Currently, up to 15% of surgical interventions in patients admitted with symptoms of an acute abdomen are performed for small bowel obstruction. In Europe, up to 60% of cases occur due to adhesions, 20% due to various hernias, and about 15% of obstructions are associated with neoplastic processes. In the USA, 50-75% of cases are associated with adhesions, in second place are Crohn's disease and inflammatory enteritis, and in last place is oncology.
Modern diagnostic approaches include abdominal ultrasound or standing radiography as the first line of imaging. Recently, there has been an increased tendency to use the ultrasound method, which, according to some authors, can replace classical radiography. Ultrasound allows you to correctly determine the presence of small intestinal obstruction, and often reveals a lot of different additional diagnostic information that is of decisive importance for treatment tactics. The main method of final, verified diagnosis of small intestinal obstruction at the moment is SCT/MDCT with bolus contrast enhancement, being the gold standard of imaging.
According to the mechanism of occurrence, acute small intestinal obstruction is divided into:
- lumen obstruction
- narrowing of the lumen
- external compression
- intussusception
- passage blockade
- colon obstruction
- strangulation/volvulus
- complex mechanism.
The etiology and mechanisms of small intestinal obstruction are well described in many manuals and monographs, so I will not duplicate this widely available information.
Small bowel intussusception
Ileal stenosis in Crohn's disease
Radiography
In the early stage of obstruction, plain radiographs in the supine position will show moderately distended loops of the small intestine with a small amount of air. When shooting in a standing position or on the left side, multiple gas-liquid levels are determined. Kerkring's folds are visible in the early stages; as the obstruction progresses, the loops stretch and the folds become blurred. Sometimes it is very difficult to distinguish swollen loops of the small intestine from the large intestine.

Plain radiography of the abdomen in a standing position

Plain radiography of the abdomen in the supine position
CT imaging with a simple form
Surgical classification of small bowel obstruction is also the basis of the classification used in radiology. There are three forms:
- simple/compensated form
- decompensated form
- complicated form.
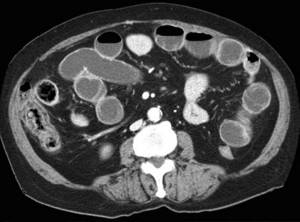
-Dilated loops of the small intestine proximal to the transition zone (obstruction zone). -The transition zone should be understood as a zone of the intestine with an obvious difference in lumen diameter between the dilated proximal segment and the site of narrowing/obstruction. Visualization of this area depends on the cause and mechanism of the obstruction, as well as on the projection of the loop location (axial, frontal, etc.). Unfortunately, detecting this zone is not always possible. With an adhesive mechanism or inflammation, the sign of a “bird's beak” is well described by many. With obstruction as a result of a nutritional bolus, the transition zone will appear as a heterogeneous formation in the intestinal lumen without signs of contrast enhancement. - Collapsed loops of intestine distal to the level of obstruction. -Mixed nature of stasis of intestinal contents in dilated loops. Some authors have described the “fecaloid” type of stasis, described in the literature as “fecal contents of the small intestine”, in English literature as “small-bowel faeces sign”. The pathogenesis of this symptom includes many factors: slowing down the passage of contents, disturbances in the mechanisms of absorption and secretion in the small intestine, reflux from the colon due to insufficiency of the ileocecal valve, placement of a gastric tube. It must be remembered that this sign is nonspecific for small bowel obstruction; it can also be determined by ultrasound and plain radiograph of the abdominal cavity. -Normal non-thickened intestinal walls with homogeneous, uniform contrast enhancement. -In the jejunum, the pattern of mucosal villi (valvulae conniventes) is thin, and they look the same throughout. -Absence of pathological changes in the colon, the colon is usually collapsed or contains a small amount of fecal contents distributed throughout the lumen. - Absence of inflammatory changes in the mesentery and intraperitoneal fat. -Normal vascularization of mesenteric vessels. -Lack of free fluid in the abdominal cavity.

Various CT scans for a simple form of obstruction, schematically depict transient zones and adhesions, which, like a “collar” or “noose”, seem to strangle a loop of intestine.
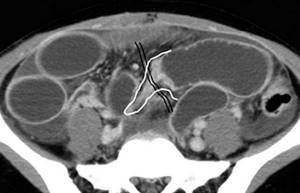
The value of reconstructions in different projections to determine the level of obstruction.

Obstruction of the lumen by phytobezoar.

Obstruction of the lumen by phytobezoar.
Causes and types of acute intestinal obstruction
Depending on what caused its development, there are:
- Dynamic or functional obstruction. It develops due to a violation of intestinal motility - its spasm or paralysis.
- Mechanical intestinal obstruction. It develops due to the closure of the intestinal lumen and the impossibility of transit of its contents. Here they distinguish:
- Strangulated intestinal obstruction, from the Latin strangulatio - strangulation. It develops due to compression of the intestine or its mesentery, as a result of which the blood supply to the intestine is disrupted. This is a very dangerous condition as it can lead to necrosis of the intestinal wall.
- Obstructive intestinal obstruction. Develops due to blockage (obstruction) of the intestinal lumen by foreign bodies (calculi, parasites), tumor or scar deformation.
Depending on the site of development, colonic and small intestinal obstruction are distinguished.
In oncology, intestinal obstruction most often has an obstructive nature and develops as a complication of colorectal cancer, when the tumor blocks the lumen of the colon, usually in its terminal stages. Obstruction can also develop as a result of compression of the intestine by a tumor of another organ, for example, the uterus or prostate gland.
Small intestinal obstruction occurs less frequently. As a rule, its cause is carcinomatosis of the visceral peritoneum. Primary tumors in this region are extremely rare.
Decompensated form
All the signs described in the simple form are determined, additionally pathological changes appear in the abdominal cavity: - dilated loops of the small intestine proximal to the transition zone (obstruction zone); -collapsed intestinal loops distal to the level of obstruction; - normal, non-thickened intestinal walls with homogeneous, identical contrast enhancement; - free fluid between dilated loops of intestine, often in the form of a piquant detail of a woman’s toilet - tanga panties, therefore in many sources it is described as a sign of “tanga” (tanga sign); -free fluid in mesenteric pockets; -free fluid in the abdominal cavity.

Examples of fluid accumulation between intestinal loops (tanga) and in mesenteric pockets in the decompensated form.

Features of colonoscopy
The procedure is carried out using an endoscopic device - a colonoscope. The main feature is the need for careful preparation, including a special diet and taking medications that help cleanse the intestinal mucosa. Preparation lasts at least 2 days.
The study reveals:
- Oncological diseases.
- Sources of intestinal bleeding.
- Assess intestinal motility.
- Diagnose inflammatory processes in the intestine.
Complicated form (most often as a result of strangulation)
Strangulation of the small intestine is characterized by thickening of the intestinal walls, vascular disorders and pronounced pathological changes in the mesentery and abdominal cavity. Diagnostic findings include: - dilated small bowel loops proximal to the transition zone (obstruction zone); -collapsed intestinal loops distal to the level of obstruction; -transient zone; - mixed nature of stasis of intestinal contents in dilated loops with a predominance of the liquid component; -thickening of the intestinal wall of a circular type. It is important to remember that this type of thickening of the walls of the small intestine with obstruction is usually associated with vascular disorders; - disruption of normal contrast enhancement of the intestinal walls. Changes range from hyperenhancement to no contrast enhancement at all. Various variations of these changes between the extremes described above can be observed simultaneously in different segments of the small intestine. The complete absence of enhancement means arterial reflex spasm and indicates the severity of the lesion; - a loop with thickened walls loses its elasticity and becomes rigid and elongated; - parietal pneumatosis of the small intestine, in especially severe cases intramural gas bubbles appear; - the appearance of pathological densities in the mesentery in the form of spreading matte infiltrates and heaviness due to hemorrhages into adipose tissue; - congestive changes in the vessels of the mesentery. At first, the diameter of the vessels increases, but over time, a reflex arterial spasm occurs, the mesentery will look depleted in vascularity. The vessels are narrowed or with a completely collapsed lumen; -gas in the lumen of the superior mesenteric vein; -gas in the lumen of the portal vein; - with torsions, the normal vascular anatomy of the mesentery is disrupted. The vessels seem to twist around the volvulus axis and pull along the modified mesenteric fat - like a snail shell or a tornado. For greater clarity, imagine a piece of straightened fabric on the table, which you pressed with your finger and began to twist without lifting your finger from the table. On CT scans you can often see a characteristic sign of a cone-shaped spiral (whirl sign); -free fluid in the mesenteric pockets and in the abdominal cavity. Sometimes the liquid may be of increased density due to the hemorrhagic component.
examples of strangulation complicated obstruction with characteristic changes in the mesentery, intraperitoneal fat, thickening of the walls of the small intestine and impaired contrast enhancement.
Twisting of the vessel during volvulus
Preparing for an abdominal x-ray
If there are food residues and excess gases in the gastrointestinal tract, it will be difficult to determine the condition of the internal organs.
Therefore, 2-3 days before the x-ray, follow a diet. You should eat foods that do not cause increased gas formation.
12 hours before the x-ray you need to stop eating solid food, and two hours before the test you need to cleanse your intestines.
Please check with the clinic administrators, contact center operators or your attending physician for all information.
Ultrasound signs of small bowel obstruction
The main ultrasound signs of obstruction are visualization of dilated loops of the small intestine, decreased peristalsis, free fluid between the loops (tanga) and in the abdominal cavity. Also, ultrasound can sometimes detect the cause of the obstruction, for example, a tumor, thickening of the walls of the terminal segment of the ileum in Crohn's disease, etc. Ultrasound can solve the diagnostic dilemma when there are ambiguous radiological signs on a plain abdominal radiograph. The limit of the method is the low specificity in assessing the condition of the mesentery, as well as the dependence of the quality of diagnosis on the patient’s constitution and the operator’s experience.
The topic of intestinal obstruction as a result of intussusception will not be covered in this review; it is well described in many domestic and foreign publications. I think that all colleagues dealing with this problem know that ultrasound diagnostics is of decisive importance in the diagnosis of intussusception. An indicative observation was previously posted on our website:

examples of sonograms with dilated loops of the small intestine

Ultrasound makes it possible to perfectly locate free fluid in the abdominal cavity
Preoperative testing
If you have symptoms of a bowel obstruction, your doctor will do a physical exam to check your stomach and bowel sounds.
Diagnostic evaluation may include an abdominal x-ray, computed tomography (ultrasound) scan, or ultrasound. These tests may or may not include a barium enema, which involves injecting a small amount of contrast material into the rectum to better visualize the structures.
If you have a blockage, you may also need a sigmoidoscopy or colonoscopy, which are invasive diagnostic procedures in which a camera is inserted into the colon to visualize the blockage.
Paralytic ileus
Paralytic or adynamic obstruction means a violation of passage through the intestines without the presence of mechanical obstruction of the lumen as a result of a decrease or complete absence of intestinal tone and peristalsis. Both the small and large intestines may be affected. Involvement of the stomach in the process reflects the seriousness of the situation. Paralytic ileus presents with complex radiological symptoms. We will limit ourselves to listing the main points that are always visualized in this pathology: - expansion of the intestinal lumen; - intestinal stasis with a predominance of the liquid component and air levels; -decreased tone and peristalsis. Dynamic monitoring of the listed signs is very important, which gives the palm to ultrasound as the most adequate and safe visualization method for adynamic obstruction.
Procedure parameters
There are several options for surgical treatment of intestinal obstruction. Surgery is usually urgent, which means you may have surgery within a few hours or a few days after you are diagnosed with a bowel obstruction. Some medications may help with nausea, but they do not prevent bowel obstruction from getting worse or better.
Ideally, you should not eat or drink for about eight to ten hours before this type of surgery, but due to the urgency, preoperative fasting is not always possible. Surgery for bowel obstruction is usually performed under general anesthesia in the operating room.
You may have open surgery with a large incision or minimally invasive surgery with several small incisions and a camera for imaging. It depends on the location, size and cause of the intestinal obstruction. Large tumors or widespread adhesions may require an open procedure, while a small tumor or infection may be treated with minimally invasive surgery.










