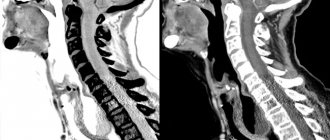
Computed tomography with contrast
CT with contrast involves examining the patient's body using minimal doses of X-ray radiation. This type of diagnostic method also involves introducing a contrast agent into the human body before the procedure. This is necessary in order to significantly increase the contrast between healthy and diseased tissues, identify even the slightest signs of the disease and make a diagnosis in the early stages.
Why do you need a CT scan with contrast?
CT scan using contrast can identify healthy and pathological tissues of the body, therefore it is often prescribed for suspected cancer. This is explained by the fact that pathological tissues are supplied with blood much better than healthy ones, so the iodine contained in the contrast accumulates in them, making it possible to find out the size, location and confirm the presence of a tumor.
The blood vessels through which the contrast agent moves are often also examined and any abnormalities identified. It also often happens that contrast-enhanced computed tomography is prescribed to examine the abdominal organs, since this can significantly improve the clarity of the resulting image. All areas that accumulate contrast are highlighted in white in the images, which makes it possible to detect even small tumors.
What is the difference between MSCT and CT
Examination using MSCT is more expensive than CT, so patients rightly ask the question: is it possible to replace the procedure with a more affordable CT? Let's look at the difference between CT and MSCT.
In simple words, MSCT is a more advanced CT model. Computed tomography (CT) is inferior to multi-slice diagnostics in terms of image quality, takes longer and has a high radiation dose to the body.
Multislice computed tomography (MSCT) takes less time due to the fact that the table on which the patient is located moves inside the device at a given speed, and information is collected not only by static sensors, but also by a special tube that moves in a spiral and transmits signals to the sensors. The higher the table rotation speed, the larger the area that can be examined and the resulting radiation exposure is 40% less than with CT. Because the procedure is 2 times faster.
Even the design of the device differs between both types of tomography. Equipment for MSCT has more technical capabilities: the doctor can select the settings individually for each patient.
In 80% of cases when a patient applies for MSCT as prescribed by a doctor, there is a need to confirm the fact:
- aortic diseases;
- hemorrhages;
- tumor and its location;
- liver diseases.
For other indications, there is no particular difference in the choice of diagnostic method, since both methods provide accurate information equally quickly.
What contrasts are used for CT
As a rule, various iodine-containing preparations are used to increase the contrast of the resulting image. All of them are divided into two groups - fat-soluble and water-soluble. Medicines of the first group are very viscous, so their use is limited. They are administered only locally, for example, into the peritoneal cavity to identify fistulas, etc. If we are talking about computed tomography with bolus contrast (the drug is administered into a vein with a special injector) or about the drug being administered orally, water-soluble contrast is used. The toxicity of such drugs is several times lower, and they also quickly enter the blood vessels.
How is contrast agent administered?
Contrast-enhanced computed tomography involves several ways to administer a contrast agent. The method chosen will depend on what exactly needs to be inspected. Contrast can be injected orally, into a vein, rectally, into an organ, or even into the lesion itself. It is worth taking a closer look at the most common methods.
Oral route
This method is most often used when examining the gastrointestinal tract; in this case, the patient must drink the drug according to the recommendations specified in the instructions. The medications are quickly absorbed, significantly increasing the clarity of the image of the mucous membranes of the stomach and allowing you to see polyps or narrowings. Often combined with intravenous contrast.
Intravenous administration
CT using intravenous contrast involves several types of injection of a substance into the body. Namely:
- Before the procedure, a nurse will inject the drug into the patient’s vein;
- first, a regular CT scan is performed, then the computer tomograph is stopped, contrast is injected into the patient’s vein, and the procedure continues with a contrast agent;
- the substance is administered as a bolus using a special syringe or a dropper if you need to administer the drug slowly.
Computed tomography with intravenous contrast is most often performed.
Into the lumen of the cavity
In such a situation, fat-soluble substances are used to determine the presence of diverticula, fistulas and other abnormal formations. Sometimes when examining hollow organs (for example, the bladder, colon), contrast is injected into them before the procedure begins. The harm of CT with contrast will be slightly higher, since fat-soluble compounds are more toxic than water-soluble ones. But, nevertheless, problems with removing the substance from the body do not arise if all the doctor’s recommendations are followed.
Other Applications
When examining the main arteries of the neck and extremities, it is very important to evaluate all sections to identify atherosclerotic plaques, the presence of narrowing of the lumen of the vessel, and to identify changes in the course of blood vessels. In some patients, detection of such changes is difficult in some areas due to anatomical features.
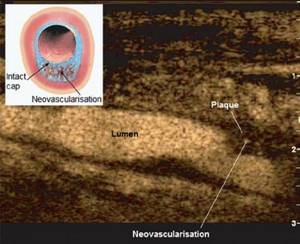
The use of ultrasound contrasts significantly improves the quality of visualization of the above pathological changes. Recent European and American studies have shown that ultrasound contrasts make it possible to clearly see newly formed vessels inside an atherosclerotic plaque and ulceration of the surface, which is a sign of the risk of detachment of part of the plaque and the development of serious embolic complications.
Theoretically, a contrast agent can be injected into any body cavity that is accessible by an ultrasound probe. The most successful application in this category is contrast-enhanced hysterosalpingosonography (HyCoSy, injection of contrast into the uterine cavity) to evaluate the patency of the fallopian tubes (search for causes of infertility).
German scientists reported the results of a study that involved patients with fertility disorders who underwent transvaginal ultrasound and hysterosalpingosonography with ultrasound contrast. The results of hysterosalpingosonography were compared with those of more invasive established techniques such as chromolaparoscopy and found a concordance of 91%.
Hysterosalpingosonography is rapidly becoming the preferred screening method for tubal patency.
Vesicoureteral reflux (backflow of urine from the bladder) is a common problem in children. Ultrasound examination of reflux as an alternative to x-ray cystography can detect or exclude vesicoureteral reflux. European experts compared different types of radiation diagnostics to identify this pathology. Their study showed that contrast-enhanced ultrasound is the lowest-cost and safest method for detecting vesicoureteral reflux in children.
Ultrasound imaging of the upper abdomen is often difficult due to the presence of gases in the intestine and the obesity of the patient. Poor visualization of the body and tail of the pancreas usually prevents adequate abdominal ultrasound.
Often, to get answers to remaining questions and increase confidence in the absence of tumors, patients are additionally referred to a CT or MRI. Ultrasound examinations that do not provide a definitive diagnosis often entail additional diagnostic tests that are expensive, time-consuming, inconvenient, and associated with some risks.
How is tomography with contrast performed?

If you do not know how to prepare for a CT scan with contrast, it is worth checking with your doctor before the procedure, as recommendations depend on what exactly needs to be examined. The procedure itself is quite standard: after the contrast is administered, the patient is placed on the tomograph table, then the diagnosis begins.
CT perfusion
This procedure is non-invasive. This type of tomography is performed only using contrast and involves examining the blood vessels of the selected organ - liver, brain
, kidneys, etc. The advantage of the procedure is that it will be possible to examine all the structures of the organ at the capillary level.
Angiography
To find out what the contrast-enhanced CT procedure shows, you need to first become familiar with its main difference from other types of tomography. This research method involves surgical intervention in the body. Such diagnostics allows you to assess the condition of the blood vessels and determine how normal their lumens are. Through a puncture, which is usually made by the arteries of the groin area, a special catheter is inserted, allowing one to gradually reach the organ being examined and obtain all the necessary information.
Bibliography
- ACR Manual on Contrast Media, ACR Manual on Contrast Media – Version 10.1, 2015.
- Hiremath S, Akbari A, Shabana W, et al. Prevention of contrast-induced acute kidney injury: is simple oral hydration similar to intravenous? A systematic review of the evidence. PLoS ONE 2013; 8: e60009.
- Kim SM, Cha RH, Lee JP, et al. Incidence and outcomes of contrast-induced nephropathy after computed tomography in patients with CKD: a quality improvement report. Am J Kidney Dis 2010; 55:1018-25.
- Mehran R, Aymong ED, A Simple Risk Score for Prediction of Contrast-Induced Nephropathy After Percutaneous Coronary Intervention. Development and Initial Validation. Journal of the American College of Cardiology Vol. 44, No. 7, 2004
- Morcos SK, Thomsen HS, Webb JAW, et al. Contrast-media-induced nephrotoxicity: a consensus report. Eur Radiol 1999; 9:1602–13.
- Solomon RJ, Natarajan MK, Doucet S, et al. Cardiac Angiography in Renally Impaired Patients (CARE) study: a randomized double-blind trial of contrast-induced nephropathy in patients with chronic kidney disease. Circulation 2007; 115:3189-96.
- Stacul F, van der Molen AJ, Reimer P, et al. Contrast-induced nephropathy: updated ESUR contrast media safety committee guidelines. Eur Radiol 2011; 21: 2527-41.
- Taylor AJ, Hotchkiss D, Morse RW, McCabe J. PREPARED: Preparation for Angiography in Renal Dysfunction: a randomized trial of inpatient vs outpatient hydration protocols for cardiac catheterization in mild-to-moderate renal dysfunction. Chest 1998; 114:1570-74.
- Weisbord SD, Palevsky PM. Prevention of contrast-induced nephropathy with volume expansion. Clin J Am Soc Nephrol 2008; 3:273-80.
- Weisbord SD, Mor MK, Resnick AL, et al. Incidence and outcomes of contrast-induced AKI following computed tomography. Clin J Am Soc Nephrol 2008; 3:1274-81.
- Clinical guidelines for the prevention, diagnosis and treatment of contrast-induced nephropathy. Developer: Scientific Society of Nephrologists of Russia Association of Nephrologists of Russia. Working group: Prof. Volgina G.V. prof. Kozlovskaya N.L., Ph.D. Shchekochikhin D.Yu.
- Contrast-induced nephropathy on the Cardioplaneta website. (as amended on February 7, 2021)
- Dunaeva A.R. , Shcherbakova A.S., Khafizov T.N., Zagidullin N.Sh., Contrast-induced nephropathy during coronary angiography. Modern issues of diagnostics, '3 (79) July 2014, p. 35-40
Who is contraindicated for contrast agents?
There are many contraindications to CT with contrast. Contrast cannot be used if:
- allergies to iodine or seafood;
- pregnancy at any stage, even small;
- diabetes mellitus;
- renal or heart failure;
- thyroid diseases;
- myeloma disease.
Breastfeeding mothers will have to wean their baby off the breast for two days after the procedure, as some contrast may pass into the milk. It is also worth knowing that the CT procedure as such becomes impossible in the case of a large patient’s weight - the devices are not designed for a weight of more than 150-200 kg. The tomography procedure is not prescribed unless absolutely necessary for patients under 14 years of age, as well as for patients with an unstable mental state or suffering from claustrophobia. In some cases, light medicated sleep can be used.
C. Assessment of renal function in patients with CKD and/or risk factors for CIN
Estimated glomerular filtration rate (eGFR) is estimated from the serum creatinine level of the most recent test performed within 6 weeks. In patients with established CKD or other risk factors for CIN, as described above, if the most recent creatinine test is 6 weeks or more old, repeat testing is indicated. In other cases, an accelerated analysis is indicated.
An online version of the eGFR calculator that uses this formula can be accessed via a link on the National Kidney Foundation website.
Calculation of the risk of developing CIN according to Mehran R., 2004
| Risk factors for CIN | Definition | Scale, points |
| Decreased renal perfusion | Hypotension (SBP < 80 mmHg during one hour of inotropic support) | 5 |
| Intra-aortic balloon counterpulsation | 5 | |
| Chronic heart failure III-IV NYHA | 5 | |
| Age | >75 years old | 4 |
| Hematocrit | <39% for men and <36% for women | 3 |
| Diabetes | 2 | |
| Volume of contrast agent | 1 for every 100ml | |
| Initially impaired renal function | Serum creatinine > 132.6 µmol/L or eGFR <60 ml/min/1.73 m2 | 2 points for 40-60 |
| 4 points for 20-40 | ||
| 6 points for <20 | ||
| Risk assessment | ||
| Frequency of development of CIN | Need for dialysis | |
| Low risk (≤5 points) | 7,50% | 0,04% |
| Medium risk (6-10 points) | 14,00% | 0,12% |
| High risk (11-15 points) | 26,10% | 1,09% |
| Very high risk (≥16 points) | 57,30% | 12,60% |
Online version of the risk calculator >>>