A single lesion in the lungs (SLP) is defined as a local area of compaction of lung tissue of a round or similar shape with a diameter of up to 3 cm [15]. This international definition differs from the traditional domestic concept of pulmonary lesions, the source of which is phthisiatric practice (in the classification of pulmonary tuberculosis, the size of lesions does not exceed 1 cm, and larger lesions are defined as infiltrates, tuberculomas and other types of changes) [14, 15].
Pathological formations of the lungs of small size (up to 2 cm) in most cases are detected during computed tomography of the chest, performed for various reasons [10, 11, 14, 16-18].
Some characteristics of space-occupying lesions on CT allow us to judge their nature - benign or malignant, but they are not decisive when making a diagnosis [19]. The nature of the formation can also be judged by the rate of its growth [20].
Meanwhile, based on the results of one CT study, it is often difficult to make a differential diagnosis; repeated studies over time are required. During the inflammatory process, the lesions disappear after 1-2 months. In the case of atypical glandular hyperplasia, the lesions do not change for several years. In adenocarcinoma, increased size and/or increased density as well as vascular convergence may be seen [11, 12].
Focal formations in the lung tissue discovered during such an examination often remain unattended by specialists, which sometimes leads to disappointing results of treatment for this category of patients.
The difficulties of accurately diagnosing focal lung formations are well known - differential diagnosis most often has to be made between peripheral cancer, benign tumor (hamartochondroma, etc.), tuberculoma, sarcoidosis, and metastatic lesions of the lung [1-4, 6, 7, 10, 12].
According to S.V. Miller et al. [8], diagnostic thoracotomy is the final method of comprehensive examination of patients with small round lung formations and provides truly early diagnosis and timely surgical treatment. Consequently, radical surgical intervention undertaken for a round formation in the lung, the genesis of which is unclear, is a method that allows for morphological verification of the early stage of a malignant tumor and performing organ-preserving surgery.
Other authors believe that currently there is no unified approach to determining the nature of focal lung formations. Obviously, with a high risk of a malignant tumor, the optimal approach is the earliest possible morphological verification of the diagnosis. In case of low risk of malignant process, it is more rational to carry out dynamic observation [11].
The result of these actions may be the identification of a group of patients with an obviously benign process, as evidenced by the absence of growth dynamics of the lesion for 2 or more years, the presence of “benign” calcifications, inclusions of fat (hamartoma) or fluid (cyst) in the lesion according to CT data. In such a situation, only observation is necessary. This also includes cases of arteriovenous malformations and other vascular changes, as well as inflammatory processes in the lungs (round tuberculous infiltrate, tuberculoma, mycetoma, etc.), requiring specific treatment [5, 9, 13].
The second possible result is the detection of signs of a malignant process (a lesion with a diameter of more than 1 cm with radiant uneven contours, lesions of the ground glass type and mixed solid type, which should be regarded as potentially malignant), for which morphological verification is necessary in a specialized medical institution [12] .
Every year in Russia over 63 thousand people, including over 53 thousand men, become ill with lung cancer. In more than 20 thousand patients (34.2%), lung cancer is detected at stage IV, so the task of detecting malignant lung tumors in the early stages of their development is extremely relevant [2, 7, 8].
A threatening factor when diagnosing small-diameter lung tumors is their asymptomatic nature. The absence of complaints, the meager clinical picture of the disease, difficulties with prevention and primary detection of lesions make the problem of lung formations up to 2 cm in diameter relevant for scientific research and practically significant for preserving the health and often the lives of patients.
Dark spot on x-ray
In fact, the presence of dark spots in the lungs, visually visible on x-rays, does not in 100% of cases indicate the development of various ailments. Other organs are also localized at the level of the lungs, so that the radiation beam, while passing through the body, will project on film an image of all organs, as well as tissues that fall within its range.
Only a doctor can determine exactly what a spot on the lung found on an x-ray is. Sometimes additional tests are required to make a valid diagnosis.
If, during a routine annual fluorography, doctors discover a spot on a patient’s X-ray, this does not become a reason for immediate hospitalization in a tuberculosis clinic or for compulsory treatment. A patient with such a disorder is shown a detailed X-ray examination, when photographs of the chest are taken in various projections. This allows you to determine an accurate diagnosis.
Sometimes spots in the image are explained by natural causes - an error in the X-ray machine or poor-quality film. Also among the relatively safe causes of such darkening are scar changes after surgical interventions, abscesses and diseases.
What does a shadow on a lung x-ray mean?
Abnormal X-rays are sometimes serious and sometimes not. One of the most concerning, yet all-too-common findings on a chest x-ray is what is called a lung shadow. Although we may assume that this means something serious, it is not really a diagnosis, but an observation of an abnormality that is not clearly defined and requires further investigation. While certain distinguishing features may indicate what it is, additional tests are needed before a definitive diagnosis can be made. After all, a shadow on a lung could mean something serious or mean nothing at all. Consider this the first step towards diagnosis.
What could a black focal spot mean?
They speak of focal spots when small nodules are detected on an x-ray of the lungs - about 1 cm, no more. Such traces can be explained by:
- Vascular disorders.
- Primary stage of cancer. Such lesions usually have clear contours.
- Many diseases of the respiratory organs. In particular, during inflammatory processes, the contours of the lesions are unclear.
- Post-myocardial infarction.
On an x-ray, only 1 lesion may be visible, but sometimes several of them are recorded, even at a significant distance from each other. So, if dark spots of this kind are localized in the upper parts of the lung, most likely they indicate tuberculosis. And multiple foci in a limited space may indicate focal pneumonia.
What does focal change mean?
The focal spot or focal shadow on a fluorogram has a round shape. The area of such a trace is often more than 10 - 12 mm. This darkening is most often recorded during an inflammatory process, possibly resulting from:
- Pneumonia.
- The presence of fluid in the pleural tissue (localized effusion).
- Parasitic diseases (with the formation of eosinophilic infiltrate).
- Development of bronchial asthma.
- Formation of a localized abscess.
However, it is worth noting that the focal spot can also be a sign of tumor formations of various etiologies. Sometimes this phenomenon is observed after rib fractures in the projection of the formation of bone calluses.
What disease causes lobar spots?

Lobar darkening usually has clear contours, which are clearly visible on the fluorogram. Such spots are distinguished by a certain convexity or concavity and most often indicate the presence of various chronic pulmonary ailments.
Among the most common causes of lobar shadows are:
- Cirrhosis.
- Bronchiectasis.
- Formation of a purulent cavity.
Lobar opacities can be seen very well and diagnosed with detailed CT scans.
Segmental opacities
Such spots on the lungs visually appear on x-rays as segmented areas with fairly clear contours and usually have a triangular shape. The appearance of isolated darkenings of this kind can be provoked by:
- Previous injuries to lung tissue.
- Formation of endobronchial tumor.
- Entry of foreign bodies.
However, the presence of several segmental changes is considered a rather alarming symptom and can be observed with:
- Inflammations of varying severity, which have an acute or chronic form.
- Cancer diseases.
- Tuberculosis.
- Stenosis of the bronchial branch.
- Metastasis.
Atelectasis of the lung or x-ray semiotics of triangular spots on the image
Lung atelectasis is a disease accompanied by the collapse of a segment, lobe or lung tissue completely against the background of cessation of bronchial ventilation. Radiologically, such changes are called limited darkening, since they do not extend beyond the segment or subsegment and have a triangular shape.
Atelectasis of the middle lobe of the right lung - frontal and lateral radiographs
How to identify atelectasis in an image:
- the size of the spot coincides with the size of the changed segment;
- triangular darkening in the lungs can be seen in frontal and lateral projections;
- during inhalation photographs the size of the spot does not increase;
- the narrow end of the triangular shadow is directed towards the root;
- Holtzknecht-Jacobson symptoms are observed during fluoroscopy (suction of the mediastinum towards the lesion during exhalation).
The morphological substrate of the pathology is the accumulation of infiltrative fluid in the alveoli, infiltration of lung tissue, and tumor growth in the pulmonary parenchyma.
Spontaneous atelectasis occurs in 1-3% of patients due to a defect in surfactant (the substance that forms the framework of the alveoli).
Schematic representation of the topography of segmental atelectasis
Limited darkening during collapse of the lungs requires knowledge of the segmental structure of the lungs, as it reflects atelectasis of a certain segment. By establishing the topography of the shadow, the doctor can guess which bronchus is affected. The substrate of formation (infiltrate, additional tissue, exudate) is almost impossible to determine on the basis of a radiograph.
Round shadow syndrome

Doctors talk about round shadow syndrome when an X-ray of the lungs in various projections reveals a round or oval spot. To accurately determine the cause of this phenomenon, the doctor first evaluates the type of darkening:
- A round-shaped spot most often has intrapulmonary formations, for example, tumors, cysts, as well as infiltrates with inflammatory content.
- Oval-shaped spots are formed when round formations are compressed by the pulmonary walls.
- Heterogeneous shadows on the spot are a sign of decay of necrotic tissue (in patients with oncology or tuberculosis infiltrate) or the formation of a cavity.
- Slightly darker areas often indicate incomplete calcification of tuberculoma.
- The presence of a clear and dense edge is a possible sign of an hydatid cyst.
It is worth considering that only spots larger than 1 cm in size are considered round shadows. The remaining darkening is considered focal.
CT diagnosis of lung cancer
PREVALENCE OF LUNG CANCER AND RISK FACTORS
Lung cancer, a tumor of the bronchial epithelium, is one of the most common cancers in the world. Every year, more than 10,000 thousand people in Russia are diagnosed with malignant neoplasms of the respiratory system, and in the world this figure is even higher. Bronchogenic malignant tumors are one of the most common causes of death from cancer and the most common type of oncopathology of the tracheobronchial tree.
Risk factors for lung cancer include:
1) Living in environmentally unfavorable areas.
2) Work in industries associated with inhalation of dust particles, metals, paint fumes and active chemicals, even with protective equipment. The most unfavorable is inhalation of asbestos dust, then coal dust, as well as vapors of heavy metals, arsenic, chlormethyl ether, chromium, and mustard gas.
3) Tobacco smoking is the main predisposing factor for neoplasms of the tracheobronchial tree. In active smokers, the risk of developing cancer is up to 10 times higher than in non-smokers, and in passive smokers - up to 2 times.
4) Specific diseases. There is a direct connection between tuberculosis, asbestosis, silicosis, other diseases manifested by diffuse or local pneumosclerosis, and malignant neoplasms of the bronchi.
MANIFESTATIONS OF LUNG CANCER - WHEN CAN YOU SUSPECT THE DISEASE?
In order not to miss the first signs and symptoms of lung cancer, you must pay attention to the following changes in your health: the appearance of a cough with sputum streaked with blood, a sharp loss of weight for no apparent reason, an increase in body temperature, especially in the form of “peaks” accompanied by chills , increased sweating.
A direct indication for CT is the detection of a clearly focal shadow in the image during fluoroscopy or radiography. Of course, lung cancer on X-ray does not look very specific - after all, similar changes can also be caused by tuberculosis, other benign tumors, and even pneumonia. All these conditions can be differentiated using CT.
Get MSCT of the lungs in St. Petersburg
HOW TO DETECT LUNG CANCER?
X-ray for lung cancer reveals a rounded shadow on the left. For the purpose of differential diagnosis (to distinguish lung cancer from tuberculoma, cyst or pneumonia), it is necessary to perform computed tomography - CT.
The most effective diagnostic method for lung cancer is multislice computed tomography (MSCT). In most cases, contrast is not necessary to see the tumor on CT scans. Contrast enhancement is used mainly in the diagnosis of central tumors in order to distinguish a small soft tissue node in the root of the lung from the pulmonary vessels located nearby. CT is an indispensable method for determining the size of the tumor, the extent of damage to the root of the lung, mediastinum and chest, and assessing damage to the lymph nodes. All these details ultimately determine the stage of the cancer process, so accurate analysis of the results of computed tomography is extremely important for prognosis.
Another tomographic research method, magnetic resonance radiography (MRI), is almost never used for diagnosing pulmonary tumors, as it poorly detects changes in lung tissue. The fact is that lung tissue contains a large amount of air, which does not give a signal on MRI.
Ultrasound examination (ultrasound) also cannot reliably diagnose changes in lung tissue, however, this method can be used to detect changes in the surrounding pleura.
X-ray and fluoroscopy can be used to detect pulmonary formations, but the isolated use of these methods does not allow a reliable diagnosis. Bronchography as a way to detect lung cancer is also a thing of the past.
Among the instrumental methods for diagnosing central tumors, fibrobronchoscopy (FBS) is very good - an endoscopic method, thanks to which you can not only see the narrowing of the bronchial lumen with your eyes, but also take part of the space-occupying lesion for histological examination. HISTOLOGICAL CLASSIFICATION OF LUNG CANCER AND SURVIVAL PROGNOSIS
According to the histological classification of bronchogenic cancer of the latest revision (from 1999), 6 types of tumors of the tracheobronchial tree are distinguished:
1) Adenocarcinoma - detected in approximately 35% of all cases. Most often, this is a peripheral tumor that looks like a single (solitary) node of various sizes with typical signs of malignancy, with the presence of spicules - radiant edges, which are formed due to the growth of cancer along the lymphatic vessels; areas of necrosis, decay and hemorrhages in the tumor stroma. Adenocarcinoma metastasizes often and early. The prognosis is very variable, largely depending on how early the formation was detected.
2) Squamous cell non-keratinizing cancer is a common variant - up to 35% of all cases of lung tumors. It has the best prognosis and rarely metastasizes. In approximately 65% it develops in one of the central bronchi and causes a picture of atelectasis on CT and x-rays, in 35% it develops in the peripheral bronchi and looks like a solid single node, often with a decay cavity in the center, similar to an abscess.

The patient was diagnosed with a cancerous node in the 6th segment of the lower lobe on the left. After resection, squamous cell lung cancer was verified by histological examination. Tomography in this case did not give a typical picture of a malignant neoplasm.
3) Small cell cancer is the most aggressive and most dangerous type; already in the early stages it can metastasize to the lymph nodes of the roots of the lungs and mediastinum. The life expectancy of patients with such neoplasms varies depending on the stage (TNM) and the possibility of surgical treatment. Frequency of occurrence up to 20%. It usually arises from the epithelium of large bronchi and causes a picture of atelectasis. Closely related to smoking.
4) Large cell undifferentiated cancer - rare, less than 5% of cases. It is usually presented by one solid peripheral node of large size. Almost always occurs in smokers. It metastasizes early - hematogenously and lymphogenously, the prognosis for it is unfavorable.
5) Large cell neuroendocrine cancer (carcinoid) - often central, with a characteristic feature - disintegration in the tumor, occurs in less than 5% of cases, metastasizes early to the lymph nodes, is aggressive, and has an unfavorable course.
6) Bronchiolo-alveolar cancer – up to 2%. It is a subtype of adenocarcinoma. Almost always peripheral. It manifests itself as a diffuse decrease in the density of the pulmonary parenchyma of the “ground glass” type, which simulates the picture of pneumonia. It also manifests itself as changes in the type of consolidation - diffuse compaction of the pulmonary parenchyma, which may look like a node. The prognosis for small node sizes is usually favorable.
WHAT DOES LUNG CANCER LOOK LIKE ON COMPUTED TOMOGRAPHY?
There are several options for the growth of a tumor node (according to Rosenstrauch):
1) Into the lumen of the bronchus on one side, narrowing it - endophytic type.
2) Into the lumen of the bronchus, circularly narrowing it - this is also an endophytic type.
3) Into the lumen of the bronchus and outwards from it - a mixed type of growth.
4) Along the wall of the bronchus, without narrowing its lumen - peribronchial type.
When a tumor grows into the lumen of the bronchus, it narrows, which leads to a violation of the ventilation of a certain area of the lung tissue. With a CT scan, you can directly notice the tumor node itself in the lumen of the bronchus - it looks dense (white). The lumen of the bronchus is narrowed in a circle, parietally, or “breaks off” at the border with the neoplasm. You can also see an increase in the density of the corresponding lobe (or segment, segments) ventilated by this bronchus. An increase in density can be caused by atelectasis - collapse of a section of lung tissue as a result of obstruction of the bronchial tube, distelectasis - partial collapse, as well as changes caused by pneumonia, most often of a stagnant nature, with abscess formation, as well as pneumofibrosis.
Get a CT scan of the lungs in St. Petersburg
There is also a division of lung cancer into peripheral and central - the classification of the latter is given above. Central cancer is clinically more severe due to the fact that it often gives complications in the form of atelectasis, massive pneumonia, abscess formation, and respiratory failure.
CT signs of central lung cancer: computed tomography reveals a volumetric formation of the soft tissue structure, in which the lumen of the lower lobe bronchus “breaks off”. The edges of the formation are tuberous, uneven, with spicules, and the shape is irregular.

Central lung cancer on CT. Note the differences in the width of the lumen of the central bronchi on the right and left. The lumen of the right upper lobe bronchus is not visible. Atelectasis of the upper lobe is visible. In the circle is the tumor itself, which caused atelectasis.
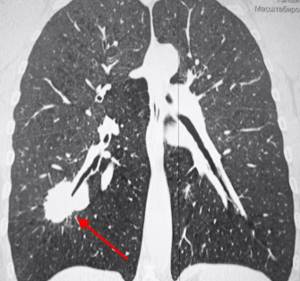
Peripheral lung cancer on CT looks like a focus or node located on the periphery of the organ far from the root. It usually has a homogeneous structure, in some cases with areas of necrosis, calcifications and hemorrhages into the parenchyma. The edges of a typical cancerous tumor are uneven, with multiple “spicules” due to lymphangitis. When located near the pleura, the formation deforms it and pulls it towards itself. Its dimensions vary - from the focus (3-10 mm) to the node (10-50 mm and more).
Typical peripheral lung cancer (adenocarcinoma) on MSCT. On the right, in the 6th segment of the lung, a dense soft tissue node with spicules was identified, deforming and pulling the interlobar pleura towards itself.
Much less common is primary multiple cancer, which must be differentiated from metastases and other diffuse and disseminated foci, including tuberculosis. There are also diffuse forms of tumors - bronchiolo-alveolar cancer (BAR), manifested on CT in the form of a total or subtotal decrease in pneumatization like “ground glass” - they need to be differentiated from pneumonia, pulmonary edema.
STAGES OF LUN CANCER ACCORDING TO TNM AND MOUNTAIN
Staging of lung cancer is necessary to determine whether the tumor can be removed.
At stages T1 and T2 according to Mountain, surgery is possible. Stage T3a means that the tumor may be resectionable (most often a pneumonectomy is necessary); stages T3b and T4 mean that it cannot be removed surgically.
In the absence of metastases to regional lymph nodes or in the presence of altered lymph nodes only on the affected side (TN0 and N1, respectively), surgical treatment is possible and the prognosis is most likely favorable. At stage N2, surgical treatment is possible after radiation and (or) chemotherapy; the prognosis is questionable. For N3, surgical treatment is not indicated. Detection of metastases to distant organs also significantly worsens the prognosis.
The table shows the classification of lung cancer according to the TNM scale (UICC, 1999).
| Stage ( TNM) | Criteria |
| T1 | A tumor node in the lung parenchyma up to 3 cm in largest size without signs of growth into the wall of the central bronchi. |
| T2 | An intrapulmonary tumor larger than 3 cm or a tumor infiltrating the wall of the main bronchus at least 2 cm below the bifurcation zone or a tumor growing into the visceral pleura. Atelectasis of a lobe or segment, but not total. |
| T3 | A tumor of any size infiltrating the main or intermediate bronchus less than 2 cm from the bifurcation or growing limitedly into the mediastinal pleura, mediastinum, or chest wall. Total atelectasis or obstructive pneumonia may be detected. |
| T4 | Tumor of any size with invasion into the mediastinum, pericardium, aorta, superior vena cava, brachiocephalic vein, bones, chest wall. Effusion into the chest cavity. Satellite foci (intrapulmonary metastases). |
| N0 | There is no damage to regional lymph nodes. |
| N1 | Damage to the root lymph nodes, bronchopulmonary lymph nodes on the side of the tumor. |
| N2 | Damage to the bifurcation, paratracheal, paraesophageal, para-aortic lymph nodes of the mediastinum on the side of the tumor. |
| N3 | Damage to the lymph nodes of the root, mediastinum on the side opposite to the tumor; damage to the axillary, sub- and supraclavicular, scalene lymph nodes. |
| M0 | There are no distant metastases. |
| M1 | Distant metastases (including intrapulmonary foci) were detected. |
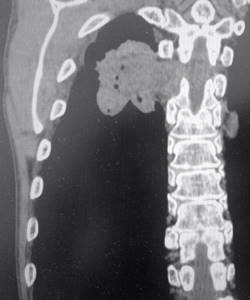
An example of stage 4 lung cancer. Surgery is not indicated, only chemotherapy. Invasion occurs into the ribs and spine, as well as into the soft tissue of the chest wall. In the stroma of the tumor, multiple hypodense (dark) areas containing gas are visible - zones of decay.
CAN WE CURE LUNG CANCER?
Can lung cancer be cured? Yes, but only if detected early at stages T1 and T2. Unfortunately, the further the tumor is located from the large bronchi, the longer the time it can remain undetected, especially if the patient “forgets” about timely fluorographic examinations.
CT CT FOR LUNG CANCER AND SECOND OPINION
An important stage in the diagnosis of pulmonary oncological diseases is the analysis of CT results with the accurate identification of all signs that influence the staging of the tumor and the choice of surgical tactics. Given the high cost of error, such testing should be performed by a professional radiologist who specializes in diagnosing pulmonary diseases. Unfortunately, sometimes the interpretation of CT results is not at the proper level. In this case, the CT results recorded on a CD can be sent for review to a more experienced specialist and a Second Opinion can be obtained. In our country, any patient faced with the need to review the results of a computed tomography scan can turn to Second Opinion services, for example, the National Teleradiological Network.
Vasily Vishnyakov, radiologist
Read more about Second Opinion
Read more about telemedicine
Pavel Popov
Candidate of Medical Sciences, Member of the European Society of Radiologists
Ring shadow syndrome
A ring-shaped spot found on an X-ray of the lung is considered by doctors to be one of the simplest diagnostic cases. Most often, such darkening is a consequence of the formation of a cavity filled with air. At the same time, taking pictures in different projections confirms the closure of the ring in all positions of the patient’s body. Features of ring-shaped spots contribute to the correct diagnosis:
- A large and uniformly thick contour indicates an inflammatory process, for example, with a tuberculous cavity (less often with an abscess).
- Unevenly wide boundaries of the ring-shaped shadow are a symptom of the disintegration of a cancerous tumor.
A visually noticeable ring in the image is also recorded in case of extrapulmonary phenomena, for example, deformation of the lungs, accumulation of gases in the intestines or pleural cavity.
Reading x-ray or scan
It can be helpful to think of radiology studies (which include X-rays, CT scans, and MRIs) as images in shades of black, white, and gray.
Dense or hard structures such as bones, the heart, and large blood vessels appear white. In contrast, air-filled structures such as the lungs will appear black. Overlapping structures or anything in between will appear in grayscale. X-ray scans are sometimes difficult to read because the structures overlap, and even if you find an abnormality, it may be difficult to determine what it is. While some abnormalities may be defined by structures such as a mass, nodule, or tumor, in other cases their appearance may not be as well defined. In this case, we can call them damage, stain or shadow.
Undefined changes

Spots on the lungs, which have an indefinite shape, can indicate various ailments:
- Inflammatory lesions caused by staphylococci.
- Pleural effusion.
- Heart attack.
- Exudative pleurisy.
Sometimes shapeless spots are a consequence of hematogenous infection of the lungs from existing purulent foci (for example, when a patient develops osteomyelitis, andexitis, etc.). In this situation we are talking about quite dangerous secondary staphylococcal pneumonia.
Total blackout - what is it?
When a spot on an X-ray image extends to 2/3 of the lung field or more - sometimes even to the entire organ, doctors record a total darkening. There may be gaps in the upper or lower region of the lung. A similar picture can be observed if there is no air in the pulmonary cavity or the tissue over its entire surface has become denser. Also, total darkening occurs in the presence of fluid or other pathological contents inside the pleural cavity.
Total blackout is possible with:
- Cirrhosis.
- Atelectasis.
- Exudative pleurisy.
- Pneumonia.
To fully interpret the X-ray results, the doctor not only evaluates all visually noticeable pathological elements, but also takes into account the individual anatomical characteristics of the patient.
What to do if a white spot is detected on the x-ray
When performing a chest x-ray or fluorography in a patient with tuberculosis, a white spot on the x-ray reflects either an inflammatory lesion of the lung tissue or destructive changes in the parenchyma with the formation of abscesses, tubercles, and caverns. Correctly, this symptom should be called darkening, since it reflects the characteristics of the passage of x-rays through objects and their color display on the x-ray.
A white shadow in a photograph is also observed when:
- pneumonia;
- atelectasis;
- exudative pleurisy;
- occupational diseases (silicosis, talcosis, asbestosis).
Radiographs with white spots of various origins: 124.3 – breast piercing, 124.4 – shot in the soft tissues of the chest, 124.5 – professional cementosis, 124.6a – contrast during bronchography, 124.6b – pneumonic focus, 124.7 – interlobar pleurisy (arrows indicate artifact)
This syndrome is a sign of many pathological changes in the lungs, but we will look at the most common options.
If spots are detected, additional research is necessary to determine the cause of the pathology. For these purposes, a radiologist may prescribe an X-ray examination in additional projections or perform layer-by-layer computed tomography or magnetic resonance imaging.
How does cancer appear on an image?

Lung cancer is not always visible on X-rays. In particular, if the size of the tumor does not exceed 2 mm, the tumor will simply be invisible. For early diagnosis to be truly successful, doctors recommend taking x-rays in several projections at once. Cancer in the image can be suspected by:
- Shadows on the edges of the lung, which is distinguished by blurry and tuberous borders.
- The presence of a thin border of rays near the focus.
- A visible white spot against the background of the shadow.
Of course, cancer can also manifest itself with other signs, which only a competent specialist can detect in an image. At the slightest suspicion of oncology, the patient is advised to conduct additional studies.
What to do if you find it?

Most often, chest radiography cannot be a sufficient basis for a final diagnosis. Detection of dark spots on an x-ray is a reason to conduct a whole range of different studies:
- MRI and CT.
- Bronchography.
- Biopsies, etc.
The image is interpreted by a radiologist. He can make a preliminary diagnosis, which is later confirmed or refuted by the attending physician. It is simply impractical to draw conclusions about existing stains on your own.
What does a spot look like on an x-ray with pneumonia?
In pneumonia, the spot on the x-ray image has a length depending on the size of the lesion in the pulmonary parenchyma:
- limited – up to 3 cm in diameter;
- segmental – within a segment;
- subtotal – the entire field, with the exception of the tops;
- total.
Pneumonia is an inflammatory disease that affects the alveolar tissue with accumulation of fluid in the acini. Pathogenesis forms a specific x-ray picture of the disease.
X-ray. Focal pneumonia in the lower lobe on the right
The white spot with pneumonia has fuzzy, blurred contours. Its intensity can be low or high, depending on the characteristics of the exudate (inflammatory fluid in the lumen of the alveoli). A path from the root approaches the site of its localization due to lymphangitis.
Treatment
Of course, not a single doctor in the world treats spots on the lungs. Therapy depends on the detected disease and the individual characteristics of the patient:
- Tuberculosis is a reason to undergo long-term anti-tuberculosis treatment using several strong antibiotics. The closed form of the disease can be successfully treated at home, while the open form is treated only in a tuberculosis clinic.
- Pneumonia is most often also treated with antibiotics, but in addition, the patient is shown targeted therapy designed to support the body, relieve intoxication and facilitate recovery.
- A detected effusion in the pleural cavity (fluid accumulation) may not be treated in any way if it is asymptomatic. Most often, it resolves on its own with successful treatment of the underlying disease. However, sometimes the fluid needs to be removed by drainage.
- Cancer diseases require complex treatment aimed at suppressing the activity of pathogenic cells and reducing tumor size. Sometimes doctors decide to remove a lobe of the lung to save the patient’s life.
There are quite a few bronchopulmonary diseases, the development of which may cause spots to appear on the images. Treatment methods for such ailments most often differ and are selected individually by the attending physician.