Computed tomography (CT) with contrast is a highly accurate diagnostic method that involves introducing a special iodine-containing drug into the patient’s body. Contrast is administered directly during scanning of the area under study intravenously using an injector (special pump). The substance blocks X-rays, which allows for more accurate visualization of soft tissues, arteries and veins, “coloring” them from the inside in response to exposure to X-rays.
The drug is non-toxic, safe for the patient’s body and is eliminated within 24 hours.
On CT scans with contrast, the boundaries of tissues of various morphologies are clearly visible, the slightest structural deviations from the norm are visible - the images are more detailed, and the information content of the study increases.
Additional contrast is necessary only in certain situations, for example, when there is a need for primary differential diagnosis of neoplasms (if oncology is suspected), monitoring the results of oncology treatment (surgery, chemotherapy), when assessing the vascular bed and venous patency. Your doctor will be able to determine whether a CT scan with contrast is appropriate. For some diseases of the thyroid gland and kidneys, and during pregnancy, the administration of a contrast agent is carried out for health reasons.
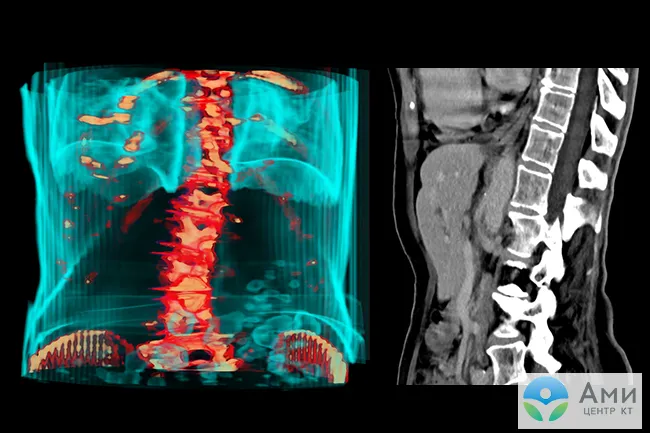
Vessels - arteries and veins - can only be examined on a CT scan with contrast. Before vascular operations, in the presence of pronounced pathological changes, such as malformations, stenosis, atherosclerotic plaques, this type of diagnosis is considered the “gold standard”.
When is a CT scan with contrast performed?
Most often, a CT scan with contrast is prescribed by the attending physician, or the patient undergoes an examination to monitor changes in the size of the tumor after treatment or the progress of recovery after surgery.
However, there are situations when, during a survey computed tomography without contrast, a radiologist notices a suspicious lump or neoplasm. In this case, to clarify the results of the first examination, the size of the tumor and its specifics, the patient is recommended to undergo a repeat CT scan with contrast.
Since the drug is safe, if there are no contraindications, you can undergo a CT scan with contrast without a doctor’s referral.
CT with contrast is preferred in the following situations:
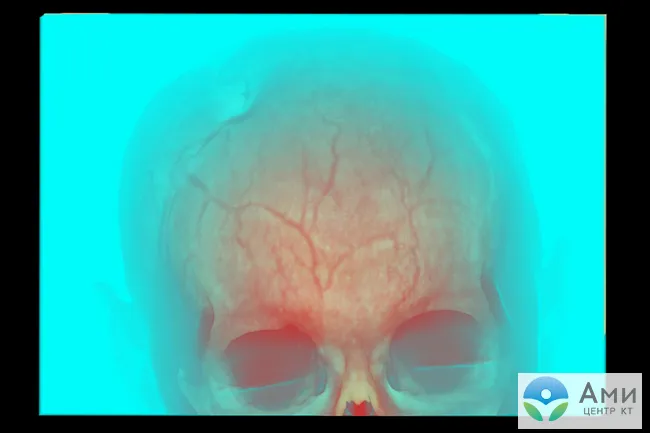
- Examination of the vascular system and deep veins - using three-dimensional cross-sectional tomograms, a radiologist examines vessels for damage, malformations, stenosis (pathological narrowing of the lumen), atherosclerotic plaques, and calcifications. CT scanning of blood vessels with contrast is called “angiography”. The study has important prognostic value, as it allows timely detection of predictors of stroke, thrombosis and tumors that compress blood vessels.
- If cancer is suspected / to assess the dynamics of tumor growth / to assess the results of surgical removal of a tumor or chemotherapy - computed tomography with contrast can detect even small malignant tumors. Cancer cells can grow and divide when they receive enough oxygen and nutrients. Therefore, blood circulation at the site of a growing tumor is usually more intense, and the texture of the tissue is denser, but the opposite situation also occurs when metastases are hypovascular in relation to the surrounding tissues. On CT scans with contrast, oncology has a special “pattern”, and the tumor itself is painted in a lighter color. A radiologist will be able to assess the size of the tumor and give an initial differentiated conclusion, that is, to distinguish a cancerous tumor from a cyst, benign lipoma, etc. To clarify the diagnosis, the patient in this case also needs to submit a tissue sample for laboratory histological examination (biopsy).
CT scan with contrast is always prescribed for suspected cancer:
- Abdominal organs (liver, kidneys, intestines, gall bladder);
- Organs of the chest (lungs, larynx, heart, mediastinum);
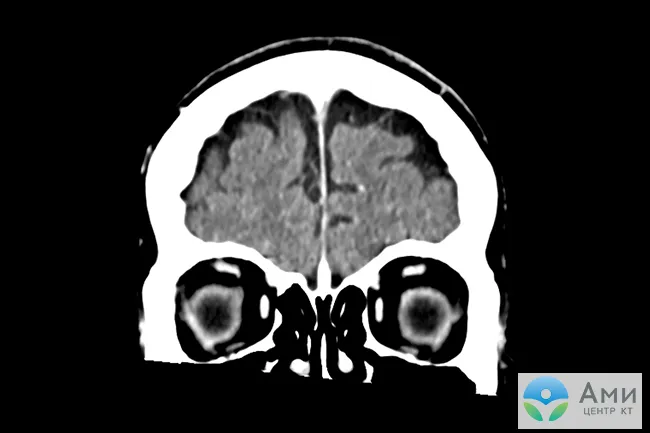
- Brain;
- Soft tissues of the supporting apparatus (muscles, ligaments).
- If metastases are suspected , CT with contrast can identify malignant cells that have migrated from the cancer site to other organs and tissues through the bloodstream and lymphatic vessels.
- For diseases that result in damage to soft tissues and internal organs - CT of the brain, CT of the neck (for diagnosing lymph nodes), CT of the abdominal cavity is best done with contrast.
- Unclear or complex clinical picture - to clarify the results of other studies.
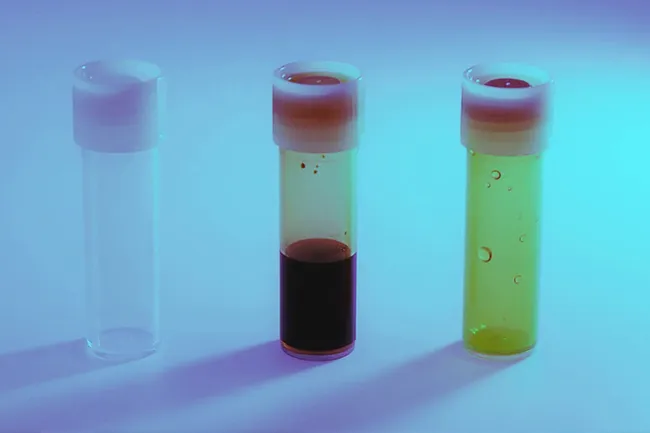
What contrasts are used for CT
As a rule, various iodine-containing preparations are used to increase the contrast of the resulting image. All of them are divided into two groups - fat-soluble and water-soluble. Medicines of the first group are very viscous, so their use is limited. They are administered only locally, for example, into the peritoneal cavity to identify fistulas, etc. If we are talking about computed tomography with bolus contrast (the drug is administered into a vein with a special injector) or about the drug being administered orally, water-soluble contrast is used. The toxicity of such drugs is several times lower, and they also quickly enter the blood vessels.
What does a CT scan with contrast show?
A CT scan of the brain with contrast is performed in patients who have had a stroke. It is recommended to undergo the examination immediately after the first signs of acute cerebrovascular accident in hemorrhagic stroke appear. The consequences of an ischemic stroke are assessed after 4-5 hours. On a CT scan of the head with contrast, tumors and vascular pathologies, including aneurysms, malformations, cavernomas, and hemangiomas, are visualized more clearly and distinctly than on MRI.
CT scan of the neck with contrast allows you to examine lymph nodes, tumors of the soft tissues of the neck and larynx.
A chest CT scan with contrast shows the thoracic aorta. The examination will show pulmonary embolism (PE) and lung tumors. To assess the respiratory organ in tuberculosis and pneumonia, it is enough to do a CT scan without contrast.
Abdominal CT with contrast is recommended in the vast majority of cases. In addition to pathologies of internal organs (urolithiasis, cholelithiasis, pancreatitis, enlarged lymph nodes), the diagnosis will show the abdominal aorta and other abdominal arteries, post-traumatic disorders and tumors: liver, kidneys, pancreas, spleen.
A CT scan of the pelvis with contrast is performed to examine the lymph nodes, but for examining internal organs, preference is given to other methods - ultrasound, MRI, etc.
A CT scan of soft tissues with contrast shows tumors - a radiologist will be able to assess the size of the tumor and clarify its specifics, however, for a correct diagnosis, the following conclusion must be given by a histologist.
CT angiography with contrast
Computed tomography of the vascular bed or CT angiography is the main study that allows you to evaluate the patency and functionality of blood vessels. The most popular scans are the aorta, coronary blood flow, neck and head. It is this examination that allows us to identify pre-stroke risk factors and is carried out for patients with symptoms of acute cerebrovascular accident, if a stroke is suspected.
CT angiography shows damage to vascular and venous walls, tumors, malformations, aneurysms, cholesterol plaques, deposits of calcium salts, stenosis, thrombosis - any pathological disturbances of blood flow. CT angiography is performed only with contrast, since without “staining” the study is uninformative. The examination is also prescribed to patients before surgical interventions, in particular, before vascular operations, for example, to remove malformations.
In what cases is contrast used in MRI?
Main indications for MRI with contrast:
- Suspicion of the presence of metastases of any location. Such “in-depth” MRI makes it possible to identify even small “screenings” of tumors, assess the prospects of their removal, and conduct dynamic monitoring against the background of antitumor therapy.
- The need to clarify the nature of the detected neoplasm, differential diagnosis between benign and malignant tumors.
- Examination of the spinal cord and brain in patients with suspected or already diagnosed multiple sclerosis.
- Differential diagnosis of infectious and inflammatory foci of unspecified etiology, signs of generalized infection.
- Examination of the mammary glands and prostate gland (for some pathologies).
The doctor may recommend using additional contrast for targeted examination of identified formations and foci of any location, if the MRI performed according to the basic program turned out to be insufficiently informative.
What types of contrast agents are there?
Today, medical institutions use various ionic and non-ionic preparations containing iodine. It is iodine that makes scans more contrasty and rich, and there is no harm from its entry into the body. The effective amount of contrast agent is calculated based on the patient's weight.
Our center uses a non-toxic and absolutely safe non-ionic contrast agent “Omnipaque” , which is quickly and almost painlessly administered as a bolus using an injector. In the case of an abdominal CT scan, the patient is given an additional contrast drink.
Patients with endocrine diseases of the thyroid gland, in particular hyperthyroidism, should consult an endocrinologist - the administration of an iodine-containing drug may be extremely undesirable. It is also necessary to make sure that you are not allergic to iodine, the main component of contrast. But before you do a home test, be careful - some patients, even when applying iodine to the crook of the elbow, may have an unpredictable reaction, even anaphylactic shock.
Preparing for a CT scan with contrast
CT without contrast does not require special preparation. Before scanning with contrast, you should adhere to the following algorithm:
- Make sure you are not allergic to iodine.
- Read the list of absolute and relative contraindications to CT with contrast.
- No more than 10 days before diagnosis, check the functionality of the kidneys (they are responsible for removing the drug from the body) by taking a blood test for creatinine.
- Patients with thyroid diseases (especially hyperthyroidism) and diabetes mellitus should consult an endocrinologist.
- At least 3 hours before the test, refrain from eating.
For more information about the preparation algorithm for CT of the pelvis and CT of the abdominal cavity with contrast, read the links on the corresponding pages of our website.

On the day of the CT scan
On the day of your CT scan, you can eat and drink as usual.
Before the scanning procedure
- You may have to change into a hospital gown before your CT scan.
- If you are using oral contrast material, you will start taking it before the test.
- If you receive intravenous contrast: Your healthcare team will ask you: if you have kidney disease;
- whether your kidney function is impaired;
- have you had kidney surgery;
- do you have diabetes?
- whether you are taking metformin or a medicine that contains metformin (such as Glucophage®, Glumetza®, or Janumet®).
During the scanning procedure
When it is time for your procedure, a technician will take you into the office and help you lie down on the machine table for scanning. The CT machine looks like a huge donut with a hole in the middle. This is a diagnostic scan ring. There is no tube like in an MRI scanner. As you lie down on the table, the table will slowly pass through the diagnostic scan ring. When going through the ring, you must lie absolutely still until the scanning process is completed.
After the technician takes the first series of pictures, you will have a contrast agent injected into your IV catheter or CVC. You may feel warm and have a slight metallic taste in your mouth. If you feel pain where the IV catheter was inserted, or have symptoms such as itching, swelling, dizziness, or have trouble breathing or feeling lightheaded, tell your nurse.
The CT scan procedure takes less than 30 minutes.
After the scanning procedure
- If you had an IV catheter, your nurse will remove it and apply a bandage to the insertion site. You can remove the bandage after 1 hour if you are not bleeding.
- If you feel unwell or have questions or concerns, talk to your doctor or technician.
- Tell your nurse if you have any of the following symptoms: itching;
- rash;
- dizziness;
- breathing problems;
- feeling weak or faint;
- swelling or discomfort in the area around the IV catheter site.
How is a CT scan with contrast performed?
The patient comes to the examination in comfortable clothing, removes metal jewelry and removable medical devices, and then lies down on the couch. The X-ray technician installs a syringe injector to administer contrast. The drug begins to act by circulating through the circulatory system, then the scan begins, which lasts less than 1 minute.
The tomograph table moves inside a frame (gantry), on which rows of sensitive sensors are installed that record the response of tissues and internal organs of the scanned area. The sensors rotate along a spiral path. In our center, the CT with contrast procedure (MSCT) is performed on a modern multislice tomograph Siemens Somatom go.Now with reduced radiation exposure.
In just a few seconds, the tomograph takes multiple slice-by-slice scans. High-resolution images are processed on a computer to create a three-dimensional model-reconstruction of internal organs and blood vessels. The study is recorded on a DVD.
The CT scan procedure with contrast lasts 15-20 minutes, taking into account the administration of the drug.

After CT scan with contrast
Some patients worry on the eve of the study. There is no need to be afraid of a CT scan with contrast - the examination is quick and in most cases absolutely without discomfort. After the administration of contrast, the patient feels warmth throughout the body - this is a normal reaction of the body to the rapid introduction of fluid into the vascular bed. To ensure that the contrast agent is eliminated from the body faster, it is recommended to drink more water after the examination. The drug is excreted naturally within 1-2 days.
Immediately after a CT scan with contrast, the patient receives a recording of the study in excellent quality on disk. The radiologist will prepare a report and send it to the patient by email.
How is contrast agent administered?
Contrast-enhanced computed tomography involves several ways to administer a contrast agent. The method chosen will depend on what exactly needs to be inspected. Contrast can be injected orally, into a vein, rectally, into an organ, or even into the lesion itself. It is worth taking a closer look at the most common methods.
Oral route
This method is most often used when examining the gastrointestinal tract; in this case, the patient must drink the drug according to the recommendations specified in the instructions. The medications are quickly absorbed, significantly increasing the clarity of the image of the mucous membranes of the stomach and allowing you to see polyps or narrowings. Often combined with intravenous contrast.
Intravenous administration
CT using intravenous contrast involves several types of injection of a substance into the body. Namely:
- Before the procedure, a nurse will inject the drug into the patient’s vein;
- first, a regular CT scan is performed, then the computer tomograph is stopped, contrast is injected into the patient’s vein, and the procedure continues with a contrast agent;
- the substance is administered as a bolus using a special syringe or a dropper if you need to administer the drug slowly.
Computed tomography with intravenous contrast is most often performed.
Into the lumen of the cavity
In such a situation, fat-soluble substances are used to determine the presence of diverticula, fistulas and other abnormal formations. Sometimes when examining hollow organs (for example, the bladder, colon), contrast is injected into them before the procedure begins. The harm of CT with contrast will be slightly higher, since fat-soluble compounds are more toxic than water-soluble ones. But, nevertheless, problems with removing the substance from the body do not arise if all the doctor’s recommendations are followed.










