— Yulia Olegovna, coronavirus often affects the lungs. How do these pneumonias differ from bacterial ones?
— They differ from bacterial pneumonia primarily in the prevalence and nature of inflammation. As a rule, these are bilateral polysegmental pneumonias. The term “covid pneumonia” is even more suitable for the term “viral covid pneumonitis”. Such inflammation in the lungs proceeds differently - with the development of interstitial inflammation (that is, affecting the walls of the alveoli and the connective tissue of the lung. - Ed.) and thrombosis of small pulmonary vessels, the formation of such a complication as pneumofibrosis. And it requires longer treatment than with bacterial pneumonia, early initiation of rehabilitation measures and their continuation even during the period of follow-up treatment and recovery.
— What happens in the lungs during covid pneumonia?
— Against the background of a viral infection, damage occurs to the wall of the pulmonary alveoli, pulmonary interstitium (connective tissue. — Ed.), involved in gas exchange of small vessels (which causes vasculitis, microthrombosis). The nature of inflammation is different than with bacterial pneumonia - there the alveoli are filled with liquid or purulent secretion, but here this is not the case. Bacterial pneumonia takes a certain time to worsen, but with viral pneumonia, lung damage can be fulminant in nature and subsequently lead to severe fibrosis. The risk of developing fibrosis in the lungs is higher in patients with extensive lung lesions, in those who have undergone mechanical ventilation, in patients with concomitant pathologies (diabetes mellitus, obesity, hypertension).
Fibrosis in the lungs can be accompanied by a constant cough, fatigue and poor tolerance to normal physical activity.
The course of covid pneumonia is unpredictable; it is impossible to say in advance how the disease will progress in a particular person. Sometimes pneumonia with initially minor damage to the lungs has a severe course, with rapidly increasing symptoms and the amount of damage to the lung tissue, up to life-threatening complications and death.
— Tell us more about fibrosis. What other complications are there after Covid?
— The main target of coronavirus infection is the lungs, therefore, viral pneumonia, especially severe, with a large volume of damage, invasive ventilation of the lungs during treatment can result in fibrosis in the lungs. Fibrosis is the consequences of an inflammatory process when lung tissue is replaced by connective tissue scar. In layman's terms, this is a scar on a lung. If it is small in size, it will not affect pulmonary function and gas exchange. If the fibrosis is extensive, bilateral, affecting several segments or even lobes, then in the future this can lead to irreversible changes in pulmonary function, respiratory failure, even disability.
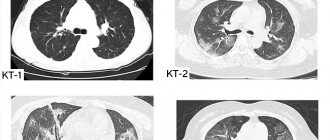
Yulia Semirech explains: viral pneumonia has certain radiological features, the so-called “ground glass” symptom. Even if the COVID test is negative, a chest CT scan can determine Covid pneumonia with a high degree of confidence.
— How does fibrosis manifest?
— After suffering from Covid, patients complain of shortness of breath during normal physical activity, which does not go away for several weeks or even months (shortness of breath can also be a manifestation of post-Covid asthenic syndrome). Also, fibrosis in the lungs can be accompanied by a constant unproductive cough, fatigue, and poor tolerance to normal physical activity. The most informative method for assessing the prevalence of fibrosis is computed tomography of the chest. In addition, doctors prescribe body plethysmography (a study of the relationship between different lung volumes) and spirometry (a method that allows one to estimate the volume of inhaled and exhaled air. - Ed.), since the vital capacity of the lungs can be reduced with pulmonary fibrosis.
— If fibrosis is an inflammatory stage in the lungs, then you can try to avoid it?
— As I already said, it cannot be said that this patient will develop fibrosis one hundred percent, and another will not have it. But the greater the degree of lung damage, the higher the risk of developing fibrosis. Therefore, during treatment, it is very important to follow all the doctor’s instructions, have a positive attitude toward recovery, begin rehabilitation measures while still in the hospital stage, and continue the course at the outpatient and follow-up stages. This may take from several weeks to several months.
— Are there effective methods for preventing fibrosis?
— Since there are no highly effective, universal drugs for the prevention of fibrosis, it is necessary to start non-drug methods of prevention as early as possible. First of all, this is therapeutic breathing exercises. There are many breathing techniques: therapeutic exercises according to Strelnikova, Buteyko, yogic breathing. You can use breathing simulators that you make yourself: blowing air through a tube into a glass of water. Do this exercise for 10 minutes three times a day.
“You can’t inflate balloons!”: how to restore your lungs after coronavirus pneumonia. Photo: prouzel.ru
It should be noted that the breathing exercise beloved by many - inflating balloons - is prohibited in the acute period of the disease, as there is a risk of damage to the inflamed lung tissue, including the development of pneumothorax. But during the period of follow-up treatment, chest massage and physiotherapeutic procedures are very useful (but taking into account contraindications).
— Is physical activity useful and what should not be done during the recovery period?
— Physical activity should be dosed. During the post-treatment period, walking and Nordic walking are very useful (where the upper shoulder girdle is involved; movements help improve drainage function and blood flow in the lungs). But heavy physical activity should definitely be avoided, since the body needs to be given time to recover from a severe infection. It is also forbidden to breathe in essential oils, which can settle in the lungs, disrupting blood supply and gas exchange in them. Do not breathe in aggressive non-medicinal products, alcohol solutions, or soda. And our people really like to self-medicate. By the way, many of those who have had a hard time with Covid subsequently quit smoking due to severe respiratory discomfort and shortness of breath. And even experienced smokers.
With covid pneumonia, tests can give a negative result, since the virus has penetrated into the lower respiratory tract and is no longer present in the upper respiratory tract, where a smear is taken. Photo: Vladimir Voropaev
— Why do patients with severe lung damage (60-70 percent) test negative for covid?
“Unfortunately, false negative tests are not uncommon. Approximately every third patient with pneumonia has a false-negative PCR test for COVID-19, and there are patients for whom this test was performed more than once. There may be several reasons: violation of the timing and technique of taking smears, unpreparedness of the patient (certain conditions must be met). With the development of covid pneumonia, tests may well show a negative result, because the virus has already penetrated far into the lower respiratory tract and may no longer be present in the upper respiratory tract, where the smear is taken.
In approximately every third patient with pneumonia, a PCR test for COVID-19 shows a false negative result.
— What do doctors then focus on when prescribing treatment?
— The fact is that X-ray viral pneumonia differs from bacterial pneumonia. And from the picture we can say with a high degree of confidence that this is Covid pneumonia. It has certain radiological features, the so-called “ground glass” symptom; the changes are bilateral, located subpleurally and affect several segments of the lungs. In addition, patients describe symptoms characteristic of coronavirus infection that cannot be confused with other viral diseases. All patients say: “This is the first time in my life that I have been sick like this.” If a patient wants to make sure that he has suffered from coronavirus pneumonia, we recommend that he take an antibody test. And in 99 percent of patients these antibodies are detected.
— Is it true that after suffering from coronavirus pneumonia, a person can get sick with it again?
— There is evidence that during the first 6-8 months after suffering from covid pneumonia, people are protected from re-infection, they develop antibodies and develop immunity. By the way, we also have another type of immunity - cellular, which also protects against viral infections. In my practice, I have not yet encountered patients who became ill with coronavirus again. Although I heard that such cases happen. You need to understand that against the background of a weakened immune system after coronavirus, you can become infected with any other viral infection that has not disappeared from our lives and spreads seasonally.
— Vaccination against Covid is underway today. Will you get vaccinated?
— I’ll post it, but later, because I’ve already had coronavirus infection (everyone in my family has had it). The number of viral pneumonias is now declining, I see that there are fewer patients than there were before the New Year, and I think that we will not reach the third wave, but will safely emerge from this difficult epidemiological situation. Vaccination, of course, will also play a significant role in this.
Using a chest CT scan, doctors can say with a high degree of confidence that pneumonia is coronavirus, even with a negative test for COVID-19.
Those who have not had coronavirus need to be vaccinated. It is extremely difficult to protect yourself from infection, as well as to predict the course of coronavirus infection. I believe that the risk of developing complications from vaccination is lower than the risk of severe coronavirus infection and its complications. And in my practice I encounter complications every day, and these are not only pneumonia, but also myocarditis, pericarditis, heart rhythm disturbances, polyneuropathy, facial nerve neuropathy, venous thrombosis and more.
— Is rehabilitation of patients after Covid carried out at the Far Eastern Scientific Center for Physiology and Pathology of Respiration?
— Yes, we have developed a good rehabilitation complex. We use therapeutic exercises, chest massage, physiotherapeutic procedures, and, if necessary, drug therapy. These are not only patients after pneumonia, but patients with post-Covid asthenic syndrome, mild post-Covid complications from the nervous and cardiovascular systems.
— Who can be denied rehabilitation?
— In case the patient does not fit the rehabilitation program. If there are decompensated chronic diseases of the lungs, heart, rhythm disturbances, any acute diseases until recovery. About 100 people have already completed a rehabilitation course with us. Demand is high; registration for February was started in January. The effect of rehabilitation is good. Many patients note that they have gained physical strength, shortness of breath has decreased, their health has improved, and their sleep has returned to normal.
Photo: Andrey Ilyinsky
To protect yourself from covid pneumonia and other lung infections, you need to:
— get vaccinated against influenza annually, vaccinated against coronavirus infection, and subsequently vaccinated against pneumococcal infection (pneumococcus is the most common causative agent of bacterial pneumonia);
- stop smoking - the less aggressive the effect on the respiratory tract, the better;
— promptly sanitize chronic foci of other infections;
— play sports whenever possible, lead an active lifestyle (athletes rarely suffer from severe covid pneumonia, and they usually do not have fibrotic changes in the lungs);
— eat properly and nutritiously, take preventive courses of vitamins and mineral complexes;
— humidify the air in the house;
— continue to wear masks, treat your hands with antiseptic, and avoid large crowds of people.
Age category of materials: 18+
- Larisa Khatamova
- Amurskaya Pravda from 02/11/2021

What to do if a white spot is detected on the x-ray
When performing a chest x-ray or fluorography in a patient with tuberculosis, a white spot on the x-ray reflects either an inflammatory lesion of the lung tissue or destructive changes in the parenchyma with the formation of abscesses, tubercles, and caverns. Correctly, this symptom should be called darkening, since it reflects the characteristics of the passage of x-rays through objects and their color display on the x-ray.
A white shadow in a photograph is also observed when:
- pneumonia;
- atelectasis;
- exudative pleurisy;
- occupational diseases (silicosis, talcosis, asbestosis).
Radiographs with white spots of various origins: 124.3 – breast piercing, 124.4 – shot in the soft tissues of the chest, 124.5 – professional cementosis, 124.6a – contrast during bronchography, 124.6b – pneumonic focus, 124.7 – interlobar pleurisy (arrows indicate artifact)
This syndrome is a sign of many pathological changes in the lungs, but we will look at the most common options.
If spots are detected, additional research is necessary to determine the cause of the pathology. For these purposes, a radiologist may prescribe an X-ray examination in additional projections or perform layer-by-layer computed tomography or magnetic resonance imaging.
Treatment of stage 4 lung cancer with metastases
Treatment depends on the location, number and location of metastases, the age and condition of the patient, and the type of lung cancer. Non-small cell cancer is the most common, occurring in more than 80% of cases.
Sometimes single metastases can be removed surgically and with radiation therapy. In some cases, this can even lead to remission. For example, small lesions in the brain can be destroyed using stereotactic radiosurgery
(gamma knife machine), and then conduct a course of radiation therapy.
In most cases, there are many metastases, many of them are microscopic in size and cannot be removed. In such cases, the main treatment methods are: chemotherapy, immunotherapy, targeted and radiation therapy.
If cancer cells have certain molecular genetic characteristics, various targeted drugs can be used:
- For changes in the ALK gene
: crizotinib (Xalkori), ceritinib (Zikadia), alectinib (Alecensa), brigatinib (Alunbrig). - For changes in the EGFR gene:
erlotinib (Tartseva), gefitinib (Iressa), afatinib (Giotrif). - For changes in the ROS1 gene:
crizotinib (Xalkori). - For changes in the BRAF gene:
dabrafenib (Tafinlar), trametinib (Mekinist).
In some patients, immunodrugs - monoclonal antibodies -
: pembrolizumab (Keytruda), bevacizumab (Avastin). They block molecules that prevent the immune system from recognizing and attacking tumor cells.
What does a spot look like on an x-ray with pneumonia?
In pneumonia, the spot on the x-ray image has a length depending on the size of the lesion in the pulmonary parenchyma:
- limited – up to 3 cm in diameter;
- segmental – within a segment;
- subtotal – the entire field, with the exception of the tops;
- total.
Pneumonia is an inflammatory disease that affects the alveolar tissue with accumulation of fluid in the acini. Pathogenesis forms a specific x-ray picture of the disease.
X-ray. Focal pneumonia in the lower lobe on the right
The white spot with pneumonia has fuzzy, blurred contours. Its intensity can be low or high, depending on the characteristics of the exudate (inflammatory fluid in the lumen of the alveoli). A path from the root approaches the site of its localization due to lymphangitis.
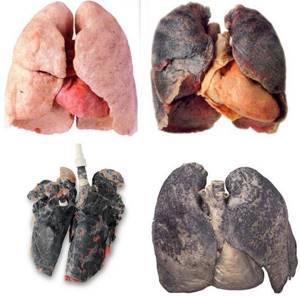
Main pathologies of smoker's lungs
The main pathologies of a smoker's lungs are combined under the name chronic obstructive pulmonary disease (COPD).
It can be prevented by quitting smoking. But, unfortunately, this is easier said than done. About 70% of smokers want to quit smoking, but only 7% do not smoke after a year of trying, but you should not stop. It will take numerous attempts, sometimes more than 10, as well as professional help, but the health benefits of quitting smoking are worth all the effort. COPD consists of two main related diseases: emphysema and chronic bronchitis. Some begin to develop emphysema, while others develop chronic bronchitis. But for most, these diseases develop together.
About the lungs of a smoker
Smoking is associated with a variety of pathologies throughout the body, which cause not only illness, but very often death. In fact, if all smoking-related deaths (lung disease, heart disease, and cancer of many organs) were considered, smoking would be the leading cause of death in industrialized countries. Paradoxically, this cause of death is the easiest to prevent in society! The study focused on the lungs of smokers. The term “smoker's lungs” refers to structural and functional pathologies (diseases) of the lungs caused by smoking. First, we will describe the normal lungs, both structurally and functionally. Then we will consider and describe the functional and structural pathologies caused by smoking.
Lung structure is normal
We have a right and a left lung, which are located in the chest cavity and around the heart. The outer surface of the lungs is covered by a thin membrane called the pleura. Inhaled air enters the lungs through the respiratory tract (airways). The respiratory tract consists of the oral and nasal cavities, which connect to the larynx, which connects to the windpipe (trachea). The windpipe splits into two airways called bronchi, which go to both lungs (right and left main bronchi). The trachea and large bronchus in the walls contain strong arches of cartilage. Cartilage prevents the airways from closing when negative pressure is created, such as occurs during inhalation (drawing in air). The right lung is divided into three sections: the upper, middle and lower lobes, while the left lung has only two: the upper and lower lobes. Each lobe has its own bronchus and blood supply. Further along the respiratory tract within the lung, the bronchi are divided into tiny (narrow) tubes, similar to the branches of a tree. Hence the term tracheobronchial tree. The walls of the bronchial tubes contain muscles that help the airways expand or contract (narrow). For example, during exercise, the airways widen to increase air flow (breathing). Conversely, when the air is polluted or cold, the airways contract to protect the lower tissues from damage. The small branches of the bronchial tree, called bronchioles, also contain muscle but no cartilage. Even the smallest bronchioles (respiratory bronchioles) connect directly to tiny air sacs in the lungs called alveoli. The bronchial wall contains cartilage and muscle. It should be noted that the surface (epithelium) of the bronchi, as well as the trachea and bronchioles, is lined by different types of cells. One type of cell is called goblet cell due to its shape. Goblet cells produce mucus, which moistens the airways and traps inhaled foreign substances (such as bacteria, viruses, and pollutants). Other epithelial cells are called ciliated, which will be discussed in the next section. Beneath the surface of the airways, goblet cells and other epithelial cells form clusters of structures called bronchial glands. These glands produce additional mucus and other lubricating fluids.
Pathologies (diseases) of a smoker's lungs
The main pathologies of the lungs of smokers are combined under the name chronic obstructive pulmonary disease (COPD). It is estimated that 40 million people worldwide have COPD. COPD is the 4th leading cause of death in the United States. The more frightening fact is that COPD is among the “top five” causes of death that have increased over the past decade. It was believed that COPD affected men, but according to some data, by 2010 there will be more women with this disease than men. The statistics are even sadder because COPD can be prevented by quitting smoking. But, unfortunately, this is easier said than done. About 70% of smokers want to quit smoking, but only 7% do not smoke after a year of trying, but you should not stop. It will take numerous attempts, sometimes more than 10, as well as professional help, but the health benefits of quitting smoking are worth all the effort. COPD consists of two main similar diseases. The first disease, emphysema, affects the pulmonary alveoli, and the other, chronic bronchitis, affects the bronchial airways. Both diseases will be described below. This study uses the term chronic bronchitis, which combines chronic bronchiolitis and chronic respiratory bronchiolitis. This is because these three diseases have the same pathology (structural pathologies), the same symptoms and differ only in their location in the airways. One way or another, some begin to develop emphysema, while others develop chronic bronchitis. But for most, these diseases develop together.
What happens to a smoker's lungs with emphysema?
With emphysema, the walls of the air sacs, that is, the alveolar septa, are destroyed. Consequently, individual air spaces (alveoli) become larger, but not equally and their number decreases. Large spaces are less efficient for gas exchange than normal-sized alveoli. Thus, emphysema disrupts the distribution of oxygen and carbon dioxide, that is, gas exchange. The more extensive the emphysema, the worse gas exchange occurs. With emphysema, the capillaries are also destroyed along with the rest of the alveolar walls. As a result, emphysema interferes with normal blood circulation. This disease usually begins to develop in the upper lobes of the lungs and is more severe in the upper lobes for several reasons. That is, pathological (enlarged and irregularly shaped) air sacs are more pronounced in the upper lobes. Blood vessels in the lungs should not be confused with abnormal air sacs. In patients with severe emphysema, the chest is enlarged. And this happens because the patient makes too many compensatory efforts to inhale as much air as possible to improve breathing. This helps to enlarge the lungs and chest. Thus, in a patient with severe emphysema, the chest takes on a barrel shape.
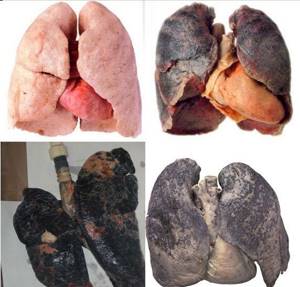
Why are smokers' lungs dark?
The lungs connect to the airways and are exposed to a potentially harmful external environment. Accordingly, the alveolar spaces normally contain special alveolar macrophages. Their job is to absorb (phagocytose) any harmful foreign substances that enter the lungs through the respiratory tract. As you know, cigarette smoke contains impurities that are inhaled by the smoker in large quantities, and they enter directly into the lungs. For this reason, the alveolar spaces of the smoker contain many macrophages, which are filled with absorbed (phagocytosed) particles of impurities and waste. Under a high power microscope, black and brown engulfed particles can be seen within the alveolar macrophages. In fact, a smoker's lungs may contain so many of these particles that they may appear gray-black to the naked eye. Therefore, in most cases there is no need to resort to a microscope to determine whether the patient is or was a heavy smoker. When examining a smoker's lungs with the naked eye, one may see enlarged gray-black lungs with enlarged air sacs.
Lung cancer in smokers
Tobacco smoke contains more than 60 carcinogens (chemicals that cause cancer) and about 200 known toxicants. Scientists are still studying how carcinogens work and why only some smokers develop lung cancer. Genes are inherited blocks on chromosomes and play a major role in susceptibility to cancer. Genes are made up of DNA (deoxyribonucleic acid), which controls cell division and reproduction. DNA damage from cigarette smoke can cause cells to multiply and grow uncontrollably, which is what cancer causes. It is very interesting why some smokers develop COPD, some develop lung cancer, some have neither of these diseases, and some develop them together. The reason for these different predispositions is not yet known. Additionally, lung cancer caused by smoking can take many different forms. For example, cancer cells may resemble skin cells (squamous cell carcinoma), bronchial gland cells (adenocarcinoma), or special cells of the nervous system (neuroendocrine carcinoma). The prognosis for such lung cancer patients may be as follows. Almost all types of lung cancer are fatal. Therefore, if lung cancer is larger than 2.5 cm in diameter or has spread beyond the lungs, less than 50% of patients will survive the next 5 years. And this happens even with the best therapy. Moreover, cancer is of concern if the tumor is smaller than 2.5 cm or not large enough to be seen on a chest x-ray and is located within the lungs. Unfortunately, even in this case, the cancer is completely removed through surgery, but about 25% of patients will nevertheless die from cancer within 5 years of diagnosis. The reason for such a sad result and prognosis is that lung cancer tends to spread as metastases to other organs at an early stage of its development. Most often these organs are the brain, liver and bones.
Are there reversible consequences of pulmonary diseases in smokers?
First, the bad news. Emphysema is irreversible. But there is good news. If a person stops smoking, inflammatory changes such as chronic bronchitis in the airways will likely disappear. In addition, when a person stops smoking, the risk of developing lung cancer decreases, but they never return to normal. In other words, the risk of developing cancer in former smokers is much lower than in current smokers, but remains high than in non-smokers.

Why do smokers die?
What is surprising is that, despite information about the death rate from smoking, there is little information about the specific causes of death in smokers. Smokers with COPD may die from oxygen deficiency (hypoxia) in the body's tissues. Hypoxia occurs because there is such a small area of functioning lung left and/or the effort to breathe is so great that the patient stops breathing from exhaustion. Other important causes of death in smokers include lung infection (pneumonia), lung cancer, cancer of the digestive, urinary and reproductive systems, and leukemia. In fact, because smoking causes cancer in so many organs, 30% of all cancer deaths are related to smoking.
However, because smoking is such a powerful risk factor for the development of coronary artery disease (hardening and blockage of the heart's arteries), heart disease is the most common cause of death in smokers. Moreover, since autopsies are performed on less than 10% of patients who die in hospital and on less than 1% of patients who die in treatment centers, there is no way to determine what causes most smokers to die. Even if a doctor correctly determines the patient's cause of death, only an autopsy can provide a more accurate answer.
Print Email
Atelectasis of the lung or x-ray semiotics of triangular spots on the image
Lung atelectasis is a disease accompanied by the collapse of a segment, lobe or lung tissue completely against the background of cessation of bronchial ventilation. Radiologically, such changes are called limited darkening, since they do not extend beyond the segment or subsegment and have a triangular shape.
Atelectasis of the middle lobe of the right lung - frontal and lateral radiographs
How to identify atelectasis in an image:
- the size of the spot coincides with the size of the changed segment;
- triangular darkening in the lungs can be seen in frontal and lateral projections;
- during inhalation photographs the size of the spot does not increase;
- the narrow end of the triangular shadow is directed towards the root;
- Holtzknecht-Jacobson symptoms are observed during fluoroscopy (suction of the mediastinum towards the lesion during exhalation).
The morphological substrate of the pathology is the accumulation of infiltrative fluid in the alveoli, infiltration of lung tissue, and tumor growth in the pulmonary parenchyma.
Spontaneous atelectasis occurs in 1-3% of patients due to a defect in surfactant (the substance that forms the framework of the alveoli).
Schematic representation of the topography of segmental atelectasis
Limited darkening during collapse of the lungs requires knowledge of the segmental structure of the lungs, as it reflects atelectasis of a certain segment. By establishing the topography of the shadow, the doctor can guess which bronchus is affected. The substrate of formation (infiltrate, additional tissue, exudate) is almost impossible to determine on the basis of a radiograph.
What does a white spot mean in a picture of tuberculosis?
In tuberculosis, a focal spot on a chest x-ray indicates the infiltrative stage of the disease, when mycobacteria begin to infect the lung tissue. In this case, the x-ray shows a path to the root from the side of the lesion (due to lymphangitis). Such radiological symptoms are called “primary tuberculosis focus”.
Radiographs for various types of tuberculosis
Multiple small disseminated shadows on both sides indicate miliary tuberculosis.
A single large shadow with a cavity inside (clearance) and a fluid level - an abscess formed against the background of destruction of the lung parenchyma - “ring shadow” syndrome.
A spot on an X-ray of the lungs in the projection of the pulmonary fields reflects a pathological process, the causes of which should be established by additional research.