Pulmonary emphysema (derived from the Greek “bloating”) is a pathological condition that is characterized by the expansion of air spaces distal to the terminal bronchioles and is accompanied by destructive changes in the walls of the alveoli. Emphysema is a component of chronic obstructive pulmonary disease (COPD).
- Epidemiology
- Classification
- Causes
- Pathogenesis
- Pathomorphology
- Symptoms and diagnosis
- Treatment of emphysema
- Forecast
- Prevention
Causes
Any cause that leads to chronic inflammation of the alveoli affects emphysematous changes, especially if there is a deficiency of antiproteolytic factors. Smoking causes low-grade inflammation in the airways. Therefore, proteolytic enzymes are constantly or recurrently released from leukocytes. Secondary emphysema occurs in patients with COPD, which indicates a severe course of the disease.
Risk factors for emphysema:
- environmental pollutants
- occupational hazards
- long-term use of certain medications
- infectious respiratory tract diseases
Alpha-antitrypsin deficiency is a genetic factor that predisposes to the development of emphysema. Because of this, the sensitivity of lung tissue to autolysis by its own proteases increases. Smoking leads to a faster development of the process.
For your information:
Over the past 20 years, bronchial obstruction has been given such importance in the etiology of emphysema that it has been repeatedly suggested that the diagnosis of emphysema should be reserved for cases where a causal relationship with chronic bronchitis has been established. However, emphysema, leading to severe respiratory failure, can develop without a previous disease of the airways, i.e., it can be primary. Insufficient knowledge of the problem has prompted many researchers to consider emphysema as one of the independent forms of nonspecific pulmonary pathology.
Telephone
Pathogenesis
The key point in pathogenesis is the destruction of lung tissue fibers, which is caused by an imbalance in the proteolysis-antiproteolysis systems. Some researchers believe that fibroblast dysfunction also plays a role. With alpha-antitrypsin deficiency, the activity of neutrophil elastase increases, which breaks down collagen and elastin, causing the destruction of respiratory tissue.
The destruction of the alveolar walls and supporting structures leads to the formation of greatly expanded air spaces. Researchers believe that the absence of a tissue frame in the lower respiratory tract leads to their narrowing due to dynamic collapse during exhalation at the level of small lung volumes. Also, the destruction of the alveolar-capillary membrane reduces the diffusion capacity of the lungs by reducing the respiratory surface area.
Pathomorphology
Emphysema is a destructive process of the elastic framework of lung tissue, as noted above. With proximal acinar emphysema, the bronchiole is larger than normal in size, and its integrity is also compromised. Proximal acinar emphysema is divided conditionally into centrilobular and emphysema in miners' pneumoconiosis. In the first form, changes occur in the respiratory bronchiole proximal to the acinus. This form of emphysema occurs mainly in the upper lobes of the lungs. In miners' pneumoconiosis, focal emphysematous areas alternate with interstitial pulmonary fibrosis.
In panacinar emphysema, which is also known as generalized emphysema, there is a uniform pattern of changes involving the acinus. Initially, the pathological process affects the alveolar ducts and sacs. Later, the boundaries between them disappear. This emphysema is localized mainly in the lower lobes of the lungs. The course of the disease is severe.
In the distal acinar form of emphysema, the process affects the alveolar ducts. The irregular form is characterized by a variety of enlarged acini and their destruction, while a scar process is expressed in the lung tissue. This form of emphysema occurs in the following diseases:
- sarcoidosis
- pulmonary tuberculosis
- eosinophilic granuloma
- histoplasmosis
- pneumoconiosis
Bullous emphysema is marked by the formation of emphysematous areas of the lung ranging from 1 centimeter in size. Most often, the disease is congenital and resolves with spontaneous pneumothorax.
Types of chest deformation
Chest deformities can be divided into two groups.
- Congenital - usually caused by a violation of skeletal development in the prenatal period (changes in the shape of bones, absence of elements of the chest walls): - funnel-shaped deformity of the chest; – keeled chest deformity; – flat chest deformity.
- acquired (more common) - are the consequences of injuries, lung diseases, bone tuberculosis, rickets, scoliosis: - emphysematous; – paralytic; – scaphoid; – kyphoscoliotic.
Symptoms and diagnosis
Symptoms become more pronounced as the disease progresses. Over time, shortness of breath progresses. Most often it manifests itself when the patient is over 50 years old. It intensifies when respiratory infections occur. Sputum when coughing is mucous, in small quantities, because with emphysema there is no bacterial inflammatory process.
Usually the patient loses weight because his respiratory muscles become more tense. In most cases, the history includes smoking, chronic or recurring respiratory diseases, and occupational hazards. Several generations of direct relatives may experience various diseases of the respiratory organs, which doctors call familial lung weakness. In bullous emphysema, recurrent spontaneous pneumothoraxes are recorded.
Physical examination
Upon examination, doctors note that the chest has a cylindrical shape. Her mobility during breathing movements is limited. Accessory muscles are actively involved in breathing. Percussion sound over the entire surface of the chest has a boxy tint. The lower borders of the lungs are shifted downwards by 1-2 ribs, their mobility is limited.
Auscultation reveals weakening of breathing, wheezing appears with concomitant chronic bronchitis during a cough test, auscultation in a lying position, forced exhalation. Heart sounds are better heard in the epigastric region.
Instrumental studies
X-ray examination reveals that the mobility of the diaphragm is limited. Increased airiness of the lung fields is recorded. The diaphragm dome is low and flattened. There are few vascular shadows in the pulmonary fields. Increased pulmonary pattern can be found in bullous emphysema. Using radiography, it is possible to detect a characteristic complication of the bullous form of emphysema - spontaneous pneumothorax.
Computed tomography confirms the depletion of the vascular pattern of the pulmonary fields and increased airiness of the lungs. The method is also relevant for determining the presence, location and size of bullae. At the onset of the disease, you may find that the lung size is higher than normal. In severe cases of the disease, the surface area of the lungs decreases. The study gives doctors the ability to non-invasively determine lung weight and volume.
FVD study is a highly informative diagnostic method for suspected pulmonary emphysema. The flow-volume curve reveals obstruction of the distal segment of the respiratory tree in the early stages. In emphysema there cannot be reversible obstruction.
Laboratory research
A general blood test for pulmonary emphysema will not show inflammatory changes. They can only occur if a person has another disease along with emphysema. Severe emphysema is characterized by progressive hypoxemia, which leads to polycythemic syndrome: the content of red blood cells and hemoglobin in the blood increases, and blood viscosity increases.
Complications
Complications include the development and progression of irreversible respiratory, pulmonary and heart failure. Emphysema can cause an emergency such as spontaneous pneumothorax, especially valvular pneumothorax, in which pressure builds up inside the chest.
Differential diagnosis
Secondary emphysema requires differential diagnosis from primary emphysema and from forms of the disease that are caused by expansion of the air spaces of the lungs without involving the vascular bed. The secondary form can be, for example, in chronic obstructive bronchitis or bronchial asthma.
Primary emphysema is found in young and middle-aged patients; it can often be found in 2 or more relatives. The diagnosis is confirmed by finding a low concentration of alpha-antitrypsin in the blood serum. With secondary emphysema, symptoms of another disease that has affected the lower respiratory tract may appear.
The involutive form of emphysema is caused by the expansion of the air spaces of the lungs (as are hypertrophic and involutive). It does not cause hypoxia, broncho-obstructive syndrome, or hypercapnia. In the hypertrophic form, which is also known as compensatory or vicarious, the volume of the remaining lung increases, which indicates a compensation process. Acute bloating of the lungs is a reversible compensation reaction during aspiration of a foreign body with incomplete bronchial obstruction, a severe attack of bronchial asthma, drowning, and sometimes during sudden physical overload.
What can be seen on an x-ray with emphysematous changes
Pulmonary emphysema
To diagnose pulmonary pathology, it is necessary to analyze images in two projections: a plain X-ray of the chest organs and a lateral projection, usually of the right side.
With pulmonary emphysema, the radiologist detects the following changes in the lungs on x-ray:
- horizontal position of the ribs;
- barrel-shaped chest;
- expansion of intercostal spaces;
- the sternum deviates forward;
- kyphotic curvature of the thoracic spine;
- increasing the transparency of lung tissue;
- displacement of mediastinal organs (heart, esophagus, great vessels);
- expansion and destructuring of the roots of the lungs;
- omission of the diaphragm;
- strengthening of the pulmonary pattern mainly in the hilar zone - expansion of the pulmonary vessels;
- prolapse (sagging) of the diaphragm towards the abdominal cavity, mainly on the left;
- an increase in the diaphragmatic angle (from acute to direct).
With a long course of the disease, emphysema is complicated by the formation of bullae - air cavities in the lung. When tension increases when coughing or sneezing, tissue rupture is possible with the formation of a closed pneumothorax.
Treatment of emphysema
There are currently no specific treatment measures for this disease. Therapeutic programs are relevant, as with all COPD. It is necessary to eliminate the factors that caused the development of emphysema. This may be a chronic infectious process in the respiratory tract, exposure to dirty air, smoking, etc.
Drug treatment includes taking drugs to dilate the bronchi:
- salbutamol or fenoterol
- M-anticholinergics
- formoterol or salmeterol
- combination of the above drugs
- long-acting theophylline preparations
For older people, it is better to prescribe m-anticholinergic drugs. Theophyllines are almost never relevant for them.
Glucocorticoids are effective in severe pulmonary emphysema. Prednisolone is prescribed in short courses of prednisolone up to 20-30 mg orally with a rapid dose reduction and discontinuation of the drug over 7-12 days. It is necessary to monitor the effectiveness of therapy using the flow-volume curve. If the effect is not achieved, then the patient does not need to give any more GCs. If systemic GCs have a positive effect, it is best to continue using inhaled medications. For example, budesonide 400-500 mcg 2 times a day is effective.
Replacement therapy with human alpha-1 antitrypsin may provide the desired effect, especially if there is a genetic predisposition to the disease in question. But to date, none of the drugs in this series has been introduced into clinical practice.
Acetylcysteine has an antioxidant effect. 600 mg is prescribed orally, taken once a day before bedtime.
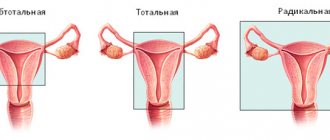
Surgical treatment consists of reducing lung volume. A bullectomy is performed, preferably a thoracoscopic one. Resection of peripheral areas of the lungs is performed, so the remaining areas are decompressed. The functional state of the lungs improves. Doctors are also trying to introduce the method of lung transplantation, including in the CIS countries. When spontaneous pneumothorax develops, drainage of the pleural cavity and air aspiration are used.
Recommendations for air travel
Pneumothorax is a complication of bullous transformation of the lungs. Air travel poses a certain risk for these patients because at an altitude of 2.5 km, the cavities in the lungs containing air can increase by 38-40%. This expansion can lead to bulla rupture and pneumothorax.
To be fair, episodes of pneumothorax during air travel are rare and there are no categorical bans on flying patients with bullae in the lungs.
If pneumothorax occurs 7-14 days before the flight, air travel should be postponed.