speeds up the process of x-ray scanning of an organ several times, thereby significantly reducing the radiation dose. The patient receives diagnostic results immediately after the procedure in the form of images on paper or in digital format on electronic media.
What the doctor won't see in the picture
X-ray examination, although informative, does not give a complete picture of the presence of pathologies in the cervical area. The technique has been used for a long time and in attempts to modernize X-rays, new types of diagnostics have appeared, however, some pathologies are still unattainable for X-rays today.
Even with a clear image, a doctor may not identify the following pathologies:
- small hematomas;
- minor cracks or fractures;
- small neoplasms.
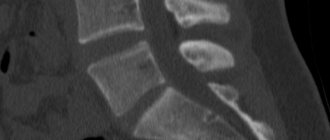
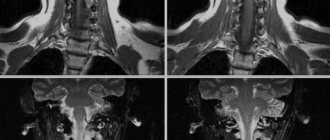
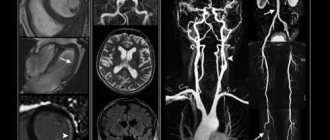
In this case, computed tomography can better diagnose such small, difficult-to-visualize abnormalities, and if you need to obtain information about the condition of soft tissues, then magnetic resonance imaging is the right choice.

The safest diagnostic method
Despite these features, radiography is widely used as a diagnostic measure, as it provides valuable information about the condition of the musculoskeletal system.
Radiography will be a valuable test for diagnosing osteochondrosis of the cervical spine, which is difficult to visualize without special techniques. This pathology is quite common because it is associated with sedentary work and physical inactivity. Using radiography of the spine, pathology can be diagnosed in a timely manner and treatment can begin.
Contraindications for X-ray diagnostics of the cervical spine
The procedure is not recommended for pregnant and lactating women and children under 14 years of age. Also, in the case of obesity (weight over 150 kg), the image will not be informative, and therefore the radiography procedure does not make sense. The situation is similar with patients who, due to some nervous disease, are unable to remain motionless for some time. However, the importance of correct and timely diagnosis is more important than the potential harm of radiation to the body. In the case of traditional film radiography of the neck, the average individual dose per procedure will be 0.3 mSv, and when using digital equipment - 0.03 mSv. It is believed that doses less than 0.1 mSv are insignificant and such values can be neglected.
Benefits of digital radiography
Thanks to the development of technology, it has become possible, using low-dose technology, to reduce radiation exposure by an average of 40%. The advantages of X-ray diagnostics using this technique are as follows:
- clarity of the resulting image (visualization of aggregations less than 1 mm);
- the ability to process images using special software;
- reduction of radiation exposure;
- concentration of the X-ray flux directly at the examined area;
- the ability to store images on digital media;
- efficiency of obtaining results
Contraindications
Research using a digital device has the advantage of being gentle on humans - the level of radiation exposure is so low that to exceed it you will need to take several hundred pictures in a short period of time. And yet there are situations when X-rays will be proposed to be replaced by other diagnostic methods. Relative contraindications for x-rays are:
- Pregnancy at any stage and breastfeeding pose a risk of disrupting the normal development of the fetus.
- Children's age 15 years.
In these cases, if it is necessary to take an x-ray of the cervical spine, it is performed at the discretion of the attending physician.
Also, a limitation for x-rays can be considered severe obesity (the information content of the image may not be large enough) and situations where, due to pain or mental disorders, the patient cannot remain motionless even while the image is being taken. In such cases, replacing x-rays with other diagnostic methods is considered.
Consequences of injuries and untimely treatment of cervical ailments
The consequences of injuries and advanced diseases of the cervical spine are very serious and sometimes fatal. A dangerous development of the disease can be compression of the spinal cord, leading to disruption of the musculoskeletal system, disorders of the nervous system, respiratory and cardiovascular systems, and sometimes even death. In any case, even minor injuries can cause cerebral circulatory disorders, blurred vision, tissue swelling, severe headaches, pressure surges, numbness of the upper extremities and other disturbances in the functioning of internal organs. Timely diagnosis and treatment of the cervical spine will not only save your health, but also help avoid disability and death.