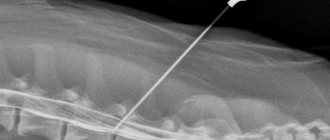
MR scanning of the sacroiliac joints (coronal projection) Magnetic resonance imaging is a highly informative and safe way to diagnose many diseases. Thanks to MRI, it is possible to study the most complex internal organs and structures, including the spinal column, surrounding soft tissues, spinal cord, etc. The method is used in vertebrology, traumatology and orthopedics. There is no preparation for MRI of the lumbosacral spine and other areas. But it is important to know how the study is carried out, take into account existing contraindications, and take medical documentation with you to the procedure.
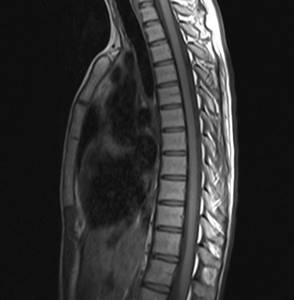
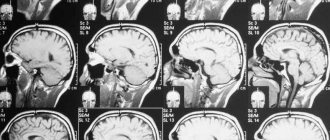
Magnetic resonance imaging of the thoracic spine in sagittal projection
What is MRI of the lumbosacral spine?
A study using a modern magnetic resonance imaging scanner is one of the most effective ways to non-invasively diagnose the spine. Tomography is an absolutely safe form of diagnosis for the patient. This examination is carried out using a magnetic field and radio frequency waves without the use of ionizing radiation. The operating principle of an MRI device is based on the physics of nuclear magnetic resonance, when hydrogen atoms in the cells of the human body begin oscillatory movements in response to electromagnetic pulses. This resonance is captured by the tomograph and based on it, three-dimensional images of the scanned area are built.
Indications
The patient can voluntarily schedule an MRI of the lower back. It makes sense to do this if you feel that:
- pain in the lower back spreads to the sacrum and pelvic area, has long become chronic, and no therapeutic measures relieve it;
- not only does it hurt in the lower back, but also your legs go numb, your calves and toes are cramped;
- suffer from partial paralysis resulting from injuries to the lumbosacral spine;
- pulled or injured the lumbar spine;
- have already been diagnosed with hernias of the lumbar spine and need to regularly monitor their behavior.
How often should an MRI of the lumbosacral spine be done?
Given the absolute safety for health, MRI of the lumbosacral spine can be performed as often as required. Therefore, with its help, the doctor controls the effectiveness of the treatment process in order to achieve 100% results. The recommended frequency of tomography for preventive purposes is once every 2 years for all patients over 35 years of age.

Previous Next
Why do you need an MRI?
A frequently asked question for doctors is why do you need an MRI, aren’t tests enough? What does it show? And can it harm the body, because it’s radiation? The MRI itself is a special test that helps the doctor obtain images of the organs and bones of the body, this gives a complete picture of what is happening inside a person. This way, the cause of pain in different parts of the body is determined, and MRI of the cervical spine is useful after serious accidents and injuries that affected the neck.
The doctor will see how the vertebrae are restored and whether everything is going correctly. In fact, patients most often undergo MRI after accidents or domestic injuries, when the sacrum, neck or back is damaged. Resonance tomography shows this clearly.
Magnetic radiation does not cause any harm to human health.
What will an MRI of the lumbosacral spine show?
Often an MRI of the lumbar spine is prescribed if necessary:
- examine the anatomy of the lumbosacral spine for congenital defects and developmental anomalies;
- detect a possible cause of chronic pain in the lumbosacral region, including narrowing of the spinal canal and the development of lumbosacral radiculitis;
- assess the condition of the lumbar vertebrae (degenerative changes, bulges, intervertebral hernias);
- examine spinal injuries to detect damage to bones, ligaments and intervertebral discs, vascular bed, as well as damage to the spinal cord;
- for the diagnosis of infectious lesions of the discs and spinal cord in the lumbosacral region;
- to identify tumors and abscesses, as well as degenerative changes in soft and bone tissue.
Using magnetic resonance imaging, diseases such as:
- multiple sclerosis;
- Bekhterev's disease;
- osteoporosis;
- spinal cancer;
- intervertebral hernia;
- kyphosis, scoliosis, radiculitis;
- Scheuermann-Mau disease;
- lumbodynia and lumbago, sciatica;
- stenosis.
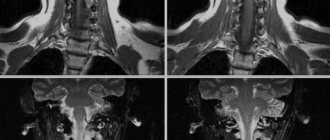
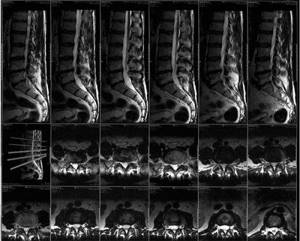
The lumbosacral spine on an MRI image
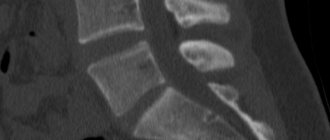
Indications for lumbar CT scan
A referral for examination can be obtained in the following cases:
- abnormalities of the spine;
- spinal deformity;
- determination of bone tissue density (densitometry);
- narrowing of the spinal canal;
- acute and chronic spinal injuries;
- oncological diseases: confirmation of changes detected on x-rays, determination of the size, location of the primary tumor and metastases, stage of the tumor process;
- chronic pain in the spine that does not go away after a standard course of treatment;
- herniated intervertebral discs;
- tumors of the spine and surrounding soft tissues, metastases of tumors to the spine from other organs;
- tuberculous spondylitis (inflammation of the vertebrae);
- osteomyelitis;
- malformations (vascular anomalies);
- preparation for spinal surgery;
- monitoring the condition of the spine after treatment (radiation or chemotherapy).
Advantages
- MRI diagnosis of pathological abnormalities of the lumbosacral region is a non-invasive procedure, that is, it does not require instrumental intervention.
- The magnetic field of the tomograph does not injure tissue, does not cause pain or cause discomfort.
- MRI does not use harmful x-rays to examine the spine, as is the case with x-rays and computed tomography.
- MRI images can detect any tissue pathology long before it can be noticed by symptoms, which is successfully used in the early diagnosis of spinal tumors and significantly increases the chances of recovery.
Initial appointment with a NEUROLOGIST
ONLY 1800 rubles!
(more about prices below)
What does it feel like during an MRI?
The procedure is completely painless. After all, a person cannot physically feel the influence of magnetic waves. Some may feel discomfort from being in a dark and cramped tomograph scanner, and the table is most often hard and cold. Therefore, immediately ask for a blanket and pillow, because the procedure takes almost an hour, sometimes more.
A working CT scanner typically makes a loud buzzing noise, so staff may provide special earplugs for the patient to muffle the sounds. There is also a constant connection between the patient and doctors inside the scanner. It supports the entire scanning procedure. Also, some modern tomographs even have a TV or special headphones so that the patient can pass the time faster.
Doctors warn people (whether women or men, regardless of gender) to move less while lying inside the tomograph. Any unnecessary movement may subsequently affect the MRI of the vertebral or sacral region
For medical reasons, some cannot stay in one position for a long time. You can ask for a sedative injection. You can eat and drink after the scan and lead your usual lifestyle. There is no recovery period.
Procedure
MRI of the spine is a fairly fast scan. In the non-contrast case it takes 10-20 minutes; the introduction of contrast increases the duration of the study to 40 minutes. MRI, like ultrasound, is one of the safest research methods. Unlike computed tomography, during it there is no harmful radiation effect on the human body.
The scanning procedure itself is as follows. The patient is invited to the diagnostic room, where he is placed on a tomography table. You will need to lie on your back with your legs extended. Then the table is moved inside the scanning part of the tomograph. The doctor leaves the room and starts the screening program from the adjacent control room. The patient will understand that the device is working by a series of noises reminiscent of tapping.
It is important not to move during the examination. The quality of the resulting tomograms depends on this. The tomograph is very sensitive to movement. And if you do not comply with the requirements of stillness, the pictures will turn out blurry, and the diagnosis will be uninformative.
- MRI
- Ultrasound

MRI tomograph:
Siemens Magnetom C
Type:
Open (expert class)
What's included in the price:
Diagnostics, interpretation of images, written report from a radiologist, recording of tomograms on CD + free consultation with a neurologist or orthopedist after an MRI of the spine or joint

Ultrasound machine
HITACHI HI VISION Avius
Class:
Expert (installation year 2019)
What's included in the price:
Diagnostics, interpretation of images, written diagnostic report
Tomography of the spine and spinal cord
Unlike common diagnostic methods, MRI allows you to identify diseases of the spine at the initial stage, assess the condition of the skeletal system and the soft tissues located around it, tendons, lymph nodes, blood vessels, cartilage tissue of the joints, and interdisk space. The study makes it possible to identify incipient foci of inflammation, tumors in the formation stage, and the penetration of metastases of malignant neoplasms into the spinal cord and surrounding tissues.
When is an MRI of the spine prescribed?
MRI helps to evaluate spinal diseases:
- Osteochondrosis and its complications in the form of hernia formation.
- Changes in the spinal column after injuries and tumors.
- Curvature of the spine: kyphosis, scoliosis, lordosis.
- Bacterial, fungal, viral damage to the spinal substance, multiple sclerosis.
- Infringement of the nerve endings of the spine.
- Changes in vascular circulation.
- Congenital pathologies.
- The appearance of pain in the spine of unknown origin.
Vertical diagnostic method
How to do an MRI with axial load:
- after tomography of the spine in a horizontal view, the table, together with the patient and the magnet, rises to a vertical position;
- gravity begins to act on the spinal column - the vertebrae shift under the load of the human body;
- disorders in the form of a hernia become more pronounced;
- The level of instability of the organ is determined if it is required to securely fix it. The information is used by neurosurgeons for traumatic lesions of the skeletal system.
The results of the MRI study are assessed by a neurologist. Images are prepared within 1-2 hours after the examination. The patient awaits the result; if necessary, another series of images is taken. Since the procedure does not have a harmful effect on the body, there is no need to worry about health complications after the diagnosis.
source
Contraindications
There are a number of contraindications to magnetic resonance imaging of the lumbosacral spine that you need to know and remember:
- Firstly, this is the presence of metal products in the body that cannot be removed or removed before diagnosis. In the lumbar region, metal is incorporated into the body extremely rarely. In most cases, these can be plates after serious injuries, stents on blood vessels, or hip replacements.
- Secondly, the presence of pacemakers, built-in hearing aids and other life support devices.
Braces, crowns, dental implants, tattoos, permanent makeup, cosmetic implants and fillers are not a contraindication for MRI of the spine.
MRI of the lower back during pregnancy
MRI is not contraindicated in pregnant and breastfeeding women. However, pregnant women are not recommended to undergo a tomography examination using contrast. The effect of a contrast agent on the formation and development of the child’s central nervous system has not been fully studied.
Questions about diagnostics
Dress code
You can enter the MRI room in any clothing that does not contain metal. When going to the clinic, it is best to wear loose, non-restrictive clothing without metal elements (zippers, rivets, hooks), in which you can lie comfortably. For women, we recommend bringing a T-shirt or not wearing a bra with metal wires or hooks.
Preparation
This tomography does not require any preparatory steps from the patient.
Is MRI harmful to health?
MRI is a completely harmless diagnostic method for the human body. This method of examination can be carried out at any age and for any disease an unlimited number of times, unless you have contraindications.
Contraindications
Some pacemakers and foreign objects in the body may pose serious limitations to tomography. In particular, cochlear implants, vascular clips, stents, heart valves and insulin pumps, pacemakers, neurostimulators, steel screws, staples, pins, plates, joint endoprostheses may be a contraindication to diagnosis. The patient must notify the radiologist about all implanted objects in the body. The diagnostician will be able, based on information about the composition and model of the implant, to assess the possibility of conducting diagnostics.
If you are having an MRI with contrast, be sure to report any allergies to medications or kidney problems. It is also necessary to inform the radiologist about a possible pregnancy.
Is it possible to do an MRI with braces and dental implants?
Dental implants and crowns are not a contraindication to magnetic resonance imaging. The magnetic field does not have any negative effect on them. Fixed brace systems can produce artifacts on tomograms during MRI of the head. If the light effect is too strong, the doctor will stop the study and offer the patient alternative diagnostic methods.
Is the device noisy?
Any MRI machine in working condition makes noises reminiscent of tapping. The open tomograph is one of the quietest installations. The noise from its operation is significantly lower compared to closed tomographs. If the sounds of the operating unit cause you anxiety, you will definitely be offered special noise-canceling headphones.
What should I do if I have claustrophobia?
An open tomograph is the optimal solution for patients suffering from panic attacks in a closed space. It is open on the sides on three sides and does not create a claustrophobic feeling.
Can I take sedatives before an MRI?
If you are a little nervous, before the tomography you can take mild sedatives, for example, valerian, motherwort infusion or afobazole. Taking sedatives does not have a negative impact on the quality of MRI.
Why is it important not to move during the test?
Any movement during the examination reduces the quality of the resulting images. Multiple motion artifacts may appear on the images, and the MRI results will be uninformative.
Can I do the research with an accompanying person?
Absolutely yes. You can invite any accompanying person from among your family and friends to the MRI room. It is important that your companion does not have metal implants or artificial pacemakers in his body.
Preparation
Simple preparation for MRI of the lower back is an important stage of a successful study, which is best not to be ignored. The first step to quality tomography is to sign up for an examination. If you're not entirely sure which MRI to choose, ask for a free consultation with a neurologist who can advise you on what type of MRI you should do and with what scanning protocol. In the clinic, you need to inform the doctor about the presence of any metal structures in the body and pacemakers. If the patient is afraid of the procedure, he can take sedatives an hour before the diagnosis, which are indicated for claustrophobia. When pain in the back prevents you from lying in a horizontal position for a long time, it is better to take painkillers or do a blockade before the tomography. Before scanning, it is necessary to remove all metal objects from the body, phone, magnetic cards, so that they cannot affect the results of the study.
Preparation for the procedure and its implementation
If an MRI of the lumbar spine with a contrast agent is prescribed, it is administered before immersion in the machine. Normally, no preparation is needed, but if the patient is allergic, it is necessary to test the substance itself for tolerance. Most clinics do not do this, relying on the hypoallergenic nature of the components. However, an allergy sufferer should not take the risk.
When a person is fixed on the table, its upper, movable part slowly moves into the chamber itself. The ring part lowers its sensor to the level of the lumbar region and the device turns on. The patient sees the process as actively moving red lights. At this point, you can simply close your eyes if the process makes you nervous. The study does not last long: up to 10 minutes. Then the moving part moves out, the clamps loosen and you can stand up.
The result takes time to process, so it is impossible to get it right away. Only inpatients receive the fastest MRI results: within a few hours on the same day. For other people, receipt is possible only the next day: at the reception or from your specialist who gave the referral.
Interpretation of MRI results of the lumbosacral region
An example of MRI decoding of the lumbosacral region
On a series of MRIs of the lumbar spine, physiological lordosis is straightened.
Retrolisthesis of the L5 vertebra by ~ 4 mm. A decrease in the signal intensity on T2-WI of the discs is determined (minimal in the Th12-L5 segments, pronounced in the L5-S1 segment), a decrease in the height of the Th12-S1 discs, moderate arthrosis of the intervertebral joints, hypertrophy of the yellow ligaments, the formation of anterolateral marginal bone growths of the L5, S1 vertebrae . There is compaction of the endplates of the vertebral bodies with areas of unexpressed subchondral sclerosis. Linear areas of bone marrow edema in the L5, S1 vertebral bodies. The posterior longitudinal ligament is compacted. Dorsal median disc herniation L5/S1 up to 4.5 mm, migrating caudally, deforming the dural sac, in contact with the roots, moderately narrowing both intervertebral foramina. The sagittal size of the spinal canal is 13 mm. The structure of the contents of the dural sac is not changed. The distal parts of the spinal cord and the cauda equina are not displaced or deformed; areas of pathologically altered signal in the brain substance are not detected. Liquorodynamics are not disturbed. Paravertebral soft tissues are not changed. Bone destructive changes in the sacrum and coccyx are not detected. Bone marrow edema of the S5 vertebra is determined, with the presence of a local area of hypointense signal on T1-BI in the distal parts of the vertebra (a fracture cannot be reliably excluded). Areas of fatty bone marrow degeneration in the Co1-Co4 vertebral bodies. There are no signs of inward deviations (dislocations, subluxations) of the coccygeal vertebrae; deviation of the coccygeal vertebrae from the center line to the right is noted. Conclusion: MRI signs of degenerative-dystrophic changes in the lumbar spine. L5/S1 disc herniation. Narrowing of the spinal canal of secondary origin. The MRI picture does not reliably exclude a fracture of the S5 vertebra. It is difficult for an ordinary person to independently understand and interpret the results that, after an MRI, will be given to him on a digital medium. Therefore, with the conclusion of the radiologist and the photographs, he should go for a consultation with the attending physician, who will make a final diagnosis based on the summary data of the examination, medical history and tomography data. In our clinic , after an MRI, you can have a free consultation with a neurologist or orthopedist . Doctor
- will answer all questions based on the results of the research and the conclusion received
- Helps explain tomography results without using complex radiological terminology
- will conduct an examination and, if necessary, offer treatment.
“Second independent opinion” service Medicine is an area where we want to be 100% sure . Therefore, at your request, we will be happy to offer you the service of a second independent opinion from the leading consultant of our clinic, Candidate of Medical Sciences , a doctor of the highest category with 18 years of experience in the field of tomography and radiology N.V. Marchenko.
Which device is better to choose?
The type of tomograph used for diagnostics directly affects the comfort and cost of the examination. Today, you can undergo MRI of the lumbosacral spine in clinics in St. Petersburg using closed or open type equipment. The first option is a device in the form of a pipe. Due to its closed design, it is not always suitable for people with fear of confined spaces, overweight patients, or children.
Unlike a closed device, an open MRI of the lumbosacral region can be performed on any patient. This is the most comfortable form of diagnosis for the patient. However, open-type tomographs are low-field installations. In terms of information content, they are inferior to closed-type machines in identifying tumors and demyelinating diseases. Hernias and protrusions, signs of osteochondrosis and spondylosis will be clearly visible on them. The main advantage of tomography using an open device will be comfort and affordability. MRI in closed installations can guarantee high image resolution and higher diagnostic accuracy.
| OPEN TYPE MRI | SEMI-OPEN MRI | CLOSED MRI |
Author: Kasimov Evgeniy Tulkunovich
Neurologist with 8 years of experience
X-ray, CT or MRI - what to choose
It is impossible to answer the question posed unambiguously, since each of the given methods is strong in its own field. The decision to prescribe a specific study is made by the doctor, who analyzes a number of factors, including the location of the suspected pathology, the patient’s condition, the degree of progression of the disease, and characteristics of the symptoms. To conduct a comparative analysis of the procedures, we provide a table of key selection criteria. First let's compare MRI and X-ray:
| MRI | X-ray |
| Special medical centers are equipped with the device | All healthcare institutions are equipped with the device |
| No radiation exposure | Based on X-ray radiation |
| Duration - 15-30 minutes | Duration: a few seconds |
| Expensive procedure | Low cost |
| Can be performed on pregnant women (2nd, 3rd trimester) | The study is contraindicated for pregnant women |
| The examination is applicable in the diagnosis of soft tissues, ligaments, discs between vertebrae, etc. | The procedure is informative in diagnosing bone tissue |
CT is comparable in information content to magnetic tomography, however, it is based on X-ray radiation. This option is cheaper (compared to MRI), but is not suitable for examining pregnant women and young children.

The most harmful diagnostic method
What determines the price of an MRI of the lumbosacral region?
| Service | Price according to Price | Discount Price at Night | Discount Price During the Day |
| from 23.00 to 8.00 | from 8.00 to 23.00 | ||
| MRI of the lumbosacral spine | 3300 rub. | 2690 rub. | 2990 rub. |
| MRI of the sacroiliac joints | 4000 rub. | 3190 rub. | 3690 rub. |
| MRI of three parts of the spine | 9900 rub. | 6900 rub. | 7900 rub. |
| Appointment with a neurologist | 1800 rub. | free after MRI | free after MRI |
| Comprehensive body diagnostics (MRI of the thoracic spine, MRI of the lumbar spine, ultrasound of the abdominal organs, ultrasound of the kidneys, ultrasound of the bladder, consultation with a neurologist, consultation with a therapist) | 11700 rub. | — | 7000 rub. |
Degenerative changes in the lumbar spine are diagnosed using any model of tomograph. Both low-field and high-field MRI machines cope with this task. The cost of MRI of the spine is influenced by several aspects:
- tomograph power;
- availability of discounts and promotions;
- qualifications of medical staff;
- geographical location of the clinic.
Also, the final price of tomography is influenced by the MRI study protocol - with or without contrast. MRI of the lumbar region with contrast will cost more, since the cost of the coloring agent will be added to the price of the tomography itself, which is calculated individually based on the patient’s body weight.
What determines the cost of tomography?
![]()
Tomograph power
![]()
Applying Contrast
Personnel qualifications
![]()
Promotions and discounts