Pneumonia or pneumonia is a complication of respiratory diseases of the airways caused by viruses, bacteria, and sometimes fungal microorganisms. They are transmitted by airborne droplets or contact and provoke the development of the inflammatory process.
Any pneumonia is dangerous because it can lead to other serious complications: pulmonary edema or abscess, acute respiratory and heart failure, myocarditis, sepsis.
Lung damage due to pneumonia
Pneumonia affects the alveoli, the end portions of the lungs. They fill with fluid or pus. SARS, as well as the new coronavirus infection (COVID-19), is characterized by pulmonary fibrosis . This is a complication in which the lung tissue is replaced by connective tissue, and pathological growth of connective tissue occurs.
Alveoli are small air cells in the lung, when their volume is reduced due to fibrosis or fluid accumulation, critical respiratory failure occurs. A person experiences shortness of breath, coughs with sputum (sometimes with blood), and body temperature rises.
Sometimes the disease is asymptomatic, and this is especially dangerous since the carrier of the virus and pathogens continues to lead a normal and, no less important, social life. Meanwhile, his lungs are gradually collapsing. If pneumonia with focal lung damage is not detected in time and treatment is not undertaken, the consequences can be severe and irreversible.
Pneumonia can be unilateral or bilateral. If the lungs are affected by 10-25% or less, then the disease can be treated outpatiently. Damage to lung tissue of 30-50% is already an indication for hospitalization. If more than 50% of the lungs are affected, this indicates a severe form of pneumonia.
However, signs such as respiratory failure, cough, fever and runny nose are also characteristic of other diseases: ARVI, influenza, bronchitis and even allergies. How to identify pneumonia and distinguish pneumonia from other respiratory diseases? Let's consider what symptoms are characteristic of pneumonia, who is most susceptible to pneumonia, and how it is diagnosed.
Bronchial pneumonia: causes
Most often, bronchial pneumonia is bacterial in nature. Its causative agents are:
- streptococci,
- staphylococci,
- coli,
- Haemophilus influenzae.
Fungal infections can also cause the disease. Bronchial pneumonia develops as a result of a violation of the drainage function of the bronchi. Prerequisites for the development of pathology are acute respiratory viral diseases, influenza, and bronchitis.
People with reduced immunity are at risk of developing bronchial pneumonia. Various chronic diseases, immunodeficiency states, and bad habits weaken the body’s protective barriers, and therefore the infection begins to actively multiply in the lungs.
In addition, bronchial pneumonia occurs as a result of exposure to toxic substances and the penetration of foreign bodies into the respiratory tract.
Pneumonia: who is at risk?
At the turn of the 19th-20th centuries, before the discovery of penicillin and the introduction of universal vaccination, most patients died from pneumonia and other complications of acute respiratory diseases. Assessing statistics on deaths and disability, Sir William Osler, known as the “father of modern medicine,” called pneumonia “Captain of the men’s death”, since by 1918 the number of victims of this disease exceeded mortality from tuberculosis.
However, with the development of radiological diagnostic methods, X-rays, and then modern computed tomography, doctors have a tool for intravital assessment of the patient’s lung condition, determining effective treatment tactics and identifying pneumonia at an early stage - before it becomes severe.
The predisposition to developing pneumonia depends on the patient’s age, heredity, medical history and lifestyle. However, under certain circumstances, even a completely healthy adult is not immune from pneumonia. “Trigger mechanisms” include: contact with a carrier of pathogenic microorganisms (pneumococci, streptococci, mycoplasmas, coronavirus, fungi), systematic stress and lack of sleep, smoking, hypothermia, weakened immunity, some concomitant diseases, pulmonary fibrosis and a history of chronic ENT pathologies with relatives.
It is known that pneumonia is more susceptible to:
- Elderly people and children;
- Patients with diabetes;
- Patients with cardiovascular diseases (heart failure);
- Smokers;
- Patients with congenital pathologies of the respiratory tract or chronic ENT diseases (tonsillitis, bronchial asthma, obstructive pulmonary disease);
- Patients with suppressed immunity;
- Patients with exogenous intoxication (alcohol and other toxic substances);
- Patients with damaged teeth and gums (caries, pulpitis, tartar);
- Patients with Parkinson's disease;
- Workers in production facilities, medical dispensaries, etc.
Such patients need to especially carefully monitor their health and listen carefully to their body.
Signs of pneumonia
The most common viral pneumonia (or rather “pneumonia”) is characterized by the following symptoms:
- Cough of any nature: dry, wet, with sputum, purulent discharge, blood.
- Temperature - the patient may have a fever (39-40 degrees) and a slightly elevated body temperature.
- Chest pain and discomfort.
- Shortness of breath and wheezing in the chest, which can be heard when listening to the lung.
- Feeling of lack of air.
- Confusion.
- Prostration.
- A sore throat.
- Pain in muscles and joints.
Important! Pneumonia can be completely asymptomatic, and sometimes the presence of even 1-2 signs indicates lung damage.
Symptoms of SARS and COVID-19
What does the term “atypical pneumonia” mean? It is used when they want to emphasize that pneumonia is caused by microorganisms or causes that give a complex and unpredictable clinical picture. In this case, an atypical course of the disease is observed, relapses and complications are possible, which will require long-term rehabilitation.
SARS refers to pneumonia caused by mycoplasma and chlamydia. In this case, as with COVID-19, adults experience symptoms:
- Shortness of breath and shortness of breath;
- Loss of smell;
- Severe dry cough, which eventually turns into a wet cough with discharge;
- General poor health: even a temperature of 37 degrees is difficult to tolerate and lasts a long time;
- Pain in muscles and joints;
- Chest pain.
Just as in the case of ordinary pneumonia, some people experience an asymptomatic course of the disease. With coronavirus, the patient may have a runny nose with loss of smell, but there is no sneezing (unlike colds and flu).
Pneumonia can only be reliably identified or excluded using computed tomography of the lungs. A tomogram of the lungs shows lesions in the respiratory tract (“ground glass”). Laboratory tests will help identify specific pathogens of pneumonia based on the response of the immune system.
Bronchial pneumonia: treatment
Antibacterial therapy is used in the treatment of bronchial pneumonia. It is important to start treatment as early as possible, as the disease can progress quickly and lead to serious complications. The choice of antibiotics will depend on the type of inflammatory pathogen. The decision is made only by the attending physician or pulmonologist based on the results of the examination and laboratory and radiological studies. It is possible that several types of antibacterial drugs from different groups will be used for treatment to obtain the most effective therapeutic effect. Most often, cephalosporins and penicillins are used to treat bronchial pneumonia. The drugs are administered intramuscularly or intravenously, and then switch to oral administration. Antibiotics should be taken over a course of 10-14 days. The duration of the course will depend on the course of the disease and response to treatment. You should not interrupt the course of therapy until complete recovery, even if there is a significant improvement in the condition after a couple of days.
In addition to antibiotics, the patient is prescribed drugs that increase the body's immunological reactivity. Expectorants are used to remove mucus. The patient must remain in bed, drink plenty of fluids (about two liters per day), eat well, and take vitamins. Physiotherapeutic methods of treatment and physical therapy help to quickly cope with the disease.
The Yusupov Hospital offers patients with bronchial pneumonia inpatient treatment in comfortable conditions. Patients are provided with high-quality medical care, care occurs around the clock. To treat bronchial pneumonia, therapists at the Yusupov Hospital use effective evidence-based treatment methods that show the best results.
Yusupov Hospital is located near the center of Moscow and receives patients 24 hours a day, 7 days a week. You can ask for help, make an appointment and get advice from specialists by phone or through the feedback form on the website.
How to identify pneumonia: examination algorithm
1. Consult your doctor - after studying your case, the doctor will draw up an examination plan. Pneumonia is classified according to a number of characteristics (pathogen, location). Pneumonia can be bilateral, focal (bronchopneumonia), viral-bacterial - and the treatment regimen depends on this. Be prepared for the fact that if there is a suspicion of pneumonia, you will be prescribed tests and radiation diagnostics.
2. Get tested - laboratory PCR diagnostics will help differentiate pneumonia. This is important because viral and bacterial infections are treated differently. However, under certain circumstances, tests can give false positive or false negative results. For example, it is known that with the COVID-19 coronavirus, primary tests have an error of about 30%.
3. Check the lungs using reliable X-ray diagnostic methods - a chest scan will show lesions in the lungs, if any. Today, computed tomography (CT) of the lungs is recognized as the most informative and accurate way to diagnose pneumonia.
Unlike fluorography and x-rays, CT scan of the lungs will reliably show areas of lung damage even at the early stages of pneumonia (1 and 2), when the percentage of destruction of lung tissue may not exceed 10%. On tomograms, such areas of the lungs look like “frosted glass” or highlights. In this case, the patient will have time to start treatment on time, and there is no need for fluorography or x-rays. When the disease progresses to a more severe form 3 or 4 (a regular x-ray will show such pneumonia), it is no longer possible to cope with pneumonia at home and without subsequent special rehabilitation.
If the patient really has pneumonia, CT scans will visualize foci of destructive changes (swelling of the alveolar walls, fluid accumulations), and there will be several “ground glass” spots on the images. For example, with coronavirus they are usually located peripherally on both sides - in the posterior and lower parts of the lungs. One “frosted glass” may indicate other diseases (allergy, bronchial asthma) or an oncogenic process.
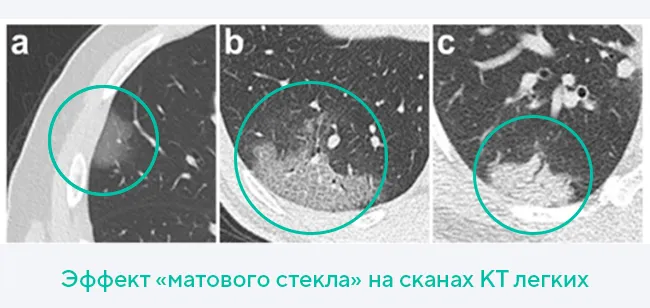
Thus, based on the presence of “ground glass” on a tomogram of the lungs and their location, doctors diagnose pneumonia. Additional examination methods (pulse oximetry, blood and sputum tests) are needed to determine treatment tactics.
Diagnosing pneumonia is a complex process in which doctors compare data and key markers to make an accurate diagnosis. The success of therapy and rehabilitation after pneumonia will depend on this, since it is also important to minimize the consequences of the disease.
Community-acquired pneumonia. Clinical examples
Lecture transcript
XXV All-Russian Educational Internet Session for doctors
Total duration: 21:21
00:00
Oksana Mikhailovna Drapkina, Secretary of the Interdepartmental Scientific Council on Therapy of the Russian Academy of Medical Sciences, Doctor of Medical Sciences, Professor:
— Conclusion of our Internet Session. I want to say right away that this conclusion was not chosen by academician Vladimir Trofimovich Ivashkin by chance: this is the start of a new project that will be supervised by Irina Aleksandrovna Sokolina.
Today Irina Aleksandrovna will talk about community-acquired pneumonia and clinical examples.
I want to say that our entire clinic (and not only our clinic, since we are in the same building) in all complex and not very complex cases when it is necessary to consult in terms of not only diagnosis, but also management of a patient with pathology of the pulmonary system and with additional lobules of the spleen (and with what else - I can’t even remember now)... The ninth floor is a favorite place for our consultations. Just the office of Irina Alexandrovna, the head of our X-ray diagnostics department.
Irina Aleksandrovna Sokolina, head of the department of X-ray diagnostics, First Moscow State Medical University named after I.M. Sechenov:
— Good day, dear colleagues! Today, the topic of our first presentation will be modern radiation diagnostics of pneumonia.
So. The objectives of radiation diagnostics for any disease are:
- identification of pathological changes in lung tissue;
- clarification of localization and prevalence;
- presence of complications;
- assessment of treatment effectiveness;
- differential diagnosis (most important).
01:32
For pneumonia, the following radiation diagnostic methods are used. Of course, it all starts with a survey X-ray of the chest organs, necessarily carried out in two projections - in the direct and in the lateral projection. This test is used at the onset of the disease and after an average of 7-10 days.
In complex clinical cases (for example, with a clinical picture of pneumonia or a high probability of developing pneumonia, but with questionable and normal radiographic data), it is advisable to perform a computed tomography study to confirm or exclude this disease and for the purpose of differential diagnosis.
An ultrasound examination is advisable if a pleural prolapse is suspected to identify it, as well as to clarify the condition of the fluid.
The frequency of X-ray examinations for pneumonia depends on the clinical situation. If the course of the process is unfavorable, including the development of complications, the frequency and type of X-ray examinations are determined by clinical indications.
The radiation picture of pneumonia depends on the type of infiltration.
Currently, the alveolar or so-called pleuropneumonic type of infiltration is distinguished. It develops when the inflammatory process is localized in the alveolar tissue. Most often caused by infectious agents such as pneumococci or Friedlander's bacillus, staphylococci.
X-ray signs of alveolar infiltration look like areas of infiltration, usually of a homogeneous structure, of medium intensity. In the infiltration zone, the air gaps of the bronchi are clearly visible (the so-called “air bronchography” symptom).
The infiltrate is adjacent to the costal pleura with a wide base. Its intensity decreases towards the root of the lung. Pathologically, the infiltrate is most often localized in the posterior lower parts of the lungs (within 1-2 segments, less often within an entire lobe).
04:02
The next type of infiltration: focal (so-called bronchopneumonic). It occurs with acute inflammation of the alveolar tissue of the lung, which develops on the basis of bronchitis or bronchiolitis. The most common infectious agents that cause bronchopneumonia are streptococci, influenza bacillus, Pseudomonas aeruginosa and staphylococci.
Radiological signs of bronchopneumonia are varied, but most often it is an area of infiltration of lung tissue of a heterogeneous structure, which consists of polymorphic (usually confluent) foci with unclear contours. The infiltration zone can occupy one or two segments. Bilateral localization is more common with this type of infiltration.
At the same time, it should be noted that about 10% of bronchopneumonia are not detected by X-ray examination.
Finally, the most difficult type of infiltration to detect using routine methods, plain radiography: the so-called interstitial type of infiltration. With it, infiltration occurs predominantly in the walls of the alveoli (the interstitial structures of the lung tissue are involved).
This should not be confused with interstitial pneumonia within fibrosing alveolitis.
Radiological signs of the interstitial type consist of one or several areas of compaction of the lung tissue, usually of a heterogeneous structure and low intensity. This is called the "ground glass" symptom. The infiltrate has unclear contours. In the area of these changes, it is possible to enhance the pulmonary pattern due to infiltration of interstitial structures.
High-resolution computed tomography plays a decisive role in identifying interstitial pneumonia.
As for community-acquired pneumonia, they usually occur in healthy people in the absence of diseases or pathological conditions that contribute to the development of the infectious process. The main infectious agents are pneumococci and mycoplasma.
Pathogens enter the lungs through the respiratory tract (bronchogenic), usually against the background of hypothermia, a stressful situation or acute respiratory disease.
As I already said, the x-ray picture is determined by the type of infiltration and the stage of the inflammatory process.
06:33
The most typical radiological signs are the local area of infiltration of the lung tissue (usually alveolar type), the volume of the lesion. Nowadays, lobar infiltrations are rare. Usually this is 1-2 segments. The change is usually unilateral.
As an example, I can give pneumococcal pneumonia, which develops as an independent disease. It is characterized by an acute onset and a vivid clinical picture. Radiological signs depend primarily on the stage of development of this pneumonia.
The hot flash stage will be characterized by a decrease in the transparency of an area of lung tissue without obvious boundaries due to hyperemia in the area of inflammation. In the stage of hepatization, we will see a characteristic alveolar infiltrate of lobar or segmental extent, against which the air gaps of the bronchi will be visible, and the symptom of “air bronchography” will persist. In the resolution stage, the shadow of the infiltration may become heterogeneous.
This should not be confused with the appearance of a focus of destruction, because areas of normalization of the lung tissue will also impart heterogeneity and cellularity to the inflammatory infiltrate.
With a computed tomographic examination (we see a frontal reconstruction on the left and axial sections on the right), pneumococcal pneumonia will have the appearance of a compaction of varying intensity - consolidation (these areas are located closer to the costal or interlobar pleura). Gradually, the intensity of the infiltrate decreases towards the root. It spreads to the root like an oil stain.
The following indications for computed tomography for pneumonia can be identified.
In a patient with obvious clinical symptoms of pneumonia, there are no changes in the lungs on the radiograph. In this case, to confirm inflammation (perhaps these are some small areas of infiltration), it is advisable to conduct a computed tomography study.
An X-ray examination of a patient with suspected pneumonia revealed, for example, changes atypical for this disease. For the purpose of differential diagnosis, it is advisable to use computed tomography as a clarifying method.
Definitely recurrent pneumonia. With it, pathological changes occur in the same area. Here, too, to clarify the reasons for these changes.
Of course, prolonged pneumonia, in which the duration of infiltrative changes in the lung tissue exceeds one month. Here, too, to clarify the reasons that prevent the resolution of pneumonia, it is advisable to perform a computed tomography study.
In general, pleuropneumonia is easily detected by routine x-ray examination.
09:53
As I already said, it is better to carry out differential diagnosis using computed tomography. The most important distinguishing sign of pneumonia is the visible air gaps of the bronchi in the structure of the infiltrate. We see this on the left slide: compacted tissues, air gaps in the bronchi.
In contrast, with abscesses or tuberculous infiltrates, which can also have the appearance of compaction of the lung tissue, we will not see this main symptom due to the fact that this condition is an abscess of caseous or other melting of the lung tissue.
Let me give you some complicated examples.
The patient, 62 years old, is a long-term smoker and suffers from chronic obstructive pulmonary disease. Due to an increase in cough and the appearance of low-grade fever, she went to the clinic at her place of residence. She was found to have changes in the lower lobe of the right lung, which were initially regarded as pneumonic.
She received appropriate antibacterial and anti-inflammatory treatment for a month. Her temperature returned to normal, but there were still changes on X-ray examination. Due to the fact that the complaints persisted, she was hospitalized at our clinic.
When performing a computed tomography study, we see a completely clear picture of a peripheral formation in the middle lobe of the right lung. Already with the phenomena of decay. Such a focus: adjacent to the pleura, with spicule-shaped contours, surrounded by a zone of lymphostasis, with the presence of enlarged lymph nodes in the root of the lung.
In a computed tomographic study, this picture did not present any difficulties in differential diagnostic terms.
11:58
One more example. The patient is 56 years old. He developed acute pain in the right side of the chest and increased shortness of breath. X-ray examination revealed changes in the middle lobe. They consisted of compaction at the base of the upper lobe (in the third segment). Initially, they were also regarded as pneumonic.
But due to the addition of hemoptysis, he was hospitalized in the hospital. Yes, we see that with X-ray examination... On computer tomograms at the base of the upper lobe, the compaction of the lung tissue, adjacent to the wide base, is more intense in the area of the interlobar pleura. But it has the appearance of permeation of the lung tissue, which is usually characteristic of hemorrhage.
In the basal sections we see areas of co-pleural linear fibrosis. The fact that these changes are bilateral and so numerous allowed us to assume the presence and suspect thromboembolism in the patient, which subsequently... These areas of linear fibrosis are like areas of already suffered heart attacks.
When performing CT angiography, we see bilateral perfusion defects, thrombi in both the right and left pulmonary arteries. Against the background of contrasted vessels, they look like grayer structures, which made it possible to change the diagnosis in this patient to recurrent pulmonary embolism and pulmonary infarction.
13:51
Of course, it is impossible to establish the etiological factor by X-ray examination. But a number of pathogens have a very characteristic (and pneumonia caused by these pathogens) picture.
Staphylococcal primary pneumonia, which develops in children and the elderly. They are characterized by an x-ray picture: they have one or several areas of bronchopneumonia. As a rule, this is a bilateral lesion, thin-walled cavities of destruction. A typical picture.
As for secondary staphylococcal pneumonia, they occur with hematogenous spread of infection or acute chronic purulent process. They also have the appearance of multiple round-shaped infiltrates (bilateral, as a rule). They are characterized by polymorphism with the formation of thin-walled cavities of destruction, which then resolve.
Differential diagnosis of these conditions must be carried out with suppurating cysts, true lung abscesses and subacute disseminated tuberculosis. But the main thing in this situation is not the radiation picture in differential diagnosis, but, of course, the clinical picture and anamnesis.
Pneumonia caused by gram-negative infection, as a rule, develops in middle-aged and elderly people, weakened, and suffering from chronic diseases. Caused by infectious agents such as Klebsiella, Pseudomonas aeruginosa, Proteus. They have a severe clinical course and high mortality.
Here we see an example of pneumonia caused by Klebsiella. With such pneumonia, extensive lobar darkening and an increase in the volume of the affected lobe are caused. Characteristic is the rapid appearance of destruction cavities in the structure of the infiltrate.
Mycoplasma pneumonia. They have become more frequent lately. They are characterized by infiltration of the alveoli and interstitial tissue. They have a very diverse x-ray picture. They can occur as interstitial changes such as bronchopneumonia, bronchiolitis, and so on.
16:20
I will give you a few examples of mycoplasma pneumonia. In this case, we see an increase in the pulmonary pattern in the lower lobe of the right lung, blurring and deformation of the bronchovascular bundles.
In this case, pneumonia has a form close to the radial picture of bronchiolitis: in the form of confluent foci in the center of the lobular foci, caused by the expansion and filling of bronchioles. As a rule, with such forms of mycoplasma pneumonia, severe broncho-obstructive syndrome is observed, which persists for a long time after the resolution of this pneumonia.
A severe form of mycoplasma pneumonia in the form of extensive areas of the “ground glass” type with almost subtotal damage to the lung.
The X-ray picture of this pneumonia can be different.
As for viral pneumonias, they occur in children and adolescents. As a rule, viral agents and pathogens are adeno- and rhinoviruses, influenza viruses. These pneumonias are characterized by an interstitial type of changes in the lung tissue, and therefore are the most difficult to diagnose.
Let me dwell on influenza pneumonia. The clinical picture is usually dominated by signs of toxicosis, hyperthermia, and headache. This pneumonia is characterized mainly by an interstitial type of changes in the initial stages.
In this case, we see strengthening and deformation of the pulmonary pattern (usually in the hilar regions). Small focal shadows. Localization in the middle and lower parts of one or both lungs. Root reaction.
A computed tomographic examination can reveal thickening of the pulmonary interstitium, areas of compaction of the lung tissue like “ground glass”, located peribronchially or perivascularly.
Here we saw an example of a 48-year-old young woman we observed. Unfortunately, she died from influenza pneumonia. In the terminal stage we see bilateral focal confluent pneumonia. Signs of hemorrhagic tracheitis were found at autopsy. The pathological examination also showed massive infiltration of the lung tissue with hemorrhagic impregnation.
19:02
What should be the tactics for radiological examination of patients with community-acquired pneumonia?
The main method of radiological examination of patients with suspected or established pneumonia is, of course, radiography of the chest cavity in two projections. To clarify the X-ray data, either linear, but best of all, of course, computed tomography can be used.
The main radiological sign of pneumonia, as I have already said, is local compaction of the lung tissue with the presence of an air lumen in the bronchi. In the absence of a symptom of compaction of the lung tissue, an x-ray conclusion about the presence of pneumonia is invalid. I mean, especially when it comes to CT scans. If we do not detect pneumonia using this method, there is no X-ray-negative pneumonia in this case.
An X-ray examination is carried out, as a rule, at the onset of the disease and no earlier than 14 days from the start of antibacterial therapy. But it can be performed at an earlier date if complications arise or a significant change in the clinical picture of the disease.
The X-ray picture of community-acquired pneumonia, as I have already said, has no correlation with the etiology of pneumonia. The degree of its clinical course does not allow determining the outcome of the disease.
With an X-ray examination of pneumonia in dynamics, changes in the lung tissue gradually decrease, but persist for a longer time than clinical symptoms. We need to remember this. They have the right to be stored for three months, so the most important thing here is to focus on the clinic.
A prolonged or recurrent course of pneumonia is an indication for a tomographic or bronchological examination to exclude central lung cancer, as well as other inflammatory processes in the lung tissue.
According to our experience and according to the literature, computed tomography has significant advantages in comparison with the same linear tomography in assessing the condition of the lung tissue and bronchi.
Thank you for your attention.
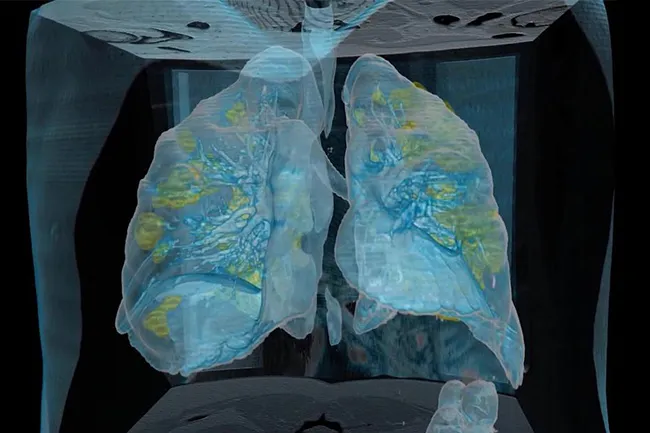
CT scan of the lungs for SARS and COVID-19
Today, CT scan of the lungs is considered the “gold standard” for diagnosing pneumonia, since it accurately shows the extent of lung damage even in the early stages. The sensitivity of fluorography and x-rays is significantly lower. For example, on an x-ray, the doctor will see areas of heterogeneous darkening, which can be interpreted as pneumonia, when pneumonia has already reached stages 3 and 4. Errors cannot be excluded in laboratory tests. Therefore, the most optimal type of radiation diagnosis for pneumonia will be modern computed tomography, eliminating the need for other radiographic studies.
During the SARS (2002) and MERS (2012) epidemics of atypical coronavirus pneumonia, doctors were faced with a problem - the inaccuracy of laboratory tests. In the case of the new coronavirus infection COVID-19, approximately 30 out of 100 patients who had their blood and sputum tested had false negative results. Only when the patients' condition worsened did CT scans reveal clinically significant areas of lung tissue destruction. It turned out that coronavirus pneumonia is best visualized on a CT scan of the lungs. Areas of damage to the alveoli correspond to “ground glass”—light areas of the lungs that are clearly visible on CT scans.
A CT scan of the lungs is done according to a doctor’s indications or independently if there are symptoms of pneumonia. If ARVI or atypical viral pneumonia caused by COVID-19 is suspected, it is recommended to do a CT scan of the lungs. In this case, the study will allow us to determine the specifics of the changes, and therefore will be the most informative. If necessary, the patient may be prescribed other examination methods in a medical institution.