The use of a rigid hysteroscope when examining the pelvic organs in women allows doctors to see what no ultrasound can show. With hysteroscopy, the specialist sees the uterine cavity in full view and, what is especially important, can at the same time remove the detected tumors without performing a second operation. That is why paid gynecology in Nizhny Novgorod recommends an endoscopic examination if a polyp in the uterus is suspected, which is almost impossible to detect on an ultrasound, but it is one of the causes of infertility in women.
What is hysteroscopy
Hysteroscopy is a method of examining the uterine cavity using a special optical system that is inserted into the cavity through the cervix. It can be diagnostic and surgical (hysteroresectoscopy). Diagnostic is a low-traumatic method, carried out under the full supervision of a doctor, using an optical system that transmits to the monitor an enlarged image of the uterine cavity several times. This magnification allows you to see the smallest changes in the inner layer of the uterus, perform surgical procedures to remove small polyps, small adhesions, membranes, and make a diagnosis. Treatment of disorders using surgical hysteroscopy allows for the removal of endometrial polyps, myomatous nodes, septa and dense adhesions, and other formations. Hysteroscopy allows women with a benign tumor in the inner layer of the uterus to undergo surgery more easily, recover quickly after surgery, and increases the chance of pregnancy.
The procedure is prescribed 7-10 days from the start of the menstrual cycle. The endometrial layer is still small, changes and formations in the uterine cavity are clearly visible. To improve visibility, the uterine cavity is expanded - liquid or gas is injected into the uterus under pressure through a hysteroscope. The device contains a light sensor that illuminates the uterine cavity, and the camera on it transmits what is happening to the monitor. Using the device, the doctor can carefully examine the cervical canal of the cervix, the opening of the fallopian tubes, and the inner layer of the uterus. With the help of hysteroscopy, the doctor can detect the reason for the failure of pregnancy, which could not be detected by other means. Very often, the cause of non-pregnancy is synechiae, which forms in the cervical canal or uterine cavity. Subtle synechiae cannot always be seen using other research methods. Endometrial hyperplasia is also not always detected by ultrasound. A symptom of endometrial hyperplasia is heavy menstruation, which may be the reason for prescribing hysteroscopy. Diagnostic hysteroscopy is used to examine the condition of the uterine cavity in postmenopausal women to exclude the development of cancer. For postmenopausal women, hysteroscopy is prescribed any day. Diagnosis can take about 30 minutes, the use of surgical hysteroscopy takes from half an hour to two hours. Diagnostic hysteroscopy is performed without the use of anesthesia, surgical hysteroscopy is performed under general anesthesia. After the manipulation, a few hours later the woman can go home.
For many years, inflammatory processes in the uterus and its appendages occupy one of the first places in the structure of gynecological diseases. The presence of persistent pain syndrome, menstrual dysfunction, and infertility is a consequence of chronic inflammatory diseases of the uterus and its appendages and determines the relevance of this problem [2].
From the perspective of modern pathophysiology, the development of an inflammatory disease, the features of its course and the outcome of the infectious process are determined by three components: a microorganism, a macroorganism and environmental conditions [2, 3]. One of the reasons for failures in the treatment of patients with inflammatory diseases of the genital organs is the peculiarities of the relationship between a macroorganism with altered reactivity (the most important component of which is immune homeostasis) and a microorganism that has acquired new biological properties in new environmental conditions [5].
The trigger mechanism in the development of pelvic inflammatory diseases (PID) is the impact of microbial factors. Currently, the structure of causative agents of inflammatory diseases of the pelvic organs is dominated by polymicrobial flora, including both pathogenic and opportunistic microorganisms [4, 5]. Pathogenic microorganisms, the isolation of which is clearly interpreted as identifying the etiological agent, include Treponema pallidum, Neisseria gonorrhoeae, Haemophilus ducreyi, Chlamydia trachomatis, Trichomonas vaginalis
[5].
Currently, most authors note the increasing role of opportunistic pathogens, which are present in small quantities in the human body without causing disease, and only under certain conditions can become truly pathogenic [6]. Such potentially pathogenic pathogens of nonspecific PID include aerobic gram-positive bacteria of the genera: Streptococcus, Staphylococcus, Enterococcus, Corynebacterium
and aerobic gram-negative rods of the
Enterobacteriaceae family: Escherichia coli, Enterobacter
spp.,
Proteus
spp.,
Klebsiella
spp.,
Pseudomonas
spp.
Among anaerobic bacteria, gram-negative non-spore-forming bacteria of the genera Bacteroides, Fusobacterium, Prevotella
and gram-positive bacteria of the genera
Clostridium
spp.,
Peptostreptococcus, Peptococcus
[2].
As for mycoplasmas and ureaplasmas, which are opportunistic pathogens, their role in the development of the inflammatory process has not been fully determined, although most practitioners, despite the dubious etiological role of these microorganisms, recommend the use of antibacterial drugs aimed at eradicating mycoplasmas and ureaplasmas in the case of their detection in the discharge from the cervical canal.
The routes of infection into the internal genital organs are different, but the main mechanism of infection of the internal genital organs is ascending. Less commonly, a lymphogenous route from nearby pelvic organs is possible. The possibility of infection being introduced into the genital organs from distant foci by hematogenous route cannot be ruled out.
However, for the development of a picture of inflammation, in addition to the presence of the causative microorganism, additional conditions are necessary: violation of barrier defense mechanisms (anatomical and physiological features of the structure of the external genitalia, colonization resistance, acidic environment of the vagina, its ability to self-cleanse, the presence of a mucous plug of the cervical canal), violation local and general anti-infective immunity [1, 6].
Thus, the trigger for the development of exacerbation of chronic salpingo-oophoritis is the influence of a microbial factor due to the activation of opportunistic vaginal flora or the entry of an infectious agent from the outside when barrier defense mechanisms and local anti-infective immunity are disrupted.
The main place in the treatment of inflammatory diseases of the pelvic organs belongs to antibacterial agents, selected taking into account microbiological research data. Considering the polyetiological nature of inflammatory diseases of the uterine appendages, as well as the need to start treatment as early as possible, even before laboratory identification of the pathogen, doctors widely use combinations of antibacterial drugs that can eliminate the widest range of possible pathogenic microorganisms, or broad-spectrum drugs that provide a sufficient clinical effect in the form of monotherapy [7, 8].
In addition to the use of antimicrobial chemotherapy, the complex treatment of chronic PID must include drugs that prevent excessive activation of the inflammatory reaction when it is excessive and activate it when it is insufficient, with the correction of hemostasiological, hemodynamic and metabolic disorders [9].
Treatment and subsequent rehabilitation of women should be based on pathogenetic principles, taking into account the mechanisms of infection of the internal genital organs. Long-term persistence of the pathogen in the lower genital tract with an inadequate response of the immune system contributes to the chronicity of the inflammatory process. The development of subsequent exacerbations, as a rule, is associated with a violation of anti-infective defense mechanisms and with the activation of opportunistic flora.
Therefore, along with systemic drugs for the treatment and prevention of PID, the use of local drugs aimed at normalizing the vaginal microbiocenosis is justified.
The predominance of predominantly polymicrobial associations with the dominant role of opportunistic microorganisms and bacteroid anaerobes explains the fact that currently preference is given to combination drugs capable of eliminating the widest range of possible pathogenic microorganisms. One of these drugs is terzhinan, which is a combination drug containing components necessary for the treatment of bacterial (neomycin sulfate), fungal (nystatin), parasitic and mixed (ternidazole) vaginitis and colpitis. Prednisolone, which is part of it, reduces capillary permeability, helps normalize microcirculation in the vaginal mucosa, thereby improving the flow of anti-inflammatory defense components to the site of inflammation, reducing exudation phenomena, and facilitating the penetration of antibacterial drugs into tissues. Thus, the anti-inflammatory effect of prednisolone is realized, clinically manifested by the rapid disappearance of the main manifestations of the inflammatory reaction: pain, hyperemia, itching, burning. The absence of a systemic effect on the body and the need for additional use of antifungal agents to prevent candidiasis, as well as the absence of an inhibitory effect on the vaginal lactoflora, allows the use of terzhinan for the treatment of mixed infections of the lower genital tract.
The purpose of the study was to evaluate the clinical effectiveness of the drug terzhinan in the complex treatment of chronic nonspecific PID: chronic metroendometritis, chronic salpingoophoritis in combination with nonspecific colpitis, endocervicitis, bacterial vaginosis.
Material and research methods
During the work, a clinical and laboratory examination was carried out on 60 women aged 15 to 50 years with exacerbation of chronic nonspecific PID: chronic salpingoophoritis and chronic metroendometritis. In all patients, inflammatory diseases of the upper reproductive tract were combined with inflammatory processes in its lower section (with nonspecific colpitis, endocervicitis, bacterial vaginosis). The examination of patients included a medical history, general clinical laboratory research methods (general blood and urine analysis, biochemical tests), as well as bacteriological (examination of cultures from the cervical canal for flora), bacterioscopic (examination of smears of vaginal contents, urethra, anus) and instrumental (colposcopy , Ultrasound of the pelvic organs) methods.
During the study, all patients were divided into 2 groups: group 1 included 40 women who used the combined drug terzhinan (1 tablet in the vagina at night for 10 days) in the complex treatment of PID for the purpose of vaginal sanitation (1 tablet in the vagina at night for 10 days); The third group consisted of 20 women who used a topical drug containing metronidazole and miconazole nitrate.
Research results and discussion
The average age of the patients was 26.78±0.78 years. When analyzing social and everyday factors, it was revealed that 61% of women were unmarried; by professional affiliation, 34% of women were housewives, 29% were students.
The frequency of concomitant extragenital pathology was 69.00±4.65%. Noteworthy is the high percentage of concomitant diseases of an infectious and inflammatory nature: acute respiratory viral infection (65.00±7.54%) and influenza (20.00±6.32%) in the anamnesis, chronic tonsillitis (30.00±7.24% ), chronic pyelonephritis (22.50±6.60%), chronic bronchitis and pneumonia (22.50±6.60%).
Analysis of gynecological pathology showed that 65.00±4.77% of patients had a history of episodes of chronic salpingoophoritis. Disturbances of the ovarian-menstrual cycle took second place in the structure of gynecological pathology and amounted to 31.00±4.62%, manifested mainly as algodismenorrhea and oligoopsomenorea. These patients often had a history of other diseases of the genital organs of inflammatory origin: metroendometritis (13.00±1.71%), bartholinitis (2.00±1.40%) and endocervicosis (11.00±3.14%).
When studying the characteristics of reproductive function, each woman had 1.42±0.21 pregnancies (38 ended in childbirth, 23 in medical abortion, 25 in spontaneous abortion).
A history of chronic urogenital infection and vaginal dysbiosis was identified in 42 (63.41±5.35%) patients. Urogenital candidiasis was most often diagnosed (17.07±4.15%), which may be due to both a decrease in general immunological resistance and the use of antibacterial drugs during previous exacerbations. Every sixth woman was treated for bacterial vaginosis (15.00±5.64%), which is a recognized risk factor for PID. Chlamydial infection took third place and amounted to 9.76±3.28%, a history of trichomoniasis was detected in 4.88±2.38% of cases.
When analyzing complaints, patients most often noted pelvic pain of varying severity: from periodic pulling to sharp, “cutting” pain. The average temperature was 37±0.04 °C. Pathological discharge from the genital tract occurred in every second patient with inflammatory diseases of the uterus and its appendages and amounted to 74%. In addition, patients noted itching, burning in the vagina (6%), painful urination (5%).
In 20 patients, during a gynecological examination, the inflammatory process in the internal genital organs was combined with pathology of the cervix. Colposcopy revealed signs of severe focal and diffuse cervicitis in all cases.
Ultrasound signs of inflammatory diseases of the uterus and its appendages were enlarged, cystic-changed ovaries (46%), increased in diameter and length of the fallopian tubes with a thickened hyperechoic wall, which were in most cases soldered to the uterus (63%), increased size uterus, the presence of hyperechoic contents with suspension in its cavity (50%), the presence of reactive effusion in the pelvis (17%).
According to the results of a bacterioscopic examination of a vaginal smear, in most cases (87%) the inflammatory type of smear predominated: a large number of leukocytes and coccal microflora.
In 13.00±4.16% of cases, bacterial vaginosis was detected, which is one of the most common infectious diseases of the lower reproductive tract and, according to various authors, accounts for 20 to 60% of cases in women of reproductive age. Bacterial vaginosis is not accompanied by symptoms of severe inflammation and is characterized by a sharp decrease or absence of lactoflora and its replacement by polymicrobial associations of obligate and facultative anaerobic opportunistic microorganisms.
It is noteworthy that in every third woman, nonspecific colpitis and bacterial vaginosis were associated with urogenital candidiasis. According to statistics, over the past 10 years the number of vaginal candidiasis has almost doubled. At a certain stage of life, 75% of women have at least one episode of vaginal candidiasis; in 5% of women, candidiasis constantly recurs. This determines the choice of therapy, including the simultaneous administration of antibacterial and antifungal drugs.
We identified microflora in cultures from the cervical canal in 5.00±7.97% of patients; in the remaining patients there was no growth of microflora under aerobic conditions. The predominant microorganisms were Staphylococcus
spp.
(15.00 ± 5.65%), fungi of the genus Candida
(20.00 ± 6.32%), as well as
Streptococcus
spp.
(5.00±3.45%), Gardnerella vaginalis
(7.50±4.16%),
E. coli
(2.50±2.455), associations (5.00±3.45%).
Complex treatment included antibacterial monotherapy with broad-spectrum drugs (inhibitor-protected aminopenicillins, second-third generation cephalosporins) or a combination of antibacterial agents (amoxicillin/clavulanate + doxycycline; clindamycin + gentamicin, second-third generation cephalosporins - cefuroxime, cefotaxime, ceftriaxone with doxycycline or macroles ladies and metronidazole).
In addition, the components of the complex treatment included non-steroidal anti-inflammatory drugs, immunomodulators, drugs that improve the rheological properties of blood, and desensitizing agents.
In order to reduce the toxic effect of antibacterial drugs and improve treatment results, patients were prescribed multienzyme drugs and probiotics.
During the acute period of the disease, the patients received physiotherapeutic procedures such as magnetic therapy and low-frequency electrotherapy. At the second stage of treatment, the use of ultrasound and low-pulse laser effects, which have a fibrolytic effect, was practiced.
The dominance of polymicrobial associations, including both aerobic, obligate and facultative anaerobic opportunistic microorganisms, and yeast fungi of the genus Candida
, dictates the need to prescribe, along with systemic antibacterial therapy, complex local agents, of which terzhinan is a representative.
According to a clinical and laboratory study, the effectiveness of terzhinan therapy was 87.7%, which was manifested by normalization of the degree of purity of vaginal contents, subjective and objective improvement, which was characterized by the disappearance or reduction of discharge from the genital tract, and in 12.3% of cases these indicators significantly improved compared with those before treatment (see table).
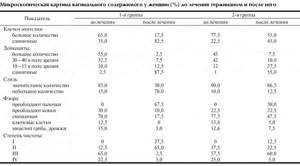
The dynamics of clinical symptoms when using Terzhinan included the disappearance of vulvar itching on average on the 5th day of treatment, relief of pain in the area of the vaginal vestibule - on the 2nd, normalization of the nature of discharge - on the 6th day. By the end of the course of treatment (on the 10th day), all patients had no complaints. Of the 40 patients with nonspecific colpitis, according to a microbiological study, cure was found in 34. In addition, all patients had an increase in the number of lactobacilli without additional use of eubiotics.
In group 2, the disappearance of these symptoms occurred 1-2 days later, and in some cases the pathological symptoms resumed on the 9-10th day and later (see figure).
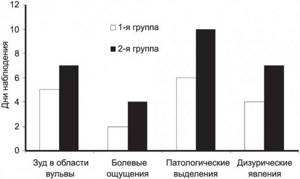
Figure 1. Time frame for relief of the main clinical manifestations of inflammatory diseases of the lower reproductive tract during treatment in the examined groups. In 12 out of 20 patients, treatment was found to be ineffective, which required an additional anti-inflammatory course of treatment.
Side effects of terzhinan were observed in 2 patients in the form of unexpressed short-term burning sensations, and only on the 1st-2nd day after application.
Among the patients of group 1, 12 had concomitant pathology of the cervix, in group 2 - 8. According to the results of colposcopy, signs of focal and diffuse cervicitis were revealed in patients of both groups. A cytological study, allowing to assess the structure and cellular level of tissue damage, was carried out after anti-inflammatory treatment.
In the group where terzhinan was used, there was no questionable cytological evidence of the presence of intraepithelial neoplasia; In no case was additional anti-inflammatory treatment required. In group 2, 5 out of 8 patients, due to incomplete relief of the inflammatory process in the cervical tissues, had difficulties with the differential diagnosis of intraepithelial neoplasia and inflammatory changes, which required an additional course of vaginal sanitation.
Thus, a decrease in local immunological resistance of the lower genital tract, characteristic of the chronic course of the inflammatory process, contributes to the disruption of normal colonization resistance of the vagina, serves as a source of ascending infection of the internal genital organs and is the main factor in the development of exacerbation. Antibacterial therapy, which is an integral part in the treatment of exacerbation of infectious processes in the internal genital organs, in turn, is accompanied by the development of dysbiosis of the vaginal flora. Thus, one of the vicious circles in the pathogenesis of exacerbation of PID is closed. Local use in complex treatment of a broad-spectrum antibiotic, a metronidazole component that affects anaerobic flora, and an antifungal drug not only promotes vaginal sanitation, but also prevents the development of bacterial vaginosis. The role of prednisolone as one of the components of terginan is significant, which allows normalizing microcirculation in the vaginal mucosa, promotes the influx of anti-inflammatory defense components, optimizes the delivery of drugs to the site of inflammation, and ensures the maintenance of normal flora in the vagina.
conclusions
The combined local drug terzhinan, along with systemic antibacterial chemotherapy drugs, immunomodulators, drugs aimed at combating hemodynamic and metabolic disorders, as well as degenerative processes in the tissues of the uterus and its appendages, is the drug of choice in the complex treatment of inflammatory diseases of the pelvic organs.
Indications for hysteroscopy
The following symptoms and diseases are indications for the procedure:
- Heavy, painful menstruation
- Uterine bleeding
- Infertility
- Endometriosis
- Endometrial hyperplasia
- Suspicion of synechia
- Myoma
- Polyps
- Inability of a woman to carry a pregnancy to term
- Suspicion of cancer
- Clarifying the location of the intrauterine device and its removal
- Examination of the uterus after surgery
- Removing the remnants of the fertilized egg after termination of pregnancy
Pain after hysteroscopy
The pain occurs most often in the lower back and abdomen. Hysteroscopy is performed using a device whose diameter is no more than 3 mm. The insertion of the hysteroscope probe is almost painless, but after the manipulation, slight nagging pain will appear. If it hurts after hysteroscopy, which was performed for diagnostic purposes, then such pain goes away a few hours after the manipulation. Minor discomfort may be felt for several days. If the pain does not go away within several days, if severe pain occurs, this is a reason to consult a doctor for help. To avoid pain after this procedure, you should refrain from sexual intercourse for several days, do not lift anything heavy, do not take a hot shower, bath, or go to the sauna or bathhouse.
Preparation for hysteroscopy
On the eve of hysteroscopy, the patient undergoes a gynecological examination. It allows the doctor to determine the condition of the vagina and cervix. The gynecologist also takes a smear from the vagina for bacteriological and cytological examination. Also, the woman must provide the results of a general blood and urine test, coagulogram, determination of blood group and Rh factor, RW, the presence of antibody titres to hepatitis C and B, as well as the causative agent of HIV (AIDS). An electrocardiogram is taken and fluorography is performed on her. After this, the patient is examined by a therapist, who, if necessary, prescribes consultations with specialized specialists.
In order to avoid complications of the postoperative period after hysteroscopy, I recommend that a woman follow these rules:
- do not use vaginal suppositories, tablets and sprays for one week preceding the procedure;
- refrain from intimacy for two days before hysteroscopy;
- do not drink alcohol on the eve of the examination;
- stop taking medications that are not recommended by your doctor.
Depending on the presence of a particular pathology, hysteroscopy is performed at different phases of a woman’s menstrual cycle. If the procedure is prescribed to diagnose uterine fibroids, then the study must be carried out a few days after the end of menstruation. In the second phase of the cycle, a study is carried out to diagnose endometriosis and identify the causes of infertility.
Discharge after hysteroscopy
As after any intervention in which the instrument comes into contact with the mucous membrane, discharge appears due to injury to the mucous membrane of the cervical canal and uterine cavity. After such an operation, discharge is considered normal. The discharge is bloody, not profuse, and lasts for several days. If the discharge is profuse, painful, or the color of the discharge has changed, you should immediately consult a doctor. If diagnostic hysteroscopy is performed, the discharge is most often scanty and passes quickly. If surgical hysteroscopy is performed, the discharge will be more abundant for several weeks. Often after such an intervention, hemostatic drugs are prescribed. The doctor is often asked the question: “When will menstruation occur if hysteroscopy is performed?” Discharge after the procedure may smoothly transition into menstruation, but in most cases, menstruation occurs on schedule for every woman. In rare cases, it is slightly delayed.
Course of the postoperative period
In most cases, hysteroscopy is quite easily tolerated by patients. Diagnostic hysteroscopy is rarely accompanied by uterine bleeding or pain. It does not require any rehabilitation measures.
After surgical hysteroscopy, the patient requires medical supervision for some time. She is prescribed anti-inflammatory combination drugs to prevent bacterial infections. Additionally, the doctor evaluates the nature of the discharge after hysteroscopy. Most often they are bloody and scanty, and after some time they stop on their own.
To relieve pain in the perineum or lower abdomen, doctors recommend that patients take non-opiate painkillers in the first days after hysteroscopy. Analgesics can be taken only in case of severe pain. Minor pain that may occur after hysteroscopy goes away on its own within a couple of days.
A woman after hysteroscopy should follow the following recommendations:
1) refrain from coitus for a couple of weeks after hysteroscopy; 2) for the same period of time, stop using tampons and vaginal suppositories; 3) refrain from taking a bath, visiting a bathhouse, sauna, or swimming in a pool.
After hysteroscopy, the polyp grew again
What to do if the polyp grows again after surgery? Polyps often appear due to hormonal imbalance in a woman’s body. Removing a polyp does not guarantee the cessation of their formation elsewhere in the uterine mucosa. Endometrial polyps are a disease characterized by the proliferation of the basal (inner) layer of the endometrium. The most common cause of the development of polyps is an excess of estrogen, a lack of progesterone; abortion, premature termination of pregnancy, and childbirth with incomplete delivery of the placenta can also cause the growth of polyps. It is possible to develop polyps after stress, with diseases: diabetes, thyroid disease, hypertension. Chronic inflammatory processes in the female genital area and a sharp drop in immunity play a negative role. If the polyp has grown again, you should be tested for sex hormone levels. When hormone levels are disrupted, polyps will reappear even after surgery. In this case, treatment with OCs (oral contraceptives) is prescribed, which will affect hormonal levels and stop the development of polyps. If hysteroscopy was used to remove a polyp, bloody discharge will persist for several days. You should monitor the condition of the discharge - it should not be abundant, change color, or have an unpleasant odor. If such symptoms appear, consult a doctor immediately.
Consequences of the procedure
Despite the fact that hysteroscopy is considered a gentle method of treatment, complications also develop with its use. After this, the consequences are as follows:
- Perforation of the uterus
- Bleeding
- Side effect of anesthesia
- Endometritis
Consequences in the form of uterine perforation rarely occur; most often, such a complication arises due to the low qualifications of the doctor, as a result of perforation of the uterine wall with a hysteroscope.
Consequences in the form of bleeding occur due to various causes and factors; if heavy discharge occurs, a woman should urgently consult a doctor.
Consequences in the form of endometritis or inflammation of the uterus arise due to an infection introduced during the procedure, due to an inflammatory process that was not treated before the procedure.
Consequences in the form of a hematometer develop due to uterine spasm during the procedure.
Also, a complication after the procedure is considered to be an incompletely removed polyp, a myomatous node, which is rare.