It would be very prudent on the part of the parents to leave with a small amount of time (registration, traffic jams on the road, adaptation to unfamiliar conditions, etc.).
The duration of stay in the clinic is from 1 to 24 hours.
The administrator will meet you at the reception. You will have time to change your shoes and take off your outerwear (if it is the cold season).
While your child gets used to an unfamiliar environment and plays in a specially equipped corner, you can fill out the necessary papers.
Documents you need to bring with you to the clinic:
- Birth certificate or passport of the child, passport of one of the parents - for registration.
- Medical documentation for the doctor who will decipher: previous EEG/video-EEG monitoring studies: conclusions and printouts of the EEG recording, if available - recording on disk or other electronic media; MRI and/or CT reports and images/discs; extracts from hospitals and/or conclusions of the attending physician (neurologist, epileptologist), data from genetic studies.
After completing the paperwork, you will be taken to a soundproofed room where video-EEG monitoring will be carried out.
Who conducts video-EEG monitoring
In our clinic, the study itself (video-EEG monitoring) is carried out by EEG assistants - highly qualified specialists who have special training. These are senior year medical students planning to study neurology and/or functional diagnostics (FD), neurology and FD residents, neurologists and FD doctors.
During the study, the EEG assistant will be located nearby in the next room - the assistant's room. He will monitor the patient through a monitor.
The EEG assistant will collect anamnesis, ask questions about the medications taken, complaints, how the disease is progressing, ask if there are currently seizures and whether they could occur during the period of the current study, talk about how the study is carried out (time frame, time of testing, sleep/wakefulness) and what needs to be done.
Before starting the study, you must remove all metal objects, jewelry, earrings, hairpins, and elastic bands from your head. The braids must be unbraided. Neck jewelry, chains, and crosses can be left on; they do not affect the results of the study.
The child will be seated facing the TV screen and will be offered to turn on their choice of cartoons or leave a channel on the TV. There is a video camera above the TV screen. Parents need to sit facing the child, but slightly to the side so as not to block him from the camera
The child must always be in the frame facing the camera; the child must not be blocked from the camera. They will show you how to bypass the camera.
It is necessary, during the entire study (while awake and while asleep). This is necessary for the interpretation of normal EEG rhythms and, especially, in the event of an attack: often the most important thing for the correct interpretation of an attack is how the eyes behave at the beginning of the attack, in addition, attacks can often be clearly differentiated only by the movements of the eyeballs and eyelids, often attacks are manifested only by movements of the eyeballs and eyelids).
To choose the optimal hat size, the child’s head volume will be measured. Then disposable electrodes will be glued: two behind the ears, one cardiac on the heart area and two myographic on the shoulders. Then they will put on a chest belt, an electrode cap with a tail of electrode wires and secure it to the chest belt with straps crosswise. The electrodes are connected to an electroencephalograph. The device allows you to enhance the biopotentials of the brain transmitted from sensors several hundred thousand times.
The international electrode arrangement system is used: 10-20.
The electrode cap has 20 electrodes built into it, in the center of which there is a hole where the EEG assistant will fill the gel with special syringes.
You will be given a patient button and a sheet to mark paroxysmal conditions.
The button should only be pressed when you see the child having an epileptic seizure (or what the parents or their doctor think is an epileptic seizure).
The time and description of the attack must be recorded on the sheet for marking paroxysmal states.
The child should not be covered with a blanket, because Arms and legs should be visible.
When everything is prepared, video-EEG monitoring begins recording. First, active wakefulness is recorded, the child is asked to sit quietly with his eyes open, and is allowed to watch cartoons. Next, a recording of passive wakefulness is carried out - you need to sit with your eyes closed; if necessary, the recording of passive wakefulness is carried out while lying down (This is necessary to record the main rhythm of wakefulness - the alpha rhythm).
Our functional diagnostics specialists:
1. Dorofeeva Natalya Evgenievna.
Candidate of Medical Sciences, neurologist, epileptologist at EpiJay Clinic. Functional diagnostics doctor. 2. Zgoda Viktor Nikolaevich. Neurologist, epileptologist at EpiJay Clinic. Functional diagnostics doctor.
3. Lvov Viktor Sergeevich. Functional diagnostics doctor at EpiJay Clinic.
4. Shin Svetlana Vladimirovna. Functional diagnostics doctor at EpiJay Clinic.
Pathological activity that does not occur during the daytime is often activated by sleep. Many pathological discharges increase during sleep, and it becomes clear how dangerous they can be (or not), both in terms of the risk of epileptic seizures and in terms of possible risks to the child's development.
At the same time, interpretation of EEG during sleep is very difficult and requires highly qualified researchers. Particularly in children, there are a number of variations in sleep EEG that are very similar to epileptiform discharges but are normal at certain ages.
When is video-EEG monitoring necessary?
- When diagnosing epilepsy and to assess the effectiveness of therapy.
- Before and during the withdrawal of antiepileptic therapy that was prescribed for epilepsy, neonatal seizures or as a preventive treatment after severe traumatic brain injury.
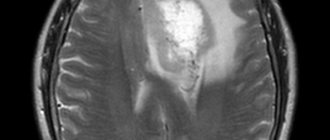
- Preparation for surgical treatment of epilepsy, when very precise localization of the lesion is necessary to decide on the extent of surgical intervention. In this case, VEM data must be consistent with the results of other methods: MRI, PET, magnetoencephalography.
- Any unclear conditions during sleep that require a differential diagnosis with epilepsy: sleepwalking, nightmares, night dystonia, night migraines and others.
- Any paroxysmal conditions that occur during wakefulness (fainting, shuddering, dystonic attacks, unclear freezing - “thoughts”) that require a differential diagnosis with epilepsy in the absence of pathological activity during the EEG of wakefulness.
- Regression of speech and mental development. If a child developed normally for some time, and then, for no apparent reason (trauma, encephalitis), stopped developing or even lost previously acquired skills, video EEG monitoring is extremely necessary, even if he has never had seizures.
In addition to the above, there are conditions (for example, Landau-Kleffner syndrome) in which epileptic activity that occurs during sleep may manifest itself not as seizures (or not only seizures), but as loss of speech and disintegration of mental abilities. In this case, only timely treatment can save the child from irreversible lifelong consequences.
The diagnosis cannot be established without VEM.
Contraindications to video-EEG monitoring
An absolute contraindication is only the technical impossibility of conducting the study; for example, in the case of traumatic or inflammatory head injuries. The duration of VEM ranges from 1 hour to several days.
A relative contraindication may be the child’s high excitability or aggressiveness.
How to prepare for video-EEG monitoring
In the case of daytime monitoring in the evening, you need to go to bed early and wake up several hours earlier than usual (the morning time, what time you need to get up is variable - parents can often more accurately say how early their child needs to be woken up so that he wants to fall asleep in the morning/afternoon) . Before the study, you should not drink caffeine/tannin containing drinks. The head must be clean; you cannot use hairspray, foam, or wax. It is necessary to have warm clothes, since it is impossible to sleep tightly covered with a blanket. Parents need to prepare in advance their favorite books and toys that can distract and occupy the child during the study. It is also necessary to explain to the child the day before why he is going to the clinic and what the procedure will look like; it is useful to watch a video about the preparation and conduct of the study.
Why is it better to do video monitoring in our clinic?
- The office in which research is carried out is equipped with soundproofing and darkened windows. In addition, in addition to a comfortable bed for research, there are sofas on which the child’s parents can sit.
- Most of the doctors performing and interpreting the studies are practicing neurologists-epileptologists, candidates of medical sciences.
- The research uses the latest equipment from Mizar, the configuration of which was custom-made for the EpiJay clinic.
- Each study is performed with an individual approach for each patient, taking into account his medical history and needs. For example, it is often necessary to artificially induce seizures using noise or conduct a test while the patient is waking up. Our doctors are ready for any research.
- Possibility of on-site research at your home.
- After the examination, a conclusion with a diagnosis is issued. Urgent decryption is possible.
Video-EEG monitoring at home
In some cases, it is difficult to carry out the study in the clinic. For example, with behavioral disorders, neuroses, or autism, it will be difficult for a child to sleep in a hospital. In these cases, home testing is used.
This study is psychologically better tolerated by both parents and the child himself. Everyone sleeps in their usual beds, remains in their usual routine. Thus, research at home is the most gentle for the child.
Expert video-EEG monitoring study
Currently, surgical treatment of epilepsy is gaining momentum. At the moment, this is the only method that, in case of a positive outcome, often allows for a complete cure of epilepsy. Surgical treatment is usually indicated for structural epilepsy, when focal changes are clearly identified on MRI.
In the case of resistant (that is, when antiepileptic drugs did not work after 2-3 attempts to prescribe them) epilepsy, surgical treatment can be considered as a possible method of choice in the absence of focal changes. The result of the operation directly depends on how accurately the boundaries of the epileptic focus are established.
Sometimes the localization and boundaries of the structural focus (visible during an MRI study) and the epileptogenic focus do not coincide. To avoid irreparable errors during surgery, it is important to achieve extreme accuracy in determining the place from which epileptic discharges emanate during an attack. Unfortunately, the sources of epileptic discharges during a seizure and on the interictal EEG may also not be the same, so it is most important when planning surgical treatment of epilepsy to record the EEG during a seizure (“ictal”) EEG. In this case, of course, it is necessary to plan a longer recording – sometimes up to several days. If the recording of an “attack” EEG is carried out on high-tech expert-class equipment with an increased number of electrodes, then the accuracy of localization of the lesion boundaries increases, and, consequently, the postoperative prognosis improves, the number of positive postoperative outcomes and the number of patients completely cured of epilepsy increases.
Decoding and delivery of video-EEG study results
Since video-EEG monitoring is a long-term study (recording lasts at least 1.5-2 hours), it is not possible to immediately issue a conclusion and printout. The turnaround time for the conclusion with decoding and printing is 2-3 business days. At the same time, sometimes urgent decoding of video-EEG monitoring is required, which is especially important for out-of-town patients. For such a case, we have provided. When recording video EEG monitoring, it is important to immediately stipulate the need for such urgent decoding, since, for example, during the holidays (or for a number of other reasons) it is not every day possible to provide you with this service.
Decoding of video EEG monitoring is carried out within 2-3 working days
Samples
30 minutes after the start of the study (and 30 minutes before its end), functional tests are carried out - “provocations” of epileptic activity and convulsive seizures.
- The patient sits on a chair calmly, relaxed, with his eyes closed, and does not speak for 3-5 minutes.
- Eye opening-closing test (the patient is asked to open his eyes, close them after 5-10 seconds, repeat three times).
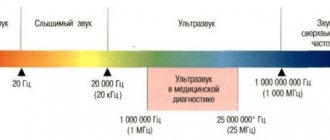
- RPS test (Rhythmic photostimulation) - flashes of light of various frequencies. It is carried out to identify “photosensitivity” - a predisposition to epileptic seizures when exposed to flickering light, such as a TV: carried out with eyes closed (if possible).
- Eye opening-closing test.
- Test with hyperventilation (forced deep breathing) The patient is asked to breathe deeply and deeply for 3 minutes, then breathe calmly for 1 minute.
- Eye opening-closing test.
- If the child does not perceive the addressed speech and does not follow commands, only tests with RFS are carried out.
While awake, the patient can do everyday activities: read books, watch movies, listen to music, eat, if necessary, visit the toilet, etc.
Stages of the IDVNE study
Day and night video monitoring is carried out in a special cap. Multi-day - by attaching cup electrodes. First, markings are made on the skull to specify the zones. The advantage of cup electrodes over a cap is that they are comfortable and do not require the supervision of assistants. The encephalogram is cleaner, written more consistently, with fewer artifacts that can complicate the analysis of seizures.
Before the procedure begins, tests of photostimulation and hyperventilation are carried out in an increased mode. The changing behavior of the patient depending on the type of activity is taken into account to introduce load parameters. Based on the initial examination and the clinical picture of complaints, the doctor chooses the duration. Sometimes the ability to fall asleep during the day is affected. If localization is suspected in different places, a daily examination may be recommended. The main condition is a stationary position so that the encephalogram is not distorted.
Dream
- The patient goes to bed only when he wants to.
- Functional tests are performed 30 minutes before the end of the study.
- After video-EEG monitoring is completed, the cap or electrodes are removed. You can go home.
Research is carried out around the clock, seven days a week, and there are 2 video-EEG monitoring chambers. In the wards, in addition to an extra bed for your mother, you will have a microwave, refrigerator, electric kettle, and dishes at your disposal. You need to bring food, pajamas, and slippers with you. Do not forget that covering your child with a blanket while sleeping during the study is highly undesirable. The rooms are well heated; each room has an additional heater. During the study, the child can move freely around the room, watch videos (cartoons and children's films from our collection, or you can bring your own recordings to watch on a flash drive or disk).
To conduct daytime video-EEG monitoring, an electrode cap is placed on the patient’s head. When conducting overnight and 24-hour video-EEG monitoring, the patient is wearing a cap or glued collodion electrodes, depending on a number of factors.
Night EEG results for children (transcript)
Highly qualified specialists with extensive clinical experience are involved in deciphering children's night video-EEG. A professional epileptologist examines the received materials and gives a detailed answer, practical recommendations, and, if necessary, refers for additional treatment to specialized hospitals. The more accurately the source of the disease is identified, the greater the chances of effective treatment of the disease. Treatment of nocturnal epilepsy, which statistically affects about 30% of patients, is possible through the use of anticonvulsant medications. In addition, it may turn out that the seizures are not caused by epilepsy, but by third-party problems, physical or emotional, that will require other treatment.
The decryption process takes just over a week. You can receive the conclusion remotely or in person. After a week, you will be given a professional conclusion and a recording disc on which the most significant stages of monitoring are recorded. If you require a more immediate response, we are ready to help with that too.
Gluing collodion electrodes
Gluing is carried out with 22 electrodes (1 of which is grounding and 2 reference electrodes) according to the “ten-twenty” scheme.
For gluing, medical glue (collodion) is used, which has a specific smell.
Advantages of gluing: the electrodes on the head are thin, do not cause discomfort during sleep, and fit firmly to the head, which eliminates the presence of artifacts in the recording.
Disadvantages of gluing: the smell of collodion, duration - approximately 40 minutes.
Is special training needed?
There is no need to prepare specially, but it is recommended to carry out classic preparatory measures:
- Wash your hair. Do not apply to hair and scalp after washing mask, cream, foam. Fat acts as a dielectric and distorts data.
- Arrive sleep-deprived. Go to bed later at night and get up earlier in the morning. This is necessary to ensure that the patient falls asleep during the daytime examination.
- If you are afraid, then carry out psychological correction of behavior, relax, listen to calm music, talk with people who have undergone the procedure.
- Remove jewelry, elastic bands, and hair clips. Remove earrings and chains from your neck.
- Don't wear makeup.
- The day before the procedure, exclude all substances that stimulate the nervous system. Do not drink alcoholic or low-alcohol drinks, energy drinks, or coffee.
- Stop smoking in 3 hours.
The conclusion is issued in 5-7 working days. If you need urgent results within 24 hours, call or come in person.
Electrode Cap
To conduct video-EEG monitoring, a cap is placed on the patient’s head, on which electrodes are placed to record electrical impulses from the brain. The cap is made of elastic spandex type fabric with clean tin electrodes recessed into it. The international standard for electrode placement is 10-20. A conductive gel is applied under the cap to improve signal reception. Depending on the size of the head, the cap is selected individually. To prevent the cap from falling off, the doctor fixes the fasteners and additional fasteners to prevent the electrodes from moving. The patient wears a cap during the entire EEG monitoring.
Reason for appointment
Video-EEG is prescribed for diagnostic purposes in diseases with seizures. Will show the cause of neuralgia - epileptic, non-epileptic, focal, generalized type. It will reveal the peculiarity, type of form, source of occurrence. The reasons are:
- Convulsive surges that suddenly appeared and had never happened before.
- Paroxysmal conditions of unknown origin.
- Behavioral and cognitive disorders that progress from childhood to adulthood.
- The need for a complete examination in the preoperative period during anticonvulsant therapy.
- Neuralgia before AED withdrawal.
- The need to determine the type of coma and confirm brain death.
In cases of spasmodic seizures of unknown etiology, disturbances of consciousness (including premenstrual days), sudden or periodic fainting, disturbed sleep, headaches, dizziness, we recommend seeking advice from IDVNE specialists.
Our doctors
GENERALOV Vasily Olegovich
Head of the center, Doctor of Medical Sciences
SADIKOV Timur Ruslanovich
Candidate of Medical Sciences, doctor, neurologist, epileptologist
KAZAKOVA Yulia Vladimirovna
Doctor, neurologist, epileptologist
TYUMENKOVA Galina Viktorovna
Candidate of Medical Sciences, psychiatrist-psychotherapist
Timonina Oksana Vasilievna
Administrator, manager's assistant
YUGAY Anton Meliksovich
Doctor, neurologist, epileptologist
OREKHOV Andrey Borisovich
Neurologist
MOKHOVA Galina Aleksandrovna
Neurologist
DEMIDOVA Ekaterina Yurievna
Neurologist
Zenkov Semen Sergeevich
Neurologist
MOROZOV Nikolay Pavlovich
Neurologist