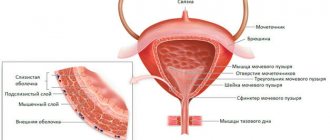
Before the advent of ultrasound diagnostics, the concept of “endometrial thickness” had no practical and diagnostic significance. Currently, it is a rare doctor who will prescribe treatment or give recommendations for the treatment of menopausal syndrome without having an ultrasound report. The endometrium is the inner lining of the uterus or mucous layer.
The mucous membrane of the uterus consists of 2 layers - basal and functional. The functional layer is a reflection of cyclic hormonal changes in the body of a woman of reproductive age. By being rejected every month with the arrival of menstruation, it signals that the bed prepared by nature for the future fetus was not useful and pregnancy did not occur. The cycle repeats again, from the cells of the basal layer a new endometrium grows and undergoes secretory changes, the thickness of which varies depending on the day of the menstrual cycle.
Endometrium in reproductive age
The menstrual cycle is usually divided into phases:
- desquamation or actual menstrual bleeding;
- proliferative;
- secretory.
In the proliferative and secretory phase, early, middle and late stages are distinguished. Each of them is characterized by its own endometrial thickness, and deviations from the average values indicate pathology of the inner layer of the uterus.
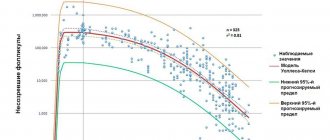
The thinnest mucosal layer is observed during menstruation. So, on the 2nd day of the cycle it is only 0.1-0.4 cm. Under the influence of estrogen hormones from the 5th to 7th day of the cycle in the early proliferative phase, this layer begins to thicken and amounts to 0.3-0.6 cm (average value 0.5). The same estrogens continue to increase it in the middle and late proliferative stages, lasting from 8 to 10 and 11 to 14 days, respectively. Endometrial thickness according to ultrasound is 0.5-1.0 (average 0.8 cm) and 0.7-1.4 (average 1.1 cm).
After ovulation, the secretory phase begins, and the inner layer of the uterus comes under the influence of progesterone. The inner lining of the uterus continues to thicken, sprouting vessels and glands in the early and middle secretory stages, which occupy days 15-18 and 19-23 of the cycle. The thickness of the endometrium is 1.0-1.6-1.8 cm (average 1.2-1.4). At the end of the middle secretory phase, the immersion of the fertilized egg should take place at maximum thickness. But, if this does not happen, the secretion of progesterone decreases and the mucosal layer in the late secretory stage on days 24-27 becomes slightly thinner, 1.0-1.7 (1.2 cm). Then, with a 28-day cycle, menstruation occurs.
How to do a pelvic ultrasound
Pelvic ultrasound in women is performed in two ways:
- Transabdominal method. The scanner sensor is placed on the anterior wall of the abdomen, while the patient's bladder should be full. The study can be carried out in any phase of the menstrual cycle, in virgins, and even during uterine bleeding.
- Transvaginal method. The scanner probe is inserted into the vagina. This method is more accurate, but is only used during a certain phase of the cycle. It is also contraindicated if you are allergic to latex, since the sensor is inserted in a condom.
Pelvic ultrasound during menstruation can only be done transabdominally.
Pathology of the mucous membrane of the uterine cavity
Deviations from average values can go in two directions. The endometrium may be thinner than it should be on a certain day of the cycle (hypoplasia), or its thickness may be greater than normal (hyperplasia). These changes can occur in small areas of the uterine cavity, and then we are talking about focal changes. If the changes affected the entire cavity, then this is diffuse hypo or hyperplasia. A pathologically thickened layer indicates a hormonal imbalance and in some cases requires diagnostic curettage of the uterine cavity followed by histological examination.
The causes of pathology of the inner layer of the uterus, in addition to hormonal imbalance, can be:
- disruption of the blood supply to the uterus;
- mechanical and hormonal trauma after abortion;
- inflammatory diseases of the uterus.
With glandular focal or diffuse hyperplasia, the thickness of the endometrium according to ultrasound reaches 2 cm, and with atypical hyperplasia, even up to 3 cm. Endometrial polyps are visualized on ultrasound in the form of formations from 0.5 to 6 cm. Changes in thickness and echogenicity are observed with endometrial cancer.
Age-related changes are physiological in nature. As a woman enters the postmenopausal period, cyclic hormonal secretion ceases, proliferative and secretory changes are absent, and the thickness of the endometrium decreases to 0.5 cm or less. Against this background, thickening up to 0.8 cm is considered critical and requires diagnostic curettage of the uterine cavity. With age, the risk of cancer pathology increases, especially if, after a long absence of menstruation, the patient experiences bleeding of varying intensity from the genital tract.
Why is it necessary?
Ultrasound detects various diseases:
- endometriosis is a pathology in which the endometrium extends beyond the uterus, penetrates the fallopian tubes and the abdominal cavity, and belongs to precancerous diseases;
- endometritis is an inflammatory process that can begin as a result of infections, abortion, diagnostic curettage, cesarean section, postpartum injuries;
- polyps - benign formations on a “pedicle”, which consist of endometrial cells;
- adenomyosis - cysts consisting of endometrial tissues that are localized in the muscular layer of the uterus;
- hypoplasia - thinning of the endometrium, which manifests itself as a result of poor blood supply or severe trauma during an abortion, which leads to miscarriage, since the embryo cannot implant in the uterus;
- hyperplasia - thickening of the endometrium caused by hormonal disorders; if untreated, cells may become malignant;
- tumors - to determine their nature (benign or malignant), a biopsy is done.
Endometrium during menopause
Endometrial hyperplasia often has no symptoms. If you have menstruation, when the body has not yet completely entered the menopause, there may be a cycle disruption. Most often, women during menopause notice bloody discharge. Sudden sharp pains during menopause are also typical.
During the postmenopausal period, the endometrium should be less than 4 millimeters. If the thickness is within 6-7 millimeters, laboratory tests are carried out within 6 months. If the thickness is more than 8 millimeters, the process is pathological.
Preparing for diagnosis
In order for ultrasound monitoring to be as effective as possible, several rules must be followed:
- for three days do not consume foods that cause increased gas formation;
- refrain from intimacy during the day;
- do not eat for 8-10 hours, as the diagnosis is carried out on an empty stomach;
- if necessary, take medications that reduce flatulence 2-3 hours before, or do a cleansing enema.
Before a transabdominal ultrasound, an hour before the procedure, you need to drink plenty of still water and not go to the toilet. When the bladder is full, the pelvic organs rise up and move closer to the abdominal cavity, which makes visualization easier. Before the transvaginal examination, you must empty your bladder.
Timing of ultrasound
The optimal timing for ultrasound should be selected depending on the purpose of the examination. The generally accepted periods are from 3-5 to 7-10 days from the start of menstruation.
To monitor the development of the follicle with a 28-day cycle, an ultrasound is performed on days 8-10, with a different cycle length - 4-5 days before the middle, with an irregular cycle - on days 3-5 after menstruation. Then, ultrasound is repeated every 2-3 days throughout the cycle, while simultaneously assessing the thickness of the endometrium using ultrasound.
Monitoring is recommended on days 9 and 25 of the cycle. When treating endometrial hyperplasia, control ultrasound is performed 3 and 6 months after the start of treatment. All examination results should be discussed with a gynecologist, who, if these parameters do not correspond to the duration of the menstrual cycle, will prescribe appropriate hormonal therapy.
When is it better to do an ultrasound for endometriosis?
Table of contents
- Indications
- Timing the Study
- Structural changes in the endometrium
- What will the ultrasound show?
- Types of disease
- Diagnostic methods
- Advantages of carrying out the procedure at MEDSI
Endometriosis is a disease of the female pelvic organs, which is characterized by a strong proliferation of tissues of the inner layer of the walls of the uterus into other structures (outside the boundaries of this organ). These cells travel to the ovaries, vagina, and other areas through the fallopian tubes, blood, and other means. Cysts can form from them, which will lead to disturbances in the functioning of the genitourinary system.
Indications
The symptoms of this disease often coincide with signs of other ailments of the genitourinary system. In some cases, it may not appear at all, or the woman may not pay attention to the symptoms, considering them unimportant or normal. Therefore, you should consult a doctor if the following phenomena are recorded:
- Long and painful menstruation
- Presence of dark-colored discharge for several days before or after menstruation
- The presence of discomfort during sexual intercourse
- Unstable cycle
- Painful urination
- Infertility
- Weakness, frequent dizziness, fatigue, skin defects
- Elevated temperature for a long time
Timing the Study
A pelvic ultrasound for endometriosis is often not enough. But this type of examination can also be useful if it is carried out at the right time.
To diagnose other diseases - fibroids and the like - it is recommended to do an ultrasound examination in the first week after the end of menstruation (from the fifth to the seventh day), when the tissues of the intrauterine layer are thinnest.
In the case of endometriosis, this principle does not work, since its formations are best visible when the inner layer of the uterine walls is thickest. Therefore, for the best result, it is necessary to do this examination from the twenty-fifth to the twenty-eighth day, if the woman’s cycle is thirty days. During this period, the endometrium becomes thickest, and, accordingly, foci of the disease grow.
Since it is not always possible to unambiguously determine the presence of this disease, it is recommended to undergo an ultrasound scan during several menstrual cycles and preferably on the same cycle days. This helps to identify signs characteristic of such a disease.
Structural changes in the endometrium
There are three main stages of changes in the state of the inner layer of the uterine walls, which are divided into several shorter mini-stages:
- First:
- Menstruation period - the thickness of the endometrium is minimal, but a number of areas may be hyperechoic
- Days five to seven – a thin layer of the endometrium up to seven millimeters thick, with low echogenicity
- Eighth to tenth days – thickness increases to ten millimeters
- Eleventh to fourteenth days – the layer grows to fifteen millimeters
- Days fifteen to eighteen – echogenicity increases, the layer reaches seventeen millimeters
- Days nineteen to twenty-four – the membrane thickens, echogenicity increases, and the tissue structure becomes heterogeneous
- Twenty-fourth to twenty-eighth days - thickness may decrease to 11-17 mm, echogenicity and structure remain the same
What will the ultrasound show?
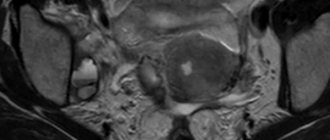
Endometriosis is not always obvious on a pelvic ultrasound, but ultrasound helps determine its presence based on certain signs:
- Presence of endometrial cells in the perineum, vagina and external genitalia
- Presence of formations on the cervix
- Enlargement of the uterus, change in its shape (becomes spherical)
- Presence of cysts in the ovaries
- Thickening of organ walls
If the focus of the disease is in the ovaries, then the examination will show that:
- The tissues contain various types of nodular inclusions
- There is a round mass behind or to the side of the uterus
- Tissue heterogeneity
If the disease is localized in the uterus, then ultrasound will reveal the following changes:
- Blurred endometrial tissue
- Asymmetry of the uterine walls
- Presence of nodules
Types of disease
As endometriosis grows, its four degrees are determined:
- The first is point propagation
- Second, the lesions gradually grow
- Third - cysts form, which gradually increase in size
- Fourth – extensive damage to organs and tissues
There is also a classification according to its localization:
- Internal - lesions in the uterus and its cervix
- External - endometrial cells in the abdominal cavity, vagina, ovaries, etc.
The types of disease are distinguished according to the shape and structure of the tumors:
- Focal - a cyst with increased echogenicity up to 16 mm in size, the uterine walls are asymmetrical
- Nodular - round neoplasms up to 30 mm in size, without clear outlines and localized in a specific organ
- Diffuse - the uterus acquires a rounded outline with calcium inclusions, its inner layer has vague boundaries, the posterior wall is enlarged, and the echogenicity is increased
Diagnostic methods
A pelvic ultrasound can detect endometriosis, but doctors recommend undergoing several types of examinations to ensure the most accurate diagnosis.
To determine the presence of this disease, the following types of ultrasound examinations are used:
- Abdominal – carried out by a sensor through the wall of the abdominal cavity
- Transvaginal – examination by inserting a sensor into the vagina
- Transrectal - with this type, the device is placed in the patient’s anus
To more accurately identify the type of neoplasm, the second and third types of examination are more suitable. They also allow you to take tissue samples for analysis.
As an additional method of clarifying the diagnosis, colposcopy (examination of the vagina and cervix using a device that includes a binocular) can be used.
Advantages of carrying out the procedure at MEDSI
- MEDSI clinics are equipped with modern devices Pro Focus 2202, Philips iU22 for conducting thirty types of ultrasound
- Doctors of the highest qualification category will prescribe all the necessary types of examinations, interpret the results qualitatively and make an accurate diagnosis
- To get a consultation, you just need to call 8 (495) 7-800-500, and you will be given an appointment at a time and place convenient for you - MEDSI has a network of more than twenty clinics
- It is always possible to conduct an urgent examination in the event of bleeding or other emergency situations.
Indications and contraindications
An endometrial ultrasound is necessary when:
- the duration of menstruation is less than 3 and more than 7 days;
- intermenstrual bleeding;
- delay of menstruation for more than three weeks;
- irregular menstrual cycle;
- pain in the lower abdomen not associated with menstruation;
- pain and discomfort during intimacy;
- inflammatory processes in the uterus;
- hormonal imbalances;
- inability to become pregnant for more than a year with regular sexual activity without the use of contraceptives;
- spontaneous termination of pregnancy;
- the need to assess the condition of the mucous membrane after abortion, cesarean section, diagnostic curettage.
It is also recommended to undergo diagnostics annually for preventive purposes.
There are no contraindications to transabdominal ultrasound. Transvaginal diagnosis is not performed on virgins and pregnant women in the second and third trimester, as well as in the presence of infectious diseases of the genitourinary system.
In the specialized clinic of urology and gynecology Uclinica, highly qualified specialists with many years of experience practice. In their work they use modern equipment of the latest generation with high resolution. It allows you to detect even the slightest changes in the structure of the endometrium. Thanks to timely diagnosis, Uclinica doctors are able to successfully cope with various diseases.
You can sign up for ultrasound monitoring of the endometrium by calling +7 or using the online form.
Contact a specialist:
| Ultrasound monitoring of the endometrium | 1000 rub. |
Go to Contacts Make an appointment