Positron emission tomography (PET) has recently become an increasingly popular research method used to detect, stage and monitor various malignant tumors. The method is based on recording gamma radiation emitted by radioactive elements (radionuclides), which are introduced into the human body as part of special labeled substances - radiopharmaceuticals (RP). When a PET scanner is combined with a computed tomography (CT) scanner, it is called combined positron emission tomography and computed tomography (PET-CT).
The combination of PET and CT allows you to combine “functional” (PET) and “anatomical” (CT) tomograms, which provides advantages over using only CT, because anatomical sections are supplemented with information reflecting functional changes. Thus, when comparing changes detected by PET-CT (58 patients took part in the study) with data obtained only on the basis of CT, combined PET-CT showed better results in identifying small tumors and multiple metastases; as well as in detecting tumor-affected lymph nodes and assessing response to chemotherapy for breast cancer.
What is the difference between CT and PET-CT for breast cancer?
Methods such as CT and MRI are based on visualization of anatomical structures in order to identify pathological changes in patients with breast cancer, staging and control. At the same time, positron emission tomography (PET) makes it possible to detect pathological changes in the metabolism of 18-fluoro-2-deoxy-D-glucose (FDG), which makes it possible to obtain high-quality information about its accumulation in the tumor, and is a critical point in the diagnosis diagnosis and during control studies. The combination of PET-CT has advantages over the isolated use of PET, since it becomes possible to more accurately assign foci of increased FDG uptake to specific anatomical areas. In addition, this method reduces the research time. Also, PET-CT can partially overcome the limited specificity of PET, which can detect foci of glucose hypermetabolism in benign tumors and inflammatory tissues (for example, in tuberculosis). A necessary condition for the informativeness of the method is a reliable assessment of the images by an experienced radiologist, sometimes with the use of a Second Opinion.
How is a CT scan of the mammary glands performed?
CT scans of the mammary glands are most often performed with contrast. This is an iodine-based substance that is safe for the human body and is injected through a catheter into the blood. This approach allows you to obtain a more accurate image. Before undergoing a CT scan, the patient will be asked to remove any metal objects, including piercing jewelry. If there are implants, shunts, pacemakers or other foreign objects in the body, you should inform your diagnostician.
The procedure is carried out after the patient has taken a lying position on the tomograph table, which smoothly moves into the scanner. The start of scanning is signaled by clicks and noise that appear during scanning. It is important that the patient lies still and relaxed. The procedure lasts 15 minutes or longer and is absolutely painless and cannot cause any discomfort.
Early diagnosis of breast cancer
Breast cancer is the most common neoplasm in women worldwide and the leading cause of cancer-related mortality in women. Worldwide, there are approximately 1.38 million new cases of the disease each year, as well as 458,000 annual deaths due to the disease. Many risk factors are well known. However, the exact causes of breast cancer have not been determined. For example, having the disease in relatives and ancestors is a well-known risk factor: it increases the likelihood of developing cancer by two or three times. It is also assumed that mutations in the BRCA gene (1 and 2) and mutations in the p53 protein significantly increase the risk of tumor development. Early diagnosis is a fundamental method of control, as it determines the method of treatment, as well as the patient’s prognosis and chances of survival.
What happens after a CT scan of the chest?
If contrast dye was used during the procedure, the patient may be monitored for a period of time for any side effects or reactions to the contrast dye. These include itching, swelling, rash, or breathing problems.
You should tell your doctor if you notice pain, redness, or swelling in the IV site after returning home. These could be signs of infection or another type of reaction.
If contrast is administered to a patient by mouth, the patient may experience diarrhea or constipation after the procedure.
Generally, no special care will be required after a chest CT scan. The patient can return to his normal diet and activities.
How to detect breast cancer
Diagnostic methods based on the detection of anatomical changes include mammography, ultrasound (US), computed tomography (CT), and magnetic resonance imaging (MRI). They are widely used in clinical practice to identify the primary tumor and determine the stage of breast cancer. These diagnostic methods are constantly improving, in addition, new methods of studying the mammary glands are also being introduced into practice: optical mammography, single photon emission tomography (SPECT) and positron emission tomography (PET), which allow transferring information regarding anatomical changes, function, metabolism from the macroscopic to the molecular level.
Radionuclide research methods, including SPECT and PET, make it possible to assess in vivo the cellular, molecular and biochemical features of neoplasms and normal tissues. While "anatomical" diagnostic methods emphasize increasing spatial resolution and image quality, the goal of using radionuclide methods is more specific - increasing the contrast between the tumor and normal tissues.
In combination with traditional radiation diagnostic methods, radionuclide research methods, which allow visualization of biological processes, have made it possible to take a step forward in cancer detection. And now the new goals of using radionuclide methods are to separate various biochemical changes in tissues.
Indications for CT scanning of the mammary glands
As already mentioned, computed tomography is prescribed to clarify the results of previous studies if it is not possible to determine the nature of the tumor and provide the following information:
- Precise localization of the tumor;
- Presence/absence of metastases;
- Tumor operability;
- Confirmation of a malignant breast neoplasm if it cannot be palpated;
- The condition of the lymph nodes that are located nearby.
CT is also used in cases where it is necessary to collect material for diagnostics, but ultrasound and mammography do not allow full control of the process.
Evaluation of the Primary Tumor
The ability to detect breast cancer using PET depends on the size and tissue structure of the tumor. The sensitivity of PET is reported to be 68% for small tumors (less than 2 cm), and 92% for larger tumors (2-5 cm), however, the overall accuracy for detecting cancer in situ is low (sensitivity is 2-25%) . Thus, the main factor limiting the use of PET in breast imaging is the low detection rate of small tumors and noninvasive cancers.
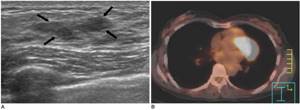
Ductal carcinoma in situ in a 49-year-old woman. A: Ultrasound reveals a hypoechoic mass formation measuring 2.5 cm with indistinct edges, located in the upper parts of the left breast (marked by arrows). B: PET-CT scan shows no evidence of increased FDG uptake in the left breast. Surgery confirmed non-invasive ductal carcinoma.
However, the method plays an important role for some groups of patients, for example, with dense mammary glands or with the presence of implants. Positron emission tomography is used to determine the multiplicity of tumor lesions; to identify the location of the primary tumor in patients with metastases, when mammography is uninformative; as well as in those patients for whom biopsy is contraindicated. PET-CT has potential advantages over isolated PET in the evaluation of small lesions that may show reduced FDG uptake due to the partial volume effect of PET, since glucose hypermetabolism can be characteristic of both pathological and normal anatomical structures.
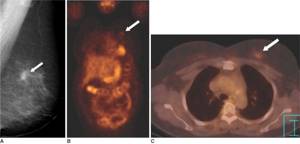
Invasive breast cancer in a 57-year-old woman. A: a screening radiograph of the left breast in an oblique mediolateral projection reveals a space-occupying formation with spicule-shaped edges, about 1.1 cm in size (marked by an arrow). B: PET scan revealed a focus of mild FDG hypermetabolism (standardized uptake level = 1.2) in the left breast. The lesion is difficult to detect due to the partial volume effect. C: PET-CT identifies a focus of FDG hypermetabolism in a limited area (marked by an arrow) in the left mammary gland.
Where to get an MRI with contrast in Moscow?
Any lump in the chest requires high-quality diagnosis. Doctors at the Central Clinical Hospital of the Russian Academy of Sciences recommend regular examinations to their patients, especially since MRI of the mammary glands can be done as many times as necessary. Safe and painless procedures in our clinic are carried out using the latest high-resolution equipment. This allows you to obtain detailed images of excellent quality and make accurate diagnoses. The cost of the study is one of the most affordable in Moscow.
To make an appointment for an examination and clarify the cost of services, you can call or use a special form on the website.
Assessment of secondary lymph node involvement
The second objective of the method is to detect breast cancer metastases in the lymph nodes. Metastatic lesions of the axillary lymph nodes are an important factor determining the prognosis. Patients suffering from breast cancer with secondary damage to four or more axillary lymph nodes have a significantly higher risk of relapse. Sensitivity of PET for imaging axillary lymph nodes in patients with breast cancer has been reported to range from 79% to 94% and specificity to 86% to 92%. With PET-CT, it is possible to accurately determine the location and distinguish from each other lymph nodes secondarily affected by the tumor and reactively changed (non-cancerous) lymph nodes, while CT will reveal only multiple enlarged lymph nodes of the axillary group without clear differential signs.
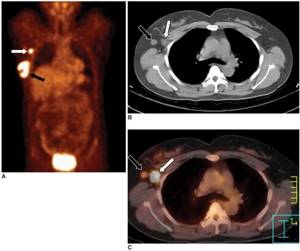
Axillary lymph node metastases in a 45-year-old woman with invasive ductal breast cancer. A: PET shows a focus of FDG hypermetabolism in the right gland (black arrow) and in the axillary region (white arrow). B: CT scan reveals two enlarged axillary lymph nodes on the right (marked by arrows). C: PET-CT allows you to determine the exact localization of lymph nodes secondarily affected by the tumor (white arrow, standardized level of radiopharmaceutical accumulation = 9.9); a reactively changed lymph node is also visualized (black arrow). Among 21 lymph nodes removed during surgery, metastases were detected in only one.
Metastases of breast cancer to intrathoracic or mediastinal lymph nodes often do not manifest themselves clinically. The number of detected pathological changes in intrathoracic or mediastinal nodes (in patients with metastatic or recurrent breast cancer) with PET is almost twice as large as compared with traditional CT. In addition, PET-CT appears to be more useful than CT for the evaluation of hilar and mediastinal lymph nodes, since the ability of CT to detect metastases in small lymph nodes is quite limited.
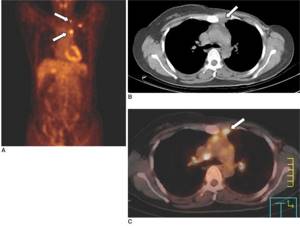
Metastases to the mediastinal lymph nodes in a woman who underwent a modified radical left mastectomy 10 months ago. A: PET scan reveals multiple areas of radiopharmaceutical hypermetabolism in the left upper chest. B: CT image shows a small area of soft tissue density in the anterior mediastinum (marked with an arrow). B: PET-CT revealed that the soft tissue area in the anterior mediastinum identified on CT correlates with an area of FDG hypermetabolism, suggesting metastases to the hilar lymph nodes.
What do abnormal results mean?
A chest CT scan can diagnose problems with the heart, lungs, or chest area, including:
- A tear in the chest, an abnormal widening or swelling, or narrowing of the main artery that carries blood out of the heart (aorta)
- Other abnormal changes in major blood vessels in the lungs or chest
- Accumulation of blood or fluid around the heart
- Lung cancer or metastatic cancer that has spread to the lungs from other parts of the body
- Fluid accumulation around the lungs (pleural effusion)
- Damage and enlargement of the large airways of the lungs (bronchiectasis)
- Enlarged lymph nodes
- Lung diseases in which lung tissue becomes inflamed and then damaged.
- Pneumonia
- Esophageal carcinoma
- Lymphoma in the chest
- Tumors, nodules, or cysts in the breast
Evaluation of distant metastases
Breast cancer often gives distant metastases to the lungs, liver and bones. The advantage of whole body PET over traditional diagnostic methods, such as chest radiography, skeletal scintigraphy and abdominal ultrasound, is the ability to detect distant metastases in various areas of the body and organs during one study. Whole body PET has been found by Moon et al to have high diagnostic accuracy in patients suspected of having recurrent or metastatic cancer. Based on the number of lesions detected, the sensitivity of the method in detecting distant metastases was 85% and the specificity was 79%.
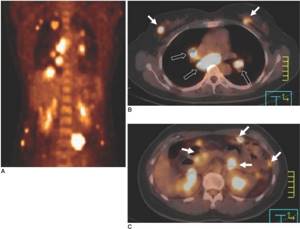
Multiple distant metastases in a 44-year-old female patient suffering from cancer of both glands. A: PET scan shows multiple areas of FDG hypermetabolism in the chest and abdomen. B, C: PET also revealed areas of FDG hypermetabolism in both mammary glands (marked with white arrows on tomogram B), in the mediastinal lymph nodes (marked with black arrows on tomograph B), and in the internal organs (marked with arrows on tomograph C).
In a study (Cook et al.), PET was found to be superior to skeletal scintigraphy in detecting osteolytic metastases from breast cancer. Conversely, osteoblastic metastases are characterized by low metabolic activity and are often undetectable by PET. However, PET-CT overcomes this limitation: osteoblastic metastases, even if not visible on PET, will be visualized on CT scans.
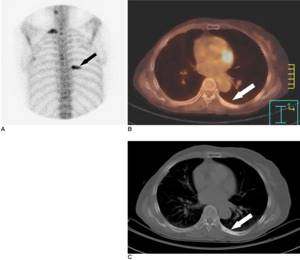
Bone metastases in a 64-year-old woman who underwent right modified radical mastectomy 36 months ago. A: Skeletal scintigraphy reveals foci of FDG hyperfixation in the first rib on the right and the seventh rib on the left (arrows), which are most likely associated with metastatic disease of the ribs. B: PET-CT shows no FDG hypermetabolism in the left seventh rib (arrow). C: CT scan reveals an osteoblastic lesion on the left seventh rib (arrow).
Contraindications and side effects
The examination is not carried out if:
- severe forms of bronchial asthma, renal and liver failure;
- allergic reaction to contrast agent (if used);
- acute mental disorders.
Restrictions associated with breastfeeding. If examination is necessary, the woman is recommended to express milk first so that there is enough for several feedings. If the child needs diagnosis, it can be performed. The specifics of the examination in this case are agreed with the doctor.
Important! The doctor will tell you about all contraindications. If necessary, he will agree with the patient on all the specifics of the examination. In some cases, you may need to stop taking certain medications.
Breast cancer treatment
To treat patients whose tumor is large or has local spread, neoadjuvant chemotherapy is used to reduce the stage of the primary tumor before surgery and eliminate metastases. In addition, several studies have demonstrated that survival of patients with refractory tumors may be improved by using alternative chemotherapy and/or by lengthening chemotherapy courses. Since chemotherapy has side effects, it is necessary to identify patients who do not benefit from the treatment as quickly as possible.
Currently, radiodiagnostic methods are often used to determine the response to therapy by assessing changes in tumor size. However, serial measurements of tumor size in many cases do not allow inferring the presence of an early response. The effectiveness of PET in assessing response to therapy has been confirmed for various types of neoplasms. A study by Smith et al showed that the mean reduction in FDG uptake after the first course of chemotherapy was greater in lesions that showed a macroscopic partial or complete response, or a microscopic complete response, compared with resistant lesions. in histopathological studies. According to (Rose et al.), after a single course of chemotherapy, positron emission tomography was able to predict complete response to therapy on pathological examination, with a sensitivity of 90% and a specificity of 74%. If we take the degree of decrease in FDG uptake less than 55% of the initial value as the threshold value indicating the presence of a response to treatment, changes in PET in all respondents in this study were correct and confirmed pathologically (100% sensitivity and 85% specificity).
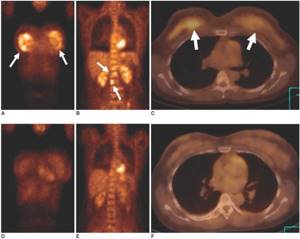
Images illustrate chemotherapy management in a 35-year-old female patient with breast cancer with bone metastases. AC: Initial PET (A, B) and PET-CT (C) show significant FDG hypermetabolism in both breasts and in many vertebrae. DF: control PET (D, E) and PET-CT (F) performed after three courses of chemotherapy show a significant decrease in FDG hypermetabolism in both mammary glands and vertebrae.
PET-CT also plays a role in radiotherapy because it allows accurate assessment of tumor extent.
How is a chest scan done?
If contrast is used during the examination, the procedure is performed on an empty stomach. A regular CT scan requires no preparation. The patient is placed on a special table (metal items must be removed before this) and moved inside the tomograph. The examination lasts from 10–15 minutes (without contrast) to half an hour (with contrast). Do not move while the scanner is running. This is one of the main conditions on which the quality of the images depends. The doctor observes the procedure from an adjacent room, and if necessary, you can contact him via speakerphone.
After the scanning is completed, the resulting images are decrypted and given to the patient along with a medical report.
Tumor recurrence control
Early recognition of tumor recurrence is important in improving survival by prompting clinicians to use different treatment modalities. However, it is difficult to distinguish a true relapse from postoperative and radiation changes when using only traditional methods of radiation diagnosis. With limited, regional relapse, the mammary gland, skin, axillary and supraclavicular lymph nodes, and the chest wall are predominantly affected.
The sensitivity and specificity of PET in detecting recurrence were found to be 84% and 78%, respectively, while the sensitivity and specificity of conventional testing were 63% and 61%, respectively. PET has been suggested to be a more effective method for assessing breast cancer recurrence than traditional imaging techniques in detecting changes throughout the body. CT data obtained from PET-CT allow us to establish the correspondence of anatomical structures and foci of FDG hypermetabolism.
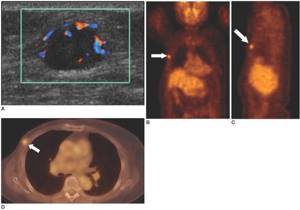
Local tumor recurrence in a 74-year-old woman who underwent a modified right radical mastectomy 8 years ago. A: Ultrasound revealed an ovoid-shaped mass, 1.4 cm, with increased blood flow, located in the right pectoral muscle in the mastectomy area. B, C: PET scan reveals a localized focus of FDG hypermetabolism (standardized uptake rate = 3.3) (arrows) in the right hemithorax. D: PET-CT identifies a focus of FDG hypermetabolism (arrow) in the right pectoral muscle, while using PET alone is difficult to determine the exact location of the focus.
CT scan of the mammary glands at CELT - effective and convenient!
Our clinic has a powerful diagnostic base, which is represented by modern equipment. Multislice 64-slice tomograph "General Electric" allows you to conduct research in accordance with international safety and quality standards. The specialists of our radiology department have many years of clinical experience and actively collaborate with doctors of various specialties, which allows us to further increase the efficiency of diagnostics. You can make an appointment with doctors at our clinic online or by phone: +7.
Deciphering PET-CT for breast cancer
In some cases, to increase the reliability of the assessment of PET-CT results, it is recommended to obtain a second opinion from a specialized radiologist. This may be necessary if the results of the initial reading of the images are dubious or ambiguous. A second opinion on PET-CT helps solve the following problems: reducing the risk of medical error, more reliable assessment of the primary tumor, clarifying the stage of the disease, reliably excluding signs of metastatic lesions of the bones, liver or lungs. In addition, as a result of such a consultation, the oncologist receives a more detailed description of the study, which helps him choose the most appropriate treatment protocol.
Contraindications to CT:
- due to the fact that the mammary glands are highly sensitive to radiation exposure and a fairly large dose load (minimum 2.8 mSv with MSCT versus 0.5 mSv with mammography), CT is not recommended for women with high radiation sensitivity, mutation of cancer genes, or a family history;
- It is not recommended to perform CT scans frequently (more than once a year), or if other radiation methods have recently been used;
- Scanning is strictly prohibited for pregnant and lactating women.
Due to the high sensitivity of the organ to ionizing radiation, it is advisable to scan only with a multislice tomograph (with a step-by-step tomograph, the radiation dose can reach 13 mSv).
For all contraindications, it is recommended to use an equally informative method - magnetic resonance imaging.