The essence of the radiography method
The basis of X-ray examination is the use of the characteristics of X-rays when exposed to the human body: the human skeleton and other dense tissues of the body absorb a much larger amount of radioactive particles when irradiated than soft tissues.
This makes it possible to obtain X-ray images in which dense tissue appears in white, while soft tissue and air-filled body cavities appear in shades of gray. Modern radiographic equipment allows for high-precision studies thanks to the latest methods of creating digital images. Obtaining an image after the procedure takes only a few minutes, and the image quality significantly exceeds the quality of images obtained with analog devices.
X-ray or CT scan of the lungs and bronchi, which is better?
Both X-rays and CT scans are used to diagnose lung diseases.
What to choose - X-ray or CT - this question often arises when it is necessary to undergo a chest examination. X-ray is a more common and accessible method. CT is a modern type of x-ray examination method.
Both X-ray diagnostics and tomography are successfully used in examining the lungs and bronchi. Both methods are based on the use of X-rays, which makes their wider use difficult because There are contraindications in both cases, despite the fact that modern devices have made it possible to significantly reduce the dose of ionizing radiation received.
The X-ray method is more often used for preventive, mass examinations (fluorography) and as a primary diagnosis. CT is a method of a higher, expert level, and is more often used for clarifying diagnostics.
There are other significant differences between these methods :
- X-ray allows you to obtain only one image of an organ in one plane. Using CT, a set of layer-by-layer images is obtained at different slice levels, which can be combined into a three-dimensional image using a computer program. With this image of the organ at different levels, the presence of “blind” spots is eliminated.
- With CT of the chest, thanks to the use of multislice scanning (MSCT), clearer images are obtained; there is no effect of “overlaying” denser tissue (bone) on less dense tissue (pulmonary). The attenuation coefficient for CT is 0.5%, for X-ray – 20%, i.e. tomography has a higher tissue resolution, providing greater data accuracy.
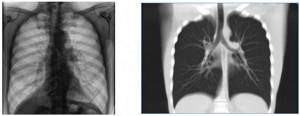
X-ray of the lungs - normal (left) CT scan of the lungs - normal (right)
- Scanning speed : CT allows you to conduct an examination in 3-5 minutes, which is especially important for patients in serious condition, children, patients on mechanical ventilation.
- To examine the lungs using radiography, it is necessary to take pictures in two projections to determine the location of the pathological focus. With CT, layer-by-layer scanning of an organ with a slice thickness of 1-10 mm makes it possible to detect a pathological focus of small size, determine the nature of the disease and the stage of its development, makes it possible to clearly localize the object, determine its size and boundaries.
- X-ray is a cheaper method (300.00-700.00 rubles), available to almost all patients free of charge under the compulsory medical insurance system. Computed tomography of the chest organs will cost several times more (4000.00-6000.00 rubles), but it will be more informative than the usual x-ray at the nearest clinic.
- CT allows you to examine the lungs during breathing movements.
Doctors prescribe the examination method, taking into account the advantages and disadvantages of each method.:
- If pneumonia is suspected, an x-ray or digital fluorography is performed first. CT is indicated if complications develop 4–10 days after the start of treatment, there is no positive effect from the therapy, or pneumonia often recurs. The same tactics are used when diagnosing coronavirus pneumonia - in the first 2-4 days after infection, there may be no pathological signs on CT.
- CT is prescribed to confirm tuberculosis when initial radiography does not provide clear data or when it is necessary to distinguish tuberculosis from pneumonia.
- For pulmonary edema, a more informative method would be plain radiography.
- It is more advisable to start the examination immediately with CT , because the method is more informative: if the presence of neoplasms is suspected,
- for inflammatory infectious diseases of the lungs (bronchiolitis, aspergillosis),
- if foreign bodies in the bronchi are suspected, because Not all objects can be identified using X-rays,
- HIV-infected patients with suspected tuberculosis,
- with purulent-necrotic processes in the lung.
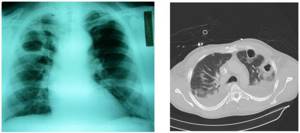
Decay cavities (abscess) in the lung with X-ray (left) and CT (right)
CT scans are carried out only according to medical indications; this study is not recommended to be performed frequently, therefore it is not used for mass examinations. Fluorography is used for preventive purposes.
How is radiography performed?
Carrying out an X-ray examination does not require the patient to change his usual lifestyle, any preliminary preparation or special diet.
During the procedure, the patient should:
- undress to the waist or leave only simple underwear without various solid elements - buttons, fasteners, etc.;
- remove all metal jewelry;
- hold the breath;
- do not move.
If you violate these instructions, the image may turn out to be inaccurate - solid objects will be irradiated and will interfere with the detection of pathologies in the body, and the expansion of the lungs during breathing will create the effect of dynamic blurring - the contours will be too blurry to make a diagnosis. Follow your doctor's instructions so you don't have to go through the procedure again.
Visualization of bronchial diseases (part 1)
Transcript of the first part of the video lecture by Professor Igor Evgenievich Tyurin on the visualization of bronchial diseases from the second program of the radiology diagnostics for therapists series.
Igor Evgenievich Tyurin, professor, doctor of medical sciences:
— Good afternoon, dear colleagues. We continue our sessions on radiation diagnostics of respiratory diseases.
As usual there must be two people in this studio. My name is Igor Evgenievich Tyurin. I head the Department of Radiation Diagnostics at the Russian Medical Academy of Postgraduate Education. My colleague who traditionally conducts these sessions with me is Irina Aleksandrovna Sokolina.
Today we are talking about a very interesting, relevant and extremely important from a practical point of view problem concerning radiation diagnostics and clinical medicine. This is a visualization of bronchial diseases in the broadest sense of this concept.
We will talk not only about chronic or obstructive pulmonary disease, but also about bronchial pathology in general, in principle, from the point of view of radiodiagnosis, assessment of these pathological conditions using various imaging methods.
We will pay the main, perhaps the greatest, attention to conventional x-ray examinations, as is generally accepted in pulmonological practice. But we will also talk about modern technologies, such as computed tomography (CT), first of all, about the significance of this technology for assessing the condition of the bronchi.
Before we start talking about obstructive pulmonary diseases (since we devoted the last session entirely to the pathology of the mediastinum, and this time we are moving on to the pathology of the respiratory organs), I will say a few words about the fundamental radiological approach and the approach of radiation diagnosticians to the interpretation of pulmonary pathology (in this case of pathology of the lung as an organ) to the changes that we observe in various types of x-ray studies.
From the position of X-ray diagnostics, we can distinguish various syndromes and treat most pathological processes from the position of syndromic diagnosis. If we try to systematize these changes in the lung tissue, we can identify two or even three large groups of radiological syndromes.
The first of them is designated differently. But the point is that the amount of air in the lung tissue decreases. For some reason, the density of lung tissue increases. It blocks X-ray radiation to a greater extent. As a result, a corresponding skeological picture arises.
Increased density, decreased airiness. Shading in the most general sense of the word, which can cover the entire lung or almost the entire lung, part of the lung, represent rounded or irregularly shaped formations in the lung tissue, or are depicted as multiple foci, from large to billions.
Any compaction in the lung tissue, of any shape, of any size, which leads to a decrease in the transparency of the lung fields.
03:44
The second large group of radiological syndromes or pathological conditions that will be discussed today is, on the contrary, an increase in the airiness of the lung tissue or an increase in density or clearing. If we talk about ideological terminology, which can also involve the lung or part of the lung, or represent separate air cavities or cystic formations in the lung.
These changes most often occur as a result of excess air accumulation in the lung tissue. As part of anatomical changes and as part of functional disorders. With X-ray examination, we see a significant part of these changes quite clearly.
In addition, we can talk about the pathology of the pulmonary pattern. Or in CT now they call it reticular changes. Changes that are localized not in the alveoli or even inside the alveoli, leading to displacement or, conversely, accumulation of air in the lung tissue, but rather to a pathology of the lung frame, pathology of the pulmonary interstitium.
Hence, reticular, interstitial changes in conventional X-ray examination on conventional radiographs are often defined as a pathology of the pulmonary pattern.
These three components of radiological syndromes can be referred to by different terms. In different textbooks and books you will find different definitions. But in principle, probably, most pulmonary pathologies fit into these anatomical concepts.
On the other hand (this is very important in relation to our conversation today), X-ray and CT, and any other tomographic study has the goal of identifying anatomical changes in the lung tissue. But there is also a functional component.
All pathological changes that occur in the chest cavity and in the lung tissue, including, can also be considered from the point of view of dysfunction of certain anatomical structures.
05:57
As a rule, in X-ray diagnostics and radiation diagnostics, we distinguish two large groups of pathological processes that are associated with a global change in function. These are changes in the bronchial tree, changes in the airways, which are most often realized in the process of obstruction, local or generalized.
This is an obstructive syndrome, ultimately. It most often leads either to an increase in the airiness of the lung tissue as a whole, or to some local changes, which we will probably talk about in future lessons.
The second group of pathological processes is a violation of the pulmonary circulation. Something that is associated with local changes inside the vessels (pulmonary embolism). Generalized changes that occur during pulmonary edema and other pathological processes.
Functional disorders leave a very large imprint on the anatomical and morphological signs, which we usually identify during x-ray examination.
Today we decided to start our conversation with such not only anatomical, but also to a large extent functional concept as the pathology of the bronchi, large, small, medium-sized, but pathological conditions, where anatomical changes in the bronchi themselves and lung tissue, on the one hand. Functional manifestations that we do not always see as separate anatomical manifestations.
As for visualization, methods, research techniques that are acceptable and used today to assess the condition of the bronchi, bronchial tree and the function of the respiratory system in general...
X-ray as the main first-line method, as a way to obtain an image of the entire chest cavity and both lungs in order to evaluate or identify pathological changes.
08:07
Direct, anterior or lateral projection is usually used to fully characterize the condition of the lung tissue. X-ray functional studies used to be really extremely popular (in the 1970s, 1980s).
Starting from the simplest breathing test, when a picture is taken or fluoroscopy is performed during inhalation and exhalation, the mobility of the diaphragm and the transparency of the pulmonary fields are assessed. Finishing with very complex technologies, such as linear pneumopolygraphy or tomorespiratory test. Doctors of the older generation probably remember such unique techniques.
Today this is used relatively rarely. These X-ray functional techniques have largely come under the purview of CT. Linear tomography today is used for this purpose very rarely, as an exception. Tomographic studies, if used to assess the bronchial tree, are often CT studies.
In any case, we would like it to be so. If the attending physician or radiologist considers it necessary to perform a tomographic examination of a given patient, then it is better to perform a CT scan in that situation in order to obtain more objective, more valuable information about the nature of pathological changes.
As for CT, there are two main technologies - high-resolution CT (step-by-step technology) and multilayer CT (spiral scanning technology) - I’ll tell you a little more about it. Specifically for assessing the condition of the respiratory system.
(Slide show).
If we are talking about radiography, then these are two standard ordinary radiographs of the chest organs. There is nothing surprising about them. During X-ray examination, we highlight the middle shadow, which we discussed in great detail in the last session.
On both sides of it there are pulmonary fields, against the background of which images of the ribs and images of the pulmonary pattern are visible. This is a distomic division of vascular structures from the root of the lung and towards the chest wall, towards the visceral pleura. Gradually decreasing in size intrapulmonary vessels, arterial and venous, which create a kind of delicate, sometimes quite clearly visible vascular network on x-rays.
10:48
This is a normal picture. It is perceived by radiologists and pulmonologists as a normal, unchanged X-ray picture of the condition of the chest organs.
There are a huge number of structural options and images of the organs of the thoracic cavity.
(Slide show).
I deliberately did not transform these images in any way into a negative form, as happens with radiography, but show what is sometimes or often obtained during fluorographic studies. In particular, with digital fluorography, where some radiologists prefer positive images.
Two images of completely normal lungs. But constitutional features are of enormous importance in the depiction of lung tissue, pulmonary structures, the location of the diaphragm, and the configuration of the chest cavity. All this affects the severity, nature of the vascular pattern, pulmonary pattern on x-rays.
The same thing applies to the severity of the vascular pattern itself. Here, radiologists themselves sometimes sin with some overdiagnosis, naming various variants of the structure of the vascular pattern. Especially where it is overly expressed. Strengthening the pulmonary pattern or some other abstract general terms, behind which, as a rule, there are no pathological processes.
Other radiological signs such as emphysema or pneumosclerosis. There are a huge number of such variants of the structure of the vascular pattern in the lung. One must be very careful not to over-diagnosis when interpreting anatomical structures.
12:45
As for thin-layer CT or high-resolution CT, today it is of great importance in interpreting the nature of changes in lung tissue in bronchial pathology and obstructive pulmonary diseases. This is usually a study with a layer thickness of 1 mm, which is very often performed using a special high-resolution algorithm of this technology. Hence the name of this technology.
Two main options. A step-by-step protocol that can be implemented on any CT scanner. Helical scanning, which requires a CT scanner with a multi-row detector. Or it is now called a “multi-slice” or “multi-slice” CT scanner.
What is the meaning of the usual classical high-resolution CT scan of the lungs. It consists in the fact that we make an nth number of tomographic slices. Usually 20, 22, 25 sections through the entire volume of the lungs. But between these tomographic slices there is a distance of 10, sometimes 15 mm.
The study is done while inhaling. Sometimes on inhalation and exhalation to obtain an assessment of respiratory function. But the end result of this procedure is a relatively small number of tomograms that allow us to assess the condition of the lung tissue.
Multi-slice CT, which is performed on tomographs with a multi-row detector, allows one to obtain an image of the entire chest cavity during one breath-hold. After the scanning process is completed, divide the volume of tomographic data into individual tomographic layers of a certain configuration, a certain specified value that we want to obtain as a result of this. Thus, obtain a large number of thin tomographic sections through the entire volume of the chest cavity.
Step by step protocol. Its advantage is a small number of tomographic slices and a relatively high research speed. This is a test that is usually performed on the back. Hold your breath in the supine position with a held inhalation. But this may be a study in the prone position.
Expiratory examination, when we conduct X-ray studies in this way. All the possibilities that we get in this case. They are usually sufficient to assess the nature of the pathology of both the bronchial tree and lung tissue. But the advantage that helical scanning gains is very significant today, which is why we are using it more and more.
15:37
A large number of adjacent tomograms, which are performed through the entire volume of the chest cavity, make it possible to obtain thin submillimeter tomographic slices with very high resolution. We get the opportunity to carry out various types of reformation (two-dimensional, three-dimensional), and measure the thickness of the tomographic slice.
Thus, obtain multi-projection images, including those similar to conventional linear tomograms. We can combine high-resolution CT with the injection of a contrast agent, that is, in fact, with performing CT angiography. For example, when it comes to the differential diagnosis of pathology of the bronchial tree.
Pulmonary embolism, which can have very similar clinical manifestations and manifest very similar radiological changes on X-ray and CT.
Why are we talking today that 3D and 2D transformations are important. The bronchi, as well as the vascular structures of the thoracic cavity, are mostly oriented perpendicularly or at an angle to the axial scanning plane. In order to assess the course, size, and configuration of the bronchial branches, we need to sequentially view a large number of oxal sections. If it is a multi-slice CT scan, then the number of such slices can be 200, 250, 300, or even more. It takes time.
But if you look at this reformation in the frontal plane, then this immediately gives us in one image a detailed description of the nature of the pathological process. In this case, these are dilated, deformed, cylindrical bronchiectasis in the lower lobe of the left lung with fibrotic changes in the area of the costophrenic sinus on the left.
To do this, you do not need to view a large number of tomographic slices step by step. The prevalence of the disease, localization of changes, and character are visible very well and in detail on one or two diagnostic images.
17:50
Now, with the advent of new technology and more modern devices, patients with pathology of the bronchial tree are increasingly resorting to precisely this technology.
Another feature is the ability to perform functional studies. They were very popular in their time for routine x-ray diagnostic examinations. Their meaning is that we do a study on inhalation and exhalation and compare the results obtained.
But with CT, these results are much more objective and visual. Today we are resorting to their help more and more often.
A study at the height of delayed expiration is traditionally called expiratory CT. It is used most often in obstructive pulmonary diseases to identify areas of valve swelling.
This is the most important tool for the differential diagnosis of obstructive disorders that occur in diseases of the bronchi, changes that are observed in pathology of the pulmonary circulation. Especially in cases of chronic thrombolic pulmonary hypertension. Interstitial lung diseases, which can also be accompanied by very similar clinical symptoms, radiological, tomographic signs. This is where these technologies are very important.
(Slide show).
What do we see in this situation? We are observing two identical tomographic slices. If during inhalation, the pathological zone can be difficult to predict due to the greater or lesser severity of the pulmonary pattern. When examined during exhalation, the lung tissue reduces airiness. It becomes lighter.
In those areas where bronchial patency is impaired, where air during exhalation cannot leave the alveoli and remains there, just as during inhalation examination. We see darker areas. They are clearly demarcated from healthy, unchanged lung tissue. They have subpleural localization.
We have the opportunity to see and clearly delineate the boundaries of these areas with extreme precision.
20:06
If we are talking about the treatment of such a patient, then we can observe in dynamics how much these areas change in size (reduce or remain the same). This has a certain significance for assessing the effectiveness of the treatment as an additional procedure for assessing the function of external respiration.
Why? Here we see local changes. Not integral indicators, but changes localized in certain lobes and segments of the lung, which is sometimes of fundamental importance.
After a brief excursion into the syndromes and methodological features of performing CT and conventional x-ray examinations, I will allow you to start talking about chronic obstructive pulmonary disease and obstructive diseases in general. About how they can fundamentally be depicted during X-ray and tomographic examination.
I'll start with the standard definition that is familiar to all of you. It suggests that obstructive pulmonary disease is a chronic inflammatory disease with predominant damage to the distal respiratory tract, the lung parenchyma. Characterized by air flow limitation.
It is fundamentally important for us that this definition combines three different components of chronic obstructive pulmonary disease. On the one hand, these are clinical manifestations in the form of a chronic inflammatory disease.
On the other hand, these are anatomical changes and their localization in the distal parts of the respiratory tract and lung parenchyma.
Thirdly, this is a functional characteristic.
When we talk about the meaning, the purpose of any x-ray or radiation study in relation to obstructive diseases, in particular chronic obstructive pulmonary disease, we must understand that these advantages, these tasks are localized primarily in the middle part of the definition. When we talk about anatomical changes in the chest cavity associated with the development of obstructive disease.
22:14
To a lesser extent, this concerns the clinical characteristics of this condition. To a lesser extent - functional characteristics. In many cases, we have the opportunity to assess the functional state of the lung tissue and make fairly accurate correlations between the X-ray picture and the function of external respiration.
Why is it generally necessary to perform X-ray or tomographic studies in patients with obstructive diseases, possible, suspected or already reliably known?
Strange as it may seem, these studies are most often carried out or prescribed not so much to confirm the disease itself, but to exclude other pathological conditions that may have similar clinical manifestations.
This is true. In most patients who develop a chronic cough or shortness of breath that is difficult to explain clinically, an X-ray examination is performed primarily to rule out other diseases. Such as accumulation of fluid in the pleural cavity, malignant neoplasms, tuberculous infiltrate or some other vital pathological processes that are not always easy to distinguish clinically from obstructive pulmonary diseases.
The second targeted study of obstructive pulmonary disease itself is undertaken in the case when we want to identify individual components of the anatomical lesion, anatomical changes in the chest cavity in these pathological conditions.
Here we will talk about two main types of pathology. This is emphysema. Every time we try to find signs of emphysema as an anatomical and morphological condition on X-rays and CT scans.
On the other hand, it is the identification and determination of the localization of bronchiectasis, which is important both for the management of this kind of patients and for determining further diagnostic tactics.
Today Irina Aleksandrovna will talk in more detail about bronchiectasis. I will show some slides in a moment regarding the diagnosis of emphysema from the perspective of conventional x-rays and CT scans. But this is a possible indication for diagnostic radiation studies. Detection is more difficult.
I would venture to suggest that most patients with obstructive pulmonary diseases find themselves in X-ray rooms or CT rooms precisely at the moment when they experience a complication or exacerbation of the underlying disease of the pathological process.
At this moment, the radiologist and the attending pulmonologist need to resolve the question: is this an exacerbation of the process itself or is it a complication of something else. First of all, these are infectious complications (pneumonia). This is an infectious process in the lower respiratory tract, such as bronchiolitis, which today is quite confidently and clearly detected using CT.
This is the formation of pneumothorax, which worsens the patient’s condition, changes the clinical picture, and so on.
Safety of the procedure
Modern devices used in NEARMEDIC clinics allow minimizing the dose of radiation received, which allows radiography even for a child.
For comparison, outdated devices expose a patient to a radiation dose of 0.3 m3v, while in Russian medicine the permissible annual dose is 1.4 m3v per person. Modern equipment irradiates the body with a dose of 0.03 m3v - this is the dose received by a person during a normal lifestyle in 10 days.
However, since each organism is individual, the decision on the advisability of the procedure is made by the doctor. For pregnant women and children, as well as patients with poor health, x-rays are prescribed only when absolutely necessary.
Differences between radiography and fluorography
Today, fluorography is used by doctors mainly for prevention, while x-rays are a highly effective method for diagnosing various diseases. Due to its higher danger to the body, fluorography is prohibited for children under 15 years of age, but there are no such restrictions for radiography.
Also, fluorography provides much less accurate results without obtaining digital images and without the ability to track the smallest changes in the organs being examined. For these reasons, in modern medicine, fluorography is recognized as a somewhat outdated method for diagnosing diseases.
Bronchial tree in the human body
The function of the bronchi is to conduct air flow into the lungs, as well as to warm, cleanse and moisturize it. The bronchi are a tubular ventilation system formed from tubes of decreasing length and diameter that flow into the alveolar ducts.
Diseases of the bronchi, such as bronchial asthma, acute and chronic bronchitis or fungal diseases of the bronchi, can put an end to a carefree life, causing the patient to feel constant discomfort, pain, and also pose a danger to the patient’s life. Diseases of this group can develop into more severe forms if they are ignored, so it is very important to prevent their development by correctly diagnosing the disease. Once a diagnosis is made, an effective treatment regimen is developed and problems are eliminated.
An X-ray of the bronchi is carried out as follows: during the procedure, the X-ray tube approaches the bronchial tree, which focuses the device on the desired area. This method allows you to obtain a highly accurate image of the bronchial tree with detection of changes less than 1 mm. A high-quality x-ray allows you to:
- get an idea of the structure of the organ and its changes;
- identify inflammatory processes in the bronchi;
- monitor the patency of the contrast agent (if one is used during treatment);
- identify signs of airway obstruction;
- to differentiate diseases with similar symptoms, for example, bronchitis and pneumonia, taking into account the peculiarities of changes in the organ during the disease.
Radiographs can be taken at different times to obtain a detailed picture of the course of the disease and the results of the therapy used.
What X-Rays Don't See: Pulmonary Function Testing
Once in the hospital, during educational supervision, a patient told me: “The doctor ordered some kind of test - the function of external respiration. Is this an exhalation to explore, or what? Why external? Let's figure out what kind of breathing happens, what external breathing is and why study it.
What is a "function"?
Respiratory processes in the body are divided into two large groups. The first is internal respiration, which includes tissue (transfer of oxygen from blood to cells) and cellular (utilization of oxygen inside the cell). The second is external respiration, which combines the processes of air entering the pulmonary alveoli and gas exchange in them: the entry of oxygen into the blood and the extraction of carbon dioxide from it.
The main function of the respiratory system is to provide the body with oxygen in accordance with the current need. It is obvious that if a person has structural damage to the respiratory apparatus (anything - an abscess in the lung tissue, a foreign body in the bronchus, broken ribs, paralyzed respiratory muscles), then this function will be impaired. Such damage is clearly visible on X-ray, CT or MRI.
But there are situations when the x-ray picture is normal, and the patient complains, for example, of difficulty breathing. That is, there is a violation of the respiratory function, but without structural damage to the respiratory apparatus. What to do in this case?
Volumes and speeds
Here doctors have to turn practically into physicists - to establish a diagnosis, they need to study the movement of air through the system of tubes that form the respiratory system: the trachea and bronchi of various sizes. What matters is both the volume of air that a person can inhale or exhale and the speed at which he does it.
All these indicators are studied using methods such as pneumotachometry, peak flowmetry and spirography. The pneumotachometer measures the volumetric velocity (i.e. liters per minute) of air exhaled during so-called forced expiration. The patient is asked to inhale as deeply as possible and exhale strongly and sharply into the “neck” of the pneumotachometer. To ensure that the air comes out only through the mouth, they put... a clothespin on the nose.
With peak flowmetry, the same thing happens, but, unlike pneumotachometry, you can immediately find out not only the maximum expiratory flow achieved, but also the expiration time, the volume of exhaled air and the volume of air exhaled in the first second (a parameter that is one of the key ones in making a diagnosis "bronchial asthma").
Spirographic research is the most voluminous. The patient is asked to take a series of calm inhalations and exhalations, then a maximally deep inhalation, ending with a maximally sharp exhalation, followed by several more calm inhale-exhale cycles. But here the most data is obtained: in addition to the indicators already listed, the doctor finds out the vital capacity of the lungs, reserve volumes of inhalation and exhalation (they reflect the functional reserves of the respiratory system) and much more.
Types of respiratory dysfunction
There are only three of them, and you know one for sure: the phrase “bronchial obstruction” is very popular with local doctors, especially pediatricians. Obstruction means “blockage, narrowing.” The term refers specifically to the bronchial tree, or more precisely, to a decrease in its patency. Obstructive type disorders are characteristic primarily of bronchial asthma, as well as obstructive bronchitis, a number of chronic diseases and certain stages of pneumonia and ARVI. The study will show a decrease in speed indicators, especially expiratory speed, and the changes will vary depending on what caliber bronchi are affected: large, medium or small (terminal).