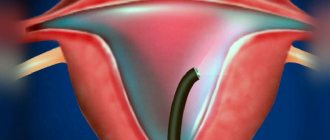
Hysteroresectoscopy (HRS) is a modern gynecological procedure that allows surgical treatment of the uterus without compromising the integrity of its wall. During treatment, laser or electrosurgical methods are used to remove tissue under visual control (i.e., using video systems that allow the surgeon to see the organ cavity throughout the entire course of the operation).
- Indications
- Contraindications
- Advantages and disadvantages of GDS
- Preoperative preparation
- Technique for performing GDS
- Postoperative recommendations
- Complications after hysteroresectoscopy
Indications
Hysteroresectoscopy is performed to treat pathological formations, altered tissues or developmental abnormalities of the uterine cavity. Indications for the procedure include:
- Submucosal (located under the mucous membrane) fibroids.
- Polyposis or some types of single polyps.
- Asherman's syndrome - intrauterine synechiae (adhesions).
- Endometrial hyperplasia in case of ineffectiveness of drug therapy or in the presence of contraindications to it.
- Menometrorrhagia (abnormally prolonged/heavy bleeding from the genital tract during menstruation). Surgical treatment is indicated in the absence of the effect of hormone therapy.
- A septum in the uterine cavity.
Since hysteroresectoscopy is an organ-saving operation, it is especially relevant in the treatment of patients of reproductive age.
What is hysteroresectoscopy?
Complex terms are always scary and raise a lot of questions. Let’s explain in simple terms: hysteroresectoscopy is a low-traumatic operation in the uterus. It completely preserves the organ itself and its reproductive function. The operation is performed through the vagina, without additional incisions.
Agree, there are not many operations in gynecology that are performed without a scalpel. This is the main advantage of hysteroresectoscopy. It is carried out almost bloodlessly, which means that rehabilitation is faster than with other forms of intervention. Hysteroresectoscopy is an extremely gentle operation that allows you to “point” eliminate the problem and not injure the surrounding tissue. This is especially important for women of reproductive age.
Contraindications
Hysteroresectoscopy is an invasive procedure, so it has a list of certain contraindications. This list includes:
- Acute or chronic inflammatory diseases of the genital organs (colpitis, endometritis, cervicitis and others).
- Narrowing of the cervical canal (for example, due to scar changes).
- Oncological diseases of the reproductive system in the last stages, metastases in the pelvic organs.
- Profuse uterine bleeding.
- Pregnancy.
- Infectious diseases.
With caution, hysteroresectoscopy is prescribed for heart defects, kidney pathology, blood clotting disorders, etc. Sometimes before the procedure, a woman is prescribed special training that can reduce risks.
Book a consultation 24 hours a day
+7+7+78
Advantages and disadvantages of GDS
Hysteroresectoscopy has a number of advantages over other endoscopic and open surgical interventions. This is due, in part, to the use of high-tech equipment that is used to perform it. Thus, video monitoring with high resolution quality, which accompanies the entire operation process, allows the surgeon to clearly see the size, shape and localization of pathological changes. Electrosurgical or laser instruments used during the procedure cause less tissue trauma compared to a conventional scalpel. The positive aspects also include the short duration of hysteroresectoscopy. Usually the operation lasts no more than an hour.
The disadvantages of the procedure include its limited capabilities. Some diseases cannot be eliminated using this method, so the surgeon will be forced to use alternative techniques. In addition, since hysteroresectoscopy is performed using high-tech equipment, it requires an experienced surgeon who is familiar with the operation of laser or electrosurgical instruments and endoscopic techniques to successfully perform it.

Preoperative preparation
Before performing hysteroresectoscopy, as with other surgical interventions, the patient must undergo a certain examination, which includes:
- General blood test, urine test, biochemical blood test, determination of the Rh factor, vaginal smears, Wasserman reaction, etc.
- ECG, chest x-ray, ultrasound of the pelvic organs.
- According to indications, consultations with other specialists are carried out.
The most favorable time for hysteroresectoscopy is the early phase of the menstrual cycle, so it is necessary to plan the operation for this period. In some cases, for the purpose of preparation, a woman is prescribed special hormonal drugs, for example, gonadotropin-releasing hormone agonists (GnRH agonists).
Immediately before the procedure, preparation of the gastrointestinal tract is necessary: the patient is prescribed a cleansing enema. Before surgery, food and water intake is prohibited.
Symptoms Symptoms of uterine fibroids include: pain in the lower abdomen, bleeding, various urination disorders, menstrual irregularities. With large fibroids, signs of anemia may appear (weakness, fatigue, dizziness). Submucous uterine fibroids most often manifest themselves in the form of uterine bleeding. B The multidisciplinary Clinic "Paracelsus" provides surgical treatment of all types of fibroids, through laparoscopic and laparotomy, resectoscopic removal of myomatous nodes with preservation of the uterus, as well as removal of the uterus using various approaches. The volume and access of surgical treatment is decided upon consultation with a gynecologist surgeon and is purely individual.
A myomectomy is a surgical procedure performed on the body of the uterus to remove a benign tumor (fibroid) from the muscular wall of the uterus. The operation involves the removal of fibromatous nodes, while the body of the uterus is preserved, and, accordingly, reproductive function is not impaired.
Hysteroresectoscopy is currently considered the most optimal method for removing myomatous submucosal nodes.
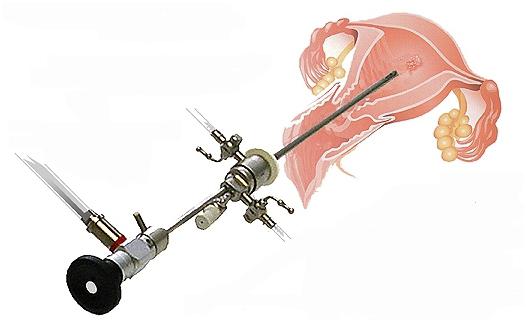
Resectoscopic myomectomy is performed using a hysteroresectoscope, a videoscopic device inserted into the uterine cavity, which has an additional channel for inserting an electrode. Through an electric wire, energy is supplied to the tip in the form of a loop, needle, or roller that captures and removes the myomatous node, while simultaneously coagulating the vessels.
Through a video camera, the image is transmitted to the monitor, and the gynecologist surgeon carries out all manipulations strictly under image control. Thus, the risk of complications is reduced to zero.
At the Paracelsus Multidisciplinary Clinic, a bipolar electrode is used to perform hysteroresectoscopic myomectomy, which eliminates the possibility of electrical injury to the patient, and makes it possible to perform these operations on patients with diabetes mellitus and a pacemaker.
Removal of a submucosal node can be performed simultaneously or in 2 stages. It depends on the nature of the node. Removing large fibroids in one intervention is the most risky choice, since in this case the walls of the uterus have deep and extensive damage, which can lead to severe bleeding. All removed tissue must be sent for histological examination.
The operation, performed in two stages, is recommended in cases where most of the fibroids are located in the wall of the uterus. At the first stage, part of the node is removed with preliminary hormonal preparation. Then, within 8 weeks, a second hormonal preparation is carried out and upon completion, the second stage of fibroid removal is carried out.
Indications:
- Reproductive dysfunction caused by submucosal nodes;
- The need to preserve fertility;
- Pathological bleeding from the uterus in the presence of a submucosal fibroid node.
You can undergo the entire scope of preoperative examination at the Paracelsus Multidisciplinary Clinic in one day! Examination for surgical intervention and validity period of examination results:
- colposcopy-12 months
- Ultrasound of the pelvic organs
- Ultrasound of the veins of the lower extremities – 3 months
- Ultrasound of the abdominal cavity, kidneys and bladder, retroperitoneal space
- Flora smear, bacteriological culture from the cervical canal -10 days
- oncocytology of the cervix – 6 months
- General urine test - 10 days,
- Fecal occult blood test - 10 days,
- Complete blood count and reticulocytes - 10 days,
- Electrocardiogram with interpretation -14 days,
- Blood for HIV, Hepatitis B, Hepatitis C, Syphilis 3 months.
- Biochemical blood test: general, direct, indirect Bilir., Total Protein, albumin, urea, glucose, creatinine, uric acid, AST, ALT, alkaline phosphatase, blood sodium and potassium, cholesterol, blood pH-10 days
- Coagulogram - 10 days
- Blood type and Rh factor
- Fluorography - 6 months.
- Consultation with a therapist, anesthesiologist and other specialists according to indications.
- Mammography -24 months (after 36 years), 12 months (after 50 years),
- Ultrasound of the mammary glands (up to 36 years) -12 months
Other examinations may be added as indicated. Anesthesia: These operations are performed under endotracheal anesthesia or spinal anesthesia. With this method of pain relief, the patient is completely relaxed. Pain after waking up is minimized by administering special medications. Contraindications to the operation are:
- The size of the uterine cavity is more than 10 centimeters;
- Combination of myomatous nodes and submucosal nodes with severe adenomyosis;
- Suspicion of leiosarcoma and endometrial cancer;
- Planned intervention is not performed for clinically significant blood clotting disorders, acute infections, decompensated somatic diseases (hypertension, unstable angina, severe diabetes mellitus, severe anemia).
After the operation, it is recommended to perform a control hysteroscopy two months later to confirm complete removal of the fibroids. Before this surgical intervention, the patient must see a gynecological surgeon. At the appointment, the doctor will explain in detail the essence of the procedure, alternative treatment methods and answer all the patient’s questions.
This procedure requires hospitalization in a hospital for 1 day. If necessary, a sick leave certificate is issued.
Technique for performing GDS
The method of pain relief during hysteroresectoscopy may vary. If a short-term intervention is expected, then intravenous anesthesia is used. Its action lasts for 30-40 minutes. If the operation promises to be long, then endotracheal (mask) or epidural anesthesia is used.

Immediately before surgery, the genitals and inner thighs are treated with antiseptic agents. In this case, the patient is in a gynecological chair. The surgeon dilates the cervix using special instruments, and then inserts the hysteroresectoscope into the uterine cavity. Next, a special liquid is injected that does not conduct current (usually a solution of glucose with sorbitol is used). Due to fluid pressure, the uterine cavity expands, which creates a good overview and the necessary space for various manipulations. Using a hysteroresectoscope, which displays an image on the screen, the surgeon carefully examines the uterine cavity, paying attention to its size, the relief and thickness of the mucous membrane, and the condition of the orifices of the fallopian tubes. The location, size and shape of altered tissues or pathological formations are carefully studied. After the necessary examination, they are excised using laser or electrosurgical instruments. The surgeon tries to remove the pathological focus as much as possible; often part of the normal tissue is captured, which helps avoid relapse of the disease.
How is hysteroresectoscopy performed?
When the price of the issue is health and the opportunity to have children, women for the most part decide to undergo any gynecological operations. But the unknown is always scary: what lies behind a complex medical term? How painful is it to have a hysteroresectoscopy? And what to expect from this procedure.
It's simple: manipulations are carried out under intravenous anesthesia, in the so-called medical sleep. An optical device with a microsurgical instrument - a hysteroresectoscope - is inserted into the uterine cavity. The doctor sees the image from the camera on the screen, identifies defects and eliminates them. The duration of the procedure is 15-40 minutes. After 3-4 hours the patient is discharged home.

Saddle-shaped uterine cavity after hysteroresectoscopy, dissection of the intrauterine septum
It’s hard to imagine, but every second woman has gynecological diseases. You should not be afraid of the problem - you need to look for its effective solution. Doctors of the University Clinic “I’m Healthy!” will come to the rescue. Would you like to make an appointment or find out the cost of hysteroresectoscopy? Don’t put off taking care of your health until tomorrow - call the number right now.
Postoperative recommendations
The rehabilitation period after hysteroresectoscopy always proceeds individually, depending on the goals and scope of the operation performed. However, there are several general points that are almost always noted:
- After surgery, the patient may feel moderate pain and discomfort in the lower abdomen. In order to eliminate these unpleasant sensations, the doctor will prescribe painkillers.
- Hysteroresectoscopy almost always causes damage to the endometrium. Sometimes it recovers on its own, but in some cases, to improve its regeneration, it is necessary to take estrogen medications. The average duration of the course is about three months, but according to the doctor’s recommendation it can be longer or shorter.
- In some cases, a woman is indicated for other specific treatment. The doctor will select the dosage of the drugs, the regimen and the duration of the course individually.
In general, rehabilitation after hysteroresectoscopy is calm and quick, especially if the operation was performed by an experienced doctor using modern equipment.
Complications after hysteroresectoscopy
Adverse consequences after surgery can occur for various reasons. All of them can be divided into three groups:
- Intraoperative (arising during surgery). These include bleeding and perforation (through damage) of the uterine wall.
- Electrosurgical. Burn tissue damage occurs when the technique of working with electrosurgical instruments is not followed.
- Postoperative. After hysteroresectoscopy, inflammatory lesions of the uterine walls, accumulation of blood in the uterine cavity, narrowing of the cervical canal, acute infectious processes, etc. may develop.
To avoid the development of complications after hysteroresectoscopy, careful preoperative preparation, a complete examination before surgery and individualization of tactics in each clinical case are necessary. The surgeon must have extensive experience in performing such interventions and have at his disposal all the necessary equipment and consumables.
Hysteroresectoscopy allows women to get rid of the disease, eliminate pain and restore the function of the reproductive system. For example, after removal of a uterine polyp, the menstrual cycle normalizes in 60-80% of patients, and in 30% of cases it is possible to restore a woman’s reproductive health. When treating uterine fibroids using hysteroresectoscopy, it is possible to restore reproductive function in 76% of those operated on. Therefore, this operation continues to remain relevant and is actively performed in the best medical institutions around the world.
Book a consultation 24 hours a day
+7+7+78
When should hysteroresectoscopy be done?
To try to understand the problem and get advice from a gynecologist, Moscow residents do not have to go to the clinic - just go online. But how accurate and useful will the information presented there be? Certified doctors of the University Clinic “I’m Healthy!”, professionals with many years of experience, consider the following pathologies to be indications for hysteroresectoscopy:
- endometrial polyps (including recurrent ones);
- submucous uterine fibroids;
- intrauterine synechiae (adhesions after previous surgical interventions or inflammatory diseases of the uterus);
- recurrent endometrial hyperplasia;
- remnants of the fertilized egg and placenta in the uterus after abortion or childbirth;
- malformations of the uterus (intrauterine septum)
- the need to remove an ingrown intrauterine device.
Quite often, hysteroresectoscopy is performed before an IVF program. So, for example, if you have an endometrial polyp, you can “cauterize” its “leg” without damaging the mucous membrane of the uterine cavity, which plays a huge role in embryo implantation. Or, in the presence of uterine fibroids, which deform the uterine cavity, leading to bleeding and infertility. With hysteroresectoscopy, it is possible to remove fibroids carefully and without incisions on the abdomen. And, if this is the only cause of infertility, in 60-70% of cases pregnancy occurs in the near future.

Endometrial polyp

Endometrial polyp

Endometrium (2nd phase of the menstrual cycle)

Normal endometrium (1st phase of the menstrual cycle)