A rib fracture is a violation of the anatomical integrity of bone tissue as a result of a blow to the chest area, a fall or strong compression.
The danger of such an injury is associated with a high probability of damage to internal organs, which can lead to serious pathologies and even death.
Treatment of a rib fracture
Immediately after injury, painkillers are used. The victim must be immobilized and a pressure bandage applied to the chest. By the way, this should be treated with extreme caution so as not to provoke lung damage and the development of pneumothorax.
If there is a suspicion of a rib fracture, you should contact the clinic. The doctor will examine the patient, check the auscultation of the heart and respiratory system, measure the pulse and pressure. The patient will then need to have an x-ray taken.
Outpatient treatment is allowed if no more than two ribs are damaged; in other cases, hospitalization is provided.
After diagnosis, the doctor prescribes comprehensive drug treatment to block pain and reduce inflammation. In the future, expectorants, heat compresses, and physiotherapeutic procedures are used.
As for complications, a fracture may cause hemothorax (accumulation of blood in the pleural area) and pneumothorax (concentration of air). In order to remove such accumulations, a puncture is performed.
In case of pneumonia development, in addition to basic treatment methods, antibiotics are used.
Monitoring a patient with a rib fracture over a long period of time

Ultrasound scanner HS50
Affordable efficiency.
A versatile ultrasound scanner with compact design and innovative capabilities.
Introduction
Patients with rib fractures periodically turn to ultrasound diagnostics (USD) doctors, and the diagnosis of a fracture depends largely on the doctor’s skills and the thoroughness of taking an anamnesis. Unfortunately, the doctor’s communication with the patient, especially in large numbers, is reduced to a minimum: for example, having learned from the patient that his “side hurts” and having no information about the existing injury, it is impossible to assume the presence of a rib fracture, and the doctor will most likely limited to examining the kidneys. But the ultrasound method for rib fractures has many advantages that we forget about, such as the speed of the study, the absence of radiation exposure and the need to prepare for the study [1, 2]. In our clinic, surgeons began to use the ultrasound method as a screening method to determine quick tactics for the patient.
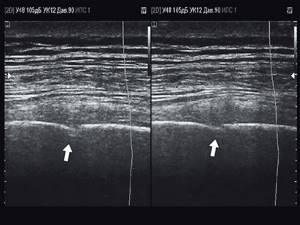
The radiology literature describes in great detail the changes that occur in bone tissue during rib fractures. Both in the literature on ultrasound diagnostics and in our practice, echograms of rib fractures and bone calluses formed at the fracture site are often encountered [3, 4], but mostly these are images of different patients. So, for example, in Fig. 1 and 2 show echograms of rib fractures identified primarily in our ultrasound office in 2021 in different patients. The purpose of this work is to familiarize the ultrasound physician with the different stages of healing of a rib fracture using the example of one patient.

Rice. 1.
Oblique fracture of the VII rib of the left half of the chest (indicated by an arrow).

Rice. 2.
Oblique fracture of the rib of the left half of the chest (indicated by an arrow).
Methods
The study was carried out on ultrasound scanners Accuvix-XG and HS40 (Samsung Medison) with linear sensors L5-13 IS and LA3-16 AD, respectively.
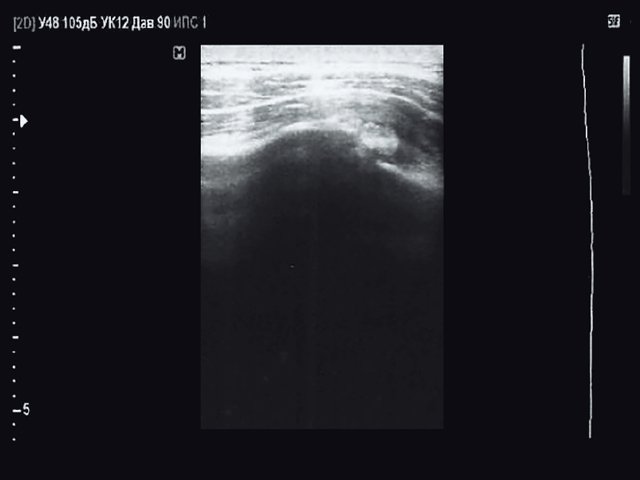
Patient Z., 30 years old, came to the ultrasound office on his own on 08/08/2018 with a bruise on the left side of the chest. The injury was received the day before while playing football. Ultrasound examination revealed no kidney damage, and, taking into account primarily the medical history, a small, depressed, non-displaced fracture of the VIII rib on the left along the posterior axillary line was detected (Fig. 3). The patient was referred to a surgeon for treatment.
15 months after the injury, the following photograph was taken (Fig. 4). Given limited time, it is not possible to say more than that the patient has a callus at the fracture site.
Rice. 3.
Destruction of the cortical layer of the VIII rib of the left half of the chest along the posterior axillary line (indicated by the arrow).
Rice. 4.
Bone callus 15 months after fracture.
The next photograph of the callus (Fig. 5) was taken 16 months after the injury and is more informative. The callus is visualized as an elongated formation 20 mm long, with an uneven, bumpy contour, the height of the callus above the expected contour of the rib is at least 5 mm (in the radiology literature, such a callus is described as a “muff”). When examining the patient in a standing position, a formation raised above the surface of the skin was observed at the site of the fracture, absolutely painless on palpation and not limiting the patient’s movement.

Rice. 5.
Bone callus 16 months after fracture.
The latest images dated August 20, 2020 (Fig. 6, 7) were taken 24 months after the injury. In Fig. 6, the callus is visualized during the period of disappearance, in a longitudinal projection, 19 mm long, with an even smooth contour, rising 1.7 mm above the expected contour of the rib. In Fig. 7, on the left the rib is located in the transverse projection next to the callus, 15 mm wide, on the right - the callus in the transverse projection of the rib, 19 mm wide. The location of the fracture was determined by palpation with great difficulty; the patient does not have any complaints.

Rice. 6.
Callus 24 months after the fracture, longitudinal view.
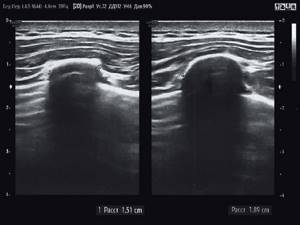
Rice. 7.
Callus 24 months after the fracture, transverse view.
conclusions
- Ultrasound is an excellent method for diagnosing bone changes in rib fractures. Since X-ray diagnosis of rib fractures is based mainly on determining the fracture line and displacement of fragments, echography has a number of advantages for the diagnosis of minor, subperiosteal fractures.
- In patients with rib fractures, even small subperiosteal fractures, the period from injury to callus formation to its disappearance can take up to 2 years or more.
- The ultrasound method is the method of choice as a screening diagnostic, as well as when examining heavy, bedridden patients, in conditions where their transportation is difficult, or in the absence of mobile X-ray equipment.
Literature
- Reinberg S.S. X-ray diagnosis of bone and joint diseases. M.: Medicine, 1964: 62–65, 110–112.
- Kishkovsky A.N., Tyutin L.A. Emergency X-ray diagnostics: A guide for doctors. M.: Medicine, 1989.
- Klyushkina Yu.A., Klyushkin R.M., Gazizyanova R.M. Sonography in the diagnosis of “undetected” rib fractures. Bulletin of modern clinical medicine. 2014; 7 (Supplement 2): 92–97.
- The role of ultrasound in recognizing chest injuries in combined trauma. Tukhtaev U.T., Afanasyeva N.I., Znamensky I.A., Yumatova E.A., Gorbunova T.S. Russian National Research Medical University named after. N.I. Pirogov. Department of Radiation Diagnostics and Therapy, Faculty of Pediatrics, Moscow, City Clinical Hospital // Bulletin of the Russian State Medical University. 2012; 1:30–33.
Ultrasound scanner HS50
Affordable efficiency.
A versatile ultrasound scanner with compact design and innovative capabilities.
Treatment

Treatment depends on the type and severity of the fracture:
- For cracks and ordinary fractures without displacement, a plaster splint is applied. The duration of wearing it depends on which bone is damaged, on average - 2 - 4 weeks.
- For displaced fractures, closed reduction can be performed: under local or general anesthesia, the doctor compares the fragments and immediately applies a plaster splint.
- Sometimes skeletal traction can be performed: a knitting needle is passed through the bone fragment, from which a load is suspended.
- For complex displaced fractures, open reduction and osteosynthesis can be performed: the doctor makes an incision, compares the fragments and fastens them using various metal structures.
- Sometimes the application of an Ilizarov apparatus or similar devices is indicated: needles are inserted through a puncture of the skin and bone fragments, and then a metal apparatus is assembled on them, which ensures the correct configuration of the bone.
- Other types of osteosynthesis.
The multidisciplinary CELT clinic employs experienced traumatologists and has modern equipment. Our specialists use the most advanced technologies to provide the most complete, effective and rapid treatment of various bone injuries. Our trauma department performs complex surgical interventions.
Technology of x-ray of ribs
Usually a chest x-ray
performed in frontal and lateral projections. This allows you to fully assess the overall picture of the condition of the ribs and spine. If necessary, targeted radiography of the area of the pathology is performed.
Before shooting, the patient stands facing the X-ray machine and presses his chest against its screen (the technique for performing such an X-ray is similar to the technique for traditional fluorography), takes a deep breath and then holds his breath. Thanks to a deep breath, the rib spaces expand - the contours of the ribs in the pictures become clearer.
Symptoms
All types of bone fractures have certain general symptoms:
- Pain. During the injury, it is strong and sharp, and after that it becomes dull. Increased pain with axial load.
- Deformation. If the fragments move relative to each other, then the leg or arm takes on an unnatural shape.
- Swelling. It begins to increase immediately after the injury.
- Subcutaneous hemorrhage - hematoma. Sharp bone fragments damage small blood vessels, and blood flows from them under the skin.
- Impaired function. If you ask the victim to move the injured leg or arm, this will not be possible due to severe pain, muscle strain and ligament damage.
The most dangerous are fractures of the skull, vertebrae, ribs, and pelvic bones. They can cause damage to internal organs and the nervous system. Multiple fractures are also dangerous; they can lead to shock.
How to prepare for a chest CT scan
There is no need for special preparation for a CT scan unless administration of a contrast agent is prescribed. About an hour before its administration, you need to have a light snack to avoid possible reactions: nausea, dizziness, drooling.
If the patient is diagnosed with diabetes mellitus and takes special medications, consultation with an endocrinologist is necessary and refusal to take pills for 48 hours before the procedure.
During lactation, you should stock up on breast milk for two feedings ahead.
Decoding the results
The interpretation of the x-ray results begins immediately after it is performed. In this case, no specific diagnoses are made, but simply all the features visualized in the images are described. First, the clarity of the resulting image and its contrast are assessed. Then an analysis of specific indicators is performed:
- symmetry of the structures of the chest and rib bones;
- bone integrity;
- structure of the roots of the lungs;
- structure and density of rib bones.
Normal indicators
In a healthy person, on an x-ray, the ribs have clear contours and a uniform structure. There are no shadows on the white areas of the bones. The ribs are located symmetrically to each other. The spine is not curved.
How is a chest CT scan performed?
Usually, a preliminary appointment is sufficient for diagnosis, but in emergency cases it is done on the day of treatment. Modern computed tomography machines can take pictures of fairly large areas of the body in a few seconds. This is very convenient for examining children and patients with severe pain and the inability to remain motionless for a long time.
The patient is positioned on a special table. It is secured with pads and straps to reduce mobility because movement blurs the image in the photograph. Then the table is sent inside the tomograph. Within a minute, the machine scans with X-rays and returns the patient to the office.
The radiologist is in the next room all this time and watches what is happening through thick glass. You can contact him at any time by clicking the contact staff button. The procedure does not bring any unpleasant sensations, and you can protect yourself from noise inside the tomograph with headphones or earplugs.
When diagnosing malignant neoplasms, a contrast agent is administered intravenously. Before this, the level of creatinine in the blood must be measured. The contrast agent helps determine the severity of the pathology and lesions.
Sensors transmit cross-sectional images to a computer screen. Pictures can be obtained both on removable media and in printed form.
CT scans of the ribs and chest are prescribed to children only for health reasons and in special diagnostic centers in pediatric departments.
Posterior ankle fracture.
Most often occurs in combination with a fracture of the lateral malleolus or as part of a trimalleolar fracture. Surgical treatment is indicated when more than 25% of the area of the supporting plateau of the tibia is involved, and displacement is more than 2 mm. Most often, fixation with screws is used; if the displacement can be eliminated closed, the screws are installed from front to back; if open reduction is performed from the paraachilles approach, then the screws are installed from the back to the front; it is also possible to use an anti-slip plate installed proximally.
Bimalleolar fracture.
This group includes both a fracture of the outer and inner ankles and a functionally bimalleolar fracture - a fracture of the outer malleolus and a rupture of the deltoid ligament. In most cases, surgical treatment is indicated. A combination of neutralizing, bridging, anti-slip plates, and compression screws is often used.

Osteosynthesis of a fracture of the outer malleolus using a compression screw and a neutralizing plate installed on the outer surface of the fibula, osteosynthesis of a fracture of the inner malleolus with two compression screws.
If the distal tibiofibular syndesmosis is damaged, which often occurs with suprasyndesmotic (high) fractures of the fibula, installation of a positioning screw is indicated for a period of 8-12 weeks with the complete exclusion of axial load.
When treating a functional bimalleolar fracture, there is no need to suture the deltoid ligament if it does not interfere with reduction, that is, if the position of the talus is satisfactory. When it is tucked into the joint cavity, it is impossible to eliminate the subluxation closed; for this reason, access to the inner ankle is performed, removal of the joint block and suture of the deltoid ligament.
Causes
For a bone to break, one of the following must be present:
- A strong blow from any object. In the place where it landed, the bone may break.
- A fall. Often it occurs from a height. But sometimes, in order to break something, it is enough to fall from your own height.
- Severe compression of the bone. For example, fragments of various collapsed massive structures.
- Excessive violent movement. For example, a helical fracture of the tibia often occurs when the leg turns, such as while skating.
Diagnostics
Diagnosis of the chest is carried out to distinguish a fracture from a bruise. A traumatologist deals with this issue. To make an accurate diagnosis, the following methods are used:
- Visual examination of the victim using tapping and listening to the chest. The doctor tries to determine whether there are accumulations of air, blood and other fluid in the lungs and pleural area.
- X-ray.
- Computed tomography or ultrasound diagnostics.
Classification of rib fractures
Impacts on human ribs are divided into indirect and direct. With indirect impact, the chest is compressed, so the ribs break on either side of the compression site. As a rule, several ribs break at once. In the case of direct impact, rib fragments can damage various internal organs, the lung when the ribs bend inward. There are bilateral fractures, as a result of which the chest loses the necessary stability, and a dangerous violation of pulmonary ventilation occurs. So-called fenestrated fractures also occur, i.e. fractures in two places on one side. Most often, rib fractures occur in people over 40 years of age. This is due to changes in bone tissue that occur in the human body due to age. In childhood, rib fractures are extremely rare, since the child's chest has great elasticity. There is also the following division of rib fractures: rib crack, bone fracture (so-called subperiosteal fracture) and complete rib fracture. The latter most often occurs at the site of the bend of the ribs. All these cases are characterized by the same symptoms of a fracture.
Signs of a fracture
There are relative and absolute signs of a fracture. Among the relative ones are the following:
- Hematomas due to internal hemorrhage due to vascular injury. There is swelling and a large hematoma in the fracture area, touching which causes acute pain.
- Cutting and unbearable pain in the affected area. In rare cases, people lose consciousness from painful shock.
- Inability to move a limb (complete loss of motor function).
- Swelling of the soft tissues indicates a fracture or dislocation.
Absolute signs of a fracture:
- With open fractures, fragments are clearly visible, and with closed fractures, bone curvature and an unnatural position are detected (there is no rupture of soft tissues).
- The appearance of clicks and crunches, as well as excessive mobility in the affected area.
- Loss of motor function (a person cannot move a limb and experiences severe pain). Often the symptoms resemble a severe bruise or dislocation, so differential diagnosis is required.
Spinal fracture - symptoms and treatment
All patients who are admitted to the hospital with high-energy trauma (after an accident, a fall from a height, etc.) should be regarded and treated as patients with spinal injury until the absence of spinal injury at all levels is confirmed [11].
Diagnostic stages:
- Interviewing a victim or witness to an incident.
- Examination and palpation (palpation) of the patient.
- Determination of the patient's neurological status.
- Instrumental diagnostics.
For a full diagnosis, the hospital must be equipped with a 24-hour spiral computer and high-field magnetic resonance imaging scanner.
Questioning and inspection
It is necessary to clarify when and under what circumstances the injury occurred. Ask if there is pain, motor or sensory disturbances. This will help understand the nature of the damage.
To detect a spinal fracture, the doctor conducts a visual examination of the patient, assesses the condition of the back muscles, the nature of the physiological bends, the peculiarities of the position of the spinous processes and the patient’s sensations when palpating them.
The doctor also conducts special tests, for example, asking the patient to raise his straight legs while lying on his back, lightly pressing or tapping the heels. The occurrence or intensification of pain in this case may indicate damage to the spine. These tests can only be performed by a doctor; doing them yourself is dangerous!
Determination of neurological status
When assessing the neurological status of patients with spinal injuries, it is advisable to use the ASIA/ISCSCI scale (American Spine Injury Association / International Standards for Neurological and Functional Classification of Spinal Cord Injury). This is the international standard for assessing spinal cord injuries based on clinical presentation. The following criteria for the condition of the spinal cord are used: muscle strength, tactile and pain sensitivity, reflex activity in the anogenital zone. Motor functions are assessed by testing the strength of 10 control muscle groups assigned to spinal cord segments.
Based on the neurological status, it is possible to determine how much the spinal cord is injured as a result of a spinal fracture. Spinal cord injury can be complete or incomplete:
- Complete damage can be anatomical, such as a rupture of the spinal cord, or functional. With functional damage, there is no rupture, but due to severe compression or contusion, there is no brain function in the area of injury; this condition is called spinal shock. It can last from 3 to 30 days.
- Incomplete injuries include concussion of the spinal cord and contusion. With a concussion, mild neurological disorders appear. They usually disappear within the first 3–7 days and are not accompanied by morphological changes in the spinal cord and its roots. When a bruise occurs, the substance of the brain is completely or partially destroyed. In this case, hemorrhages, areas of ischemia (insufficient blood supply), necrosis (death) and regional edema occur. Neurological disorders in this case persist for more than 7 days.
Incomplete spinal cord injuries can be accompanied by various clinical syndromes:
- Centromedullary syndrome is a violation of motor functions in the hands, up to complete paralysis. The muscle strength of the legs is also reduced, but not so much; most often the person can walk. This syndrome occurs when the spinal cord is damaged in the cervical region.
- Anterior medullary syndrome is a disorder of motor functions, pain and temperature sensitivity with preservation of proprioceptive sensitivity (the sense of one’s own movement and body position).
- Brown-Séquard syndrome is a disorder of motor functions and proprioceptive sensitivity on the side of the injury and loss of pain and temperature sensitivity on the opposite side. This half-damage injury to the spinal cord is common with stab wounds and tumors.
- Conus and cauda equina syndrome - weakness in the leg muscles, impaired urination and defecation due to decreased tone of the urinary and anal sphincters.
In case of spinal cord injury (SCI), it is important to distinguish compression of the spinal cord, its great vessels and roots from other types of injuries that are treated without surgery. Therefore, in every patient with PSCI, compression of the brain should be suspected until it is excluded by instrumental studies.
Instrumental diagnostics
For spinal fractures, the following may be performed: spondylography (x-ray of the spine), spiral computed tomography (SCT), CT myelography and magnetic resonance imaging (MRI).
Radiography . It is mandatory if it is not possible to perform SCT. Pictures are taken in two projections, which allows you to assess the condition of the vertebrae. Using radiography, you can detect changes in the axis of the spine, disruption of contours, displacement and dislocation of the vertebrae, deformation of their bodies and other elements. However, radiography of the spine does not allow choosing the optimal treatment tactics, since the extent of damage and characteristics of the fracture are not always visible on the x-ray.

Spiral computed tomography (SCT). Using SCT, you can more accurately assess a fracture: determine its level, the number of damaged vertebrae, identify arch fractures, etc. SCT also allows you to see displaced bone fragments that are not visible on x-rays.
CT myelography. Helps determine the location and extent of compression of the spinal cord, the patency of the space between the dura mater and the arachnoid mater, the size of the spinal cord and spinal canal.
Magnetic resonance imaging (MRI). It is carried out if after all the studies there are still doubts about the diagnosis, as well as if damage to the intervertebral discs is suspected.
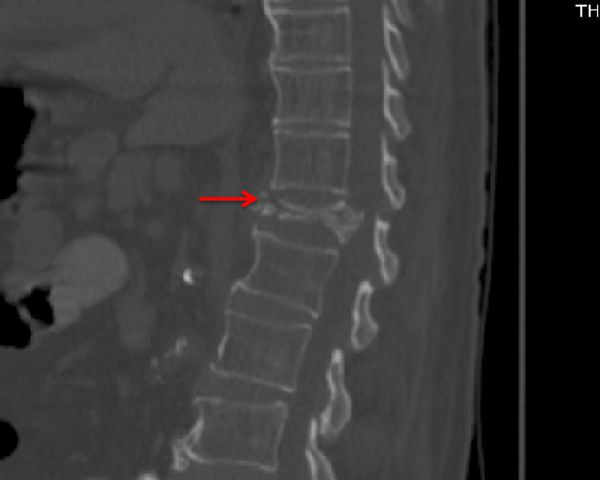
It is not always necessary to perform all of the listed studies. The most optimal methods are SCT and MRI. They allow a correct diagnosis to be made in 95–98% of patients. In intensive care units, radiography of the spine is uninformative in 80–90% of patients, so it is advisable to immediately conduct a spiral CT scan of all parts of the spine, and if a combined injury is suspected, a SCT scan of the whole body.
Densitometry. It is performed in elderly patients, as well as in cases of suspected osteoporosis [1]. A special device uses X-rays and ultrasound to determine bone density, calcium levels and the thickness of the surface layer of bones. After this, it compares the obtained data with normal values.

Fracture of the outer ankle.
Conservative treatment, as indicated above, is indicated in the absence of displacement of the talus (that is, with intact internal stabilizers of the ankle joint), and less than 3 mm of displacement of the lateral malleolus itself. The classical point of view that the width of the joint space along the internal surface of more than 5 mm indicates a rupture of the internal stabilizers has recently been revised. This is due to the fact that biomechanical studies on cadavers have shown that displacement of the talus up to 8-10 mm is possible with a simulated fracture of the lateral malleolus and an intact deltoid ligament. For this reason, there is a need to confirm deltoid ligament rupture using ultrasound or MRI.
Surgical treatment for isolated fractures of the lateral malleolus is most often performed using plates. There are two main methods for installing plates - on the outside and on the back surface. When installing the plate on the outer surface, it is possible to use a compression screw and a neutralizing plate
Osteosynthesis of a fracture of the lateral malleolus using a compression screw and a neutralizing plate installed on the outer surface of the fibula.
or using a locking plate as a bridge retainer.
Osteosynthesis of a fracture of the lateral malleolus using a plate installed on the outer surface of the fibula according to the principle of bridge-like fixation, with additional fixation of the distal tibiofibular syndesmosis with two screws.
When installing a plate on the posterior surface of the fibula, it can be used as an anti-slip plate,
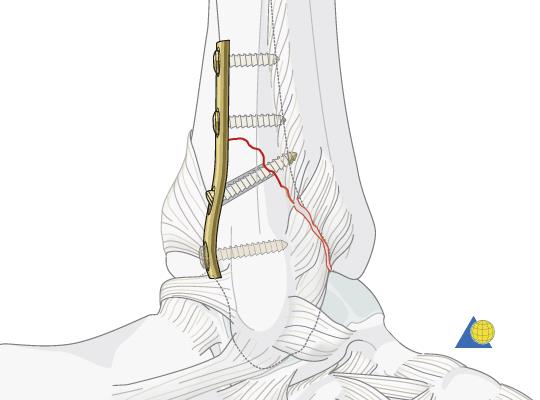
Osteosynthesis of a fracture of the lateral malleolus using a plate installed on the posterior surface of the fibula according to the principle of compression and anti-slip.
Or as a neutralizing plate when using a compression screw. The posterior position of the plate is more justified from a biomechanical point of view, but a common complication is irritation of the peroneal tendons, which can lead to long-term pain.
Alternative options include isolated fracture fixation with multiple compression screws, intramedullary nails, or TENs, but these are less common in surgical practice.
After open reduction and external osteosynthesis, 4-6 weeks of immobilization in a cast or orthosis follow; the duration of immobilization is twice as long in the group of diabetic patients.