Full text of the article:
Esophagogastroscopy
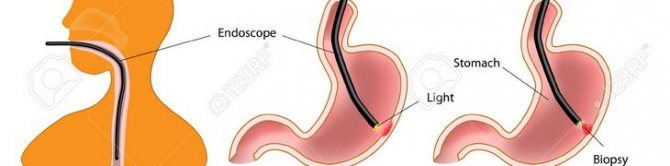
(from Latin-Greek, where oesophagus - esophagus gaster - stomach, duodenum duodenum, skopeo - look) - a type of endoscopic highly specialized examination of the upper gastrointestinal tract (esophagus, stomach, duodenum) using a flexible endoscope. Endoscopy is performed for diagnostic and therapeutic purposes. The unique optical capabilities of the device allow you not only to examine all areas of the mucous membrane of the diseased organ, to examine the pitting and vascular pattern, but also to take photos and videos of it.
This procedure allows you to study the condition of the organs of the upper gastrointestinal tract in one go, and if necessary, makes it possible to carry out additional diagnostic (test for Helicobacter pylori, chromoscopy, acidity determination, manometry) and therapeutic manipulations (stop bleeding, perform blood sampling). piece of tissue for histological examination and remove neoplasms).
How is gastroscopy (esophagogastroduodenoscopy) performed?
To conduct the examination with the greatest information content, it is important to know how to prepare for the gastric endoscopy procedure:
- To reduce the manifestations of the gag reflex, the patient’s mouth and throat are treated with a solution for local anesthesia (usually lidocaine spray 10%). In exceptional cases, anesthesia is necessary;
- The patient should lie in a left lateral position with knees bent and relaxed;
- Remove dentures from the oral cavity, remove piercings
- The nurse will install a special mouthpiece/guide that you will clamp between your teeth or gums; it is needed to make it easier for you not to “close” your mouth during the procedure and will protect the expensive endoscope from damage during the examination
- For better visualization and smoothing out all wrinkles, a small amount of air or carbon dioxide is introduced through the endoscope.
What affects the time of gastroscopy?
Despite the fact that the average duration of an endoscopic examination of the stomach is 5-10 minutes, this period can be extended under the influence of several internal and external factors.
Among them:
- Psychological mood
. Most patients (especially those undergoing this examination for the first time) associate endoscopy with painful sensations. This creates a persistent fear in them, which negatively affects the formation of contact with the doctor. - Failure to comply with proper preparation
. If the patient did not adhere to the diet and consumed any food within a few hours or minutes, performing an FGDS may be difficult or even canceled. In this situation, active digestion of incoming food will occur in the stomach cavity, as a result of which it becomes impossible to assess the condition of the walls of the organ. - Use of anesthesia
. As mentioned above, if there are indications or personal desire, endoscopic examination of the stomach is possible under local or general anesthesia. This will require the involvement of an anesthesiologist, who individually selects the optimal drug and its dosage.
How is the endoscopy procedure performed?
During esophagogastroduodenoscopy, a thin flexible endoscope tube with an optical system (video camera) at the end is gradually guided from the mouth of the esophagus to the initial parts of the small intestine. Endoscopes equipped with a fiber optic system and lens transmit the image to an online monitor, which allows the doctor to immediately diagnose the condition of the subject. Then carefully remove the device.
Capsule gastroscopy differs in that instead of a probe, the patient swallows a plastic capsule containing a video camera (after 8 to 15 hours it is removed from the body naturally during bowel movements).
The duration of the procedure is determined individually. With local anesthesia, the procedure takes 7-10 minutes
.
With general anesthesia, the examination lasts about 30 minutes
.
IMPORTANT!
After endoscopy of the esophagus and stomach, it is not recommended to drink or eat for 30 minutes. After anesthesia/sedation, refrain from driving on this day.
Why “swallowing the gut” is the only way to recognize stomach cancer in time
Stomach cancer ranks fourth among the types of oncology most common in the Voronezh region. According to the Voronezh Regional Oncology Center, it is second only to skin cancer, lung cancer and breast cancer. At the same time, according to the World Health Organization (WHO), stomach cancer ranks third in the world in the structure of causes of death from cancer.
Despite the difficulty of treatment, if gastric cancer is diagnosed early, the patient has every chance of beating this disease thanks to the capabilities of modern medicine. If this type of oncology is detected at the zero or first stage, the survival rate of patients reaches 90%.
In the case of stomach cancer, fibrogastroscopy (FGS) - an examination of the upper gastrointestinal tract - plays a key role in early diagnosis. We talked with Voronezh oncologists and specialists from the Voronezh Regional Clinical Center for Public Health and Medical Prevention about in what cases it is necessary to resort to this procedure and why FGS is perhaps the only effective method for early diagnosis of stomach cancer.
Who needs to “swallow guts” and when?
The FGS procedure involves the insertion of a gastroscope (a long thin elastic tube with special optics at the end) through the patient’s mouth into the esophagus and stomach (and in the case of fibrogastroduodenoscopy (EGD) - into the duodenum).
When it comes to fibrogastroscopy, or, as people say, the need to “swallow the gut,” the imagination of many paints terrible pictures of a painful procedure, which should be resorted to only when all other diagnostic methods have been exhausted. Most often they are based on stereotypes dating back to Soviet times.
Oncologists and gastroenterologists strongly recommend that those who have chronic stomach problems undergo FGS regularly and as planned. And after 40 years, everyone, without exception, should do this procedure at least once a year, even if there are no complaints about the gastrointestinal tract.
The attending physician (therapist, gastroenterologist) may prescribe FGS for the following patient complaints: prolonged epigastric pain (in the abdomen); heartburn, belching, nausea and vomiting; difficulty swallowing food; lack of appetite; sudden weight loss; hemoptysis, etc.
Why is FGS the most effective method for early diagnosis of stomach cancer?
The fact is that many stomach problems, including those that can lead to cancer, cannot be detected at an early stage by any other diagnostic method other than FGS.
During gastroscopy, the doctor sees the condition of the tissues of the esophagus and stomach on the screen in real time in great detail and can notice the slightest pathological changes (which cannot be seen either with ultrasound or tomography).
The insidiousness of stomach cancer is that in the early stages it often occurs without any clinical manifestations. The first symptoms begin to develop, as a rule, already with a tumor of the second or third stage, when, as they say, it is already too late to drink Borjomi.
Only with the help of FGS can one reliably and accurately identify the first signs of precancerous processes in the initial parts of the digestive system. Precancerous diseases are diseases that over time can turn into cancer or on their background often develop oncology. In the case of the stomach, such diseases include primarily chronic atrophic gastritis, adenomatous polyps and peptic ulcers.
Another advantage of FGS in diagnosing cancer is that with the help of a gastroscope you can not only visualize areas of the gastric mucosa, but also, if necessary, perform a biopsy (that is, take a tiny piece of biomaterial for subsequent laboratory testing).
Modern gastroscopes are capable of not only diagnosing, but also carrying out therapeutic procedures, which in some cases make it possible to avoid serious surgical intervention. For example, with the help of gastroscopy, you can remove polyps (a potential threat of cancer) or perform bougienage - widening the narrowed esophagus and restoring its patency.
Is it true that FGS is extremely unpleasant and painful?
Yes, of course, the FGS procedure cannot be called pleasant. Although the patient does not experience any pain. Only some discomfort associated, for example, with regurgitation of air during the examination. But modern medical equipment, coupled with anesthesia (including the possibility of medicated sleep), allows us to minimize the discomfort and time of this procedure.
Agree, it is better to wait a few minutes than to end up under the knife of an oncologist. After all, as you know, currently the main and practically the only method of radical treatment for stomach cancer is surgery.
Read about the first symptoms, risk factors for stomach cancer, as well as how to eat properly and what lifestyle you need to lead to prevent this type of cancer in our previous material. Active link - https://moe-online.ru/news/byd-v-kurse/1066445
How to prepare for gastroscopy?
Before undergoing gastroscopy, you need to follow some recommendations. It is advisable, first of all, to consult a specialist (gastroenterologist):
- Based on your medical history, he will determine indications or contraindications for gastric endoscopy. If necessary, he will prescribe additional tests for FGDS;
- Determine the type of anesthesia based on the patient’s response to certain medications;
- The doctor will find out bad habits that may affect the outcome of the endoscopy;
- Prescribe a diet before the procedure;
- The doctor will warn you about symptoms that may occur after the procedure;
- Will answer all your questions (for example, does it hurt).
Two to three days before the procedure, you should not eat spicy foods, smoked or fried foods. But lean meat, steamed, light soups with vegetable broths and porridges, on the contrary, are welcome. The bread should be slightly dry.
On the day of gastroscopy, if the procedure is scheduled for the first part of the day, you should not eat. And if in the second half of the day, then you can allow yourself a light breakfast (well-cooked porridge or cottage cheese is optimal for this), but no later than 8-10 hours before the test.
Particular attention should be paid to the drinking regime! Drinking is prohibited before the examination. And during preparation, alcohol, soda and coffee are excluded.
Duration of the procedure?
FGDS is done after special preliminary preparation, including diet, giving up bad habits and stopping taking certain medications. As a rule, it is necessary to adhere to these preparatory measures several days before the scheduled day of the diagnostic procedure. This is a mandatory measure to obtain the most informative and accurate data. If we talk directly about gastroscopy, then its duration is approximately 5-10 minutes. This medical procedure is carried out exclusively by a qualified diagnostician in a specially equipped office with the necessary amount of endoscopic equipment.
This time is enough to assess the condition of the esophagus and gastric wall. If it is necessary to perform a biopsy (taking biomaterial for further microscopic examination) or obtain images, the duration of diagnosis may increase. Since FGDS involves swallowing and further advancement of the probe, some patients may experience discomfort and activation of the gag reflex. To prevent unwanted effects or pain, local anesthesia may be used. Taking into account pain relief, the procedure takes about 15-20 minutes.
.
What are the possible complications of gastroscopy?
If a Doctor prescribed a gastroscopy for you, then he analyzed your state of health and believes that with your state of health, the risks of complications are minimal (i.e., heart attack, stroke, and other serious “general” negative manifestations that can be provoked by the study are excluded)
Directly from the procedure itself, complications are extremely rare; possible complications during endoscopy of the stomach and duodenum include perforation (perforation) of organ walls and bleeding caused by trauma. But such side effects are extremely rare, and if you are properly prepared, do not regurgitate, and comply with all the requirements and commands of the endoscopist, then the risks are minimal.
As a rule, gastroscopy is prescribed during examination by a specialist doctor if there are complaints about the gastrointestinal tract, i.e. "on demand". some are forced to undergo “preventive gastroscopy” 2 times a year during periods of exacerbation of diseases and as part of a “dispensary examination” if this item is checked for your age. But if pathologies are detected, the gastroenterologist or attending physician prescribes this examination individually, depending on the severity of the disease.
If you care about maintaining your health, we recommend that you undergo gastroscopy and colonoscopy every 4-5 years, in the absence of pathology. Ask your endoscopist what interval he recommends for you!
What happens after the procedure?
Inserting an endoscope into the stomach causes discomfort that may persist in the throat for a couple of days, but nothing more. Patients may also experience slight abdominal pain, but this also goes away quickly. It is extremely rare that damage to the endoscope may result in bleeding in the wall of an internal organ, but in other cases there are practically no complications.
The consequences will be much more serious when patients neglect the doctor’s instructions and go for the procedure after eating. In this case, food debris can move higher into the respiratory tract, which, in turn, leads to an attack of suffocation. If a person strictly followed all the rules, neither he nor the doctor will have any problems during FGDS of the stomach. The specialist will receive clear and complete images of the internal walls, which will help him more accurately determine the diagnosis. In particular, FGDS allows you to determine:
- Volumetric formations in the gastrointestinal tract
- Patency of the esophagus, stomach and some parts of the intestine
- Hernia in the esophageal opening of the diaphragm
- Gastrointestinal diseases at different stages
- Changes in the condition of the mucous membrane
- Protrusion of the muscle wall and other pathologies and diseases
In the absence of food and water in the esophagus, all these problems are clearly visible on the monitor screen. Thanks to FGDS, the doctor can prescribe timely treatment and overcome the disease at an early stage.