After undergoing an abdominal ultrasound, the sonologist will issue a research protocol containing numbers and characteristics for various organs - objective information based on reflected ultrasound data.
Also, the ultrasound diagnostician will make his own conclusion based on these results, where he will decipher the picture that he saw, based on his own knowledge and experience. But the final decision on making a diagnosis and interpreting the results of the study is made by the doctor - the specialist who referred the patient for examination.
As a rule, in addition to the ultrasound results, it takes into account the patient’s complaints, the results of a direct examination, the results of laboratory diagnostics and other factors.
Without in any way assuming the possibility of making an independent diagnosis based on the results of an abdominal ultrasound, we will still give a general idea of what data the research protocol contains.
Let us remind you that in order for the results of an abdominal ultrasound to be reliable, special preparation is required before the examination. Intestinal spasms, gas overload, and X-ray contrast agent residues can lead to incorrect data or the impossibility of obtaining it. Excess weight, which impedes the penetration of ultrasound, a significant wound in the area where the sensor is placed, and even simply increased physical activity during diagnostics can also distort the results.
What will be written in the research protocol?
Liver
- The size of the organ as a whole (normal, can be increased or decreased) and the size of the lobes (right, left, caudate). It is interesting that data on normal liver sizes vary in different medical literature; they are individual and depend on many factors.
- Contours – smooth or not.
- The capsule is normally differentiated and not thickened.
- The echostructure of the parenchyma is normal, increased, decreased.
- Focal formations are not normal.
- The vascular pattern is normally normal, but can be enhanced or depleted.
- The dimensions of the veins - portal, inferior vena cava and hepatic veins of the first order - in millimeters.
Using these data, the doctor can diagnose abscesses, hepatitis, hepatosis, fatty changes in the organ, tumors including metastases, “stagnation” due to cardiopulmonary diseases.
Ultrasonography of the abdominal organs
Ultrasound scanner WS80
An ideal tool for prenatal research.
Unique image quality and a full range of diagnostic programs for an expert assessment of a woman’s health.
- Research methodology
- Liver
- Gallbladder and bile ducts
- Pancreas
- Spleen
- Esophagus, stomach, intestines
- Kidneys and bladder
- Abdominal vessels
Research methodology
An ultrasound scan of the abdominal organs is performed in the morning on an empty stomach after an overnight fast, but in emergency situations the study can be performed at any time. In most cases, no special preparation is required, although in obese patients or patients with severe flatulence, a qualitative examination may be difficult. To reduce interference caused by the presence of gas in the intestines, it is recommended to follow a diet low in fiber for 2-3 days, eliminating foods that increase gas formation in the intestines. In addition, the use of carbolene and enzyme preparations (festal, digestal) is indicated. There is no need to give a cleansing enema. When examining urgently, as well as after eating, it is necessary to remember the possibility of detecting additional inclusions in the stomach or intestines due to the presence of contents in their lumen.
Echography is carried out with the patient lying on his back, left and right side, sitting or standing, and it is advisable to adhere to the following sequence: the examination begins from the upper abdomen using longitudinal sections. The transducer is placed in the epigastrium along the midline. In this position, the left lobe of the liver and behind it the abdominal aorta are visualized. The transducer is then moved to the left, examining the remainder of the left lobe. After this, the sensor is sequentially moved in the opposite direction, along the right hypochondrium to the anterior axillary line. In this case, the transition of the left lobe to the right, the area of the round ligament of the liver, the caudate and quadrate lobes, the inferior vena cava, the right lobe of the liver, liver veins, portal vein, gall bladder, and right kidney are visualized. Then longitudinal sections are repeated, moving the sensor again to the left to the midline. After this, scanning is carried out in the transverse plane: the transducer is installed at the level of the xiphoid process and successive sections are made, moving it to the navel and back. In this case, the left lobe of the liver, stomach, pancreas, aorta, inferior vena cava, celiac trunk, superior mesenteric artery, and splenic vein are visualized.
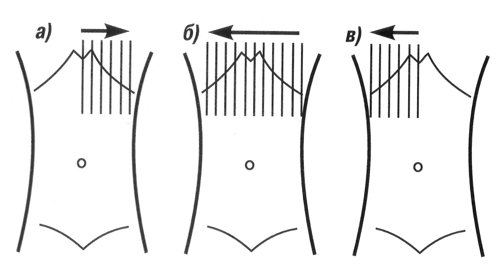
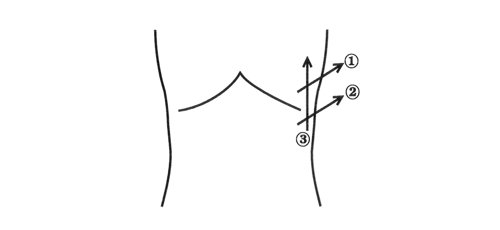
Scheme 1. Algorithm for conducting an ultrasound examination of the abdominal organs (longitudinal scanning): a) - scanning from the midline of the abdomen to the left; b) — scanning from the left anterior axillary line to the right anterior axillary line; c) - scanning from the right anterior axillary to the midline.
The study is carried out without holding your breath. As a result of scanning in 2 planes, a general idea of the topography of the organs of the upper floor of the abdominal cavity is obtained and gross deviations from the norm are identified (schemes 1, 2).
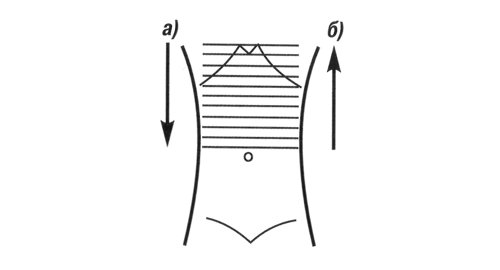
Scheme 2.
Algorithm for conducting an ultrasound examination of the abdominal organs (transverse scanning): a) - scanning from the xiphoid process to the navel; b) - scanning from the navel in the cranial direction.
Then they begin a detailed study of the organs while holding their breath at the height of a deep breath. When examining the liver and gall bladder, the transducer is installed parallel to the right costal arch and its slight inclinations, viewing the entire liver and gall bladder. In case of severe flatulence, it is possible to conduct a study through the intercostal spaces on the right with the patient positioned on the left side, which will avoid interference caused by swollen loops of intestines. Echography of the pancreas begins with transverse sections, subsequently moving to scanning in the longitudinal plane. The spleen is examined with the patient in the right lateral position, placing the transducer perpendicular to the costal arch.
To examine the gastrointestinal tract, first longitudinal sections are made across the entire abdomen from left to right and back, then transverse from top to bottom and back. Both the stomach and intestines should be examined in the transverse and longitudinal planes.
Ultrasound examination of the kidneys is carried out both from the back (transverse and longitudinal sections), and from the front (lying on the back) and lateral (lying on the right and left side) surfaces of the abdomen, preferably while holding the breath during the deep inspiration phase. To detect mobility or prolapse of the kidneys, echography is performed with the patient sitting or standing.
The proposed algorithm for conducting an ultrasound examination of the abdominal organs and kidneys must be followed in all cases, since only a systematic analysis of the resulting echograms allows for a full examination, avoiding possible errors, and obtaining the necessary information. It should be remembered that the quality of the examination, first of all, depends on the attention of the doctor, and a hasty examination is unacceptable.
Liver
An ultrasound examination of the liver can be performed at any time without prior preparation. The examination is carried out, as a rule, in three planes (longitudinal, transverse and oblique) from the right hypochondrium and epigastrium. In this case, it is necessary to evaluate the location, shape, contours, size, structure and echogenicity of the parenchyma, the vascular pattern in general and specific vessels, the ductal system, the influence of surrounding organs on the state of the liver image. The accuracy of diagnosing detected changes increases with dynamic observation (Scheme 3).
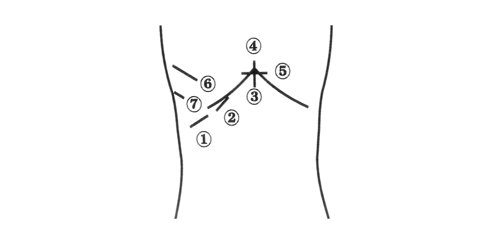
Scheme 3.
Sensor positions when scanning the liver: 1-3 - subcostal scanning 4 - longitudinal scanning 5 - transverse scanning 6-7 - intercostal scanning.
Normally, most of the liver is located to the right of the spine, and the smaller part is to the left of it and reaches the left parasternal line. The contours of the liver are smooth, it has a clear outline, the capsule is clearly visible in the form of a hyperechoic structure surrounding its parenchyma (with the exception of areas adjacent to the diaphragm, where the capsule is not differentiated from the latter). Normally, the lower edge of the liver does not protrude from under the costal arch. It is generally accepted to measure the oblique vertical size of the right lobe (does not exceed 13-15 cm) and the thickness of the left lobe (up to 5 cm). The structure of the unchanged liver is represented by a fine-grained image, consisting of many small point and linear structures, evenly distributed over the entire area of the resulting section. The echogenicity of the normal liver parenchyma is comparable to or slightly higher than the echogenicity of the renal cortex (in the absence of pathology). Sonography allows you to differentiate the various tubular structures located in the liver.
A distinctive feature of the hepatic veins is their radial arrangement (from the periphery to the walls, the ability to trace the course of small branches (up to 1 mm in diameter) to the periphery of the organ. The portal vein is formed as a result of the merger of the superior mesenteric and splenic veins. It is best seen with oblique scanning through the right hypochondrium and is visualized as a tubular structure with clear walls. It can be traced from the place of formation to the confluence with the portal of the liver, where it is divided into left and right branches. Normally, the diameter of the portal vein does not exceed 13-15 mm. The hepatic artery is visualized in the area of the porta hepatis as a tubular structure of small diameter (up to 4-6 mm) with highly echogenic walls. Intrahepatic bile ducts can normally be visualized only starting with the lobar ones. They also have highly echogenic walls and a small diameter (no more than 1 mm).
Research results
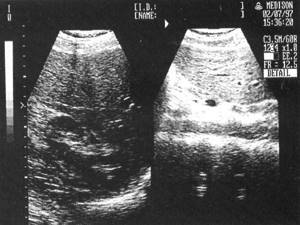
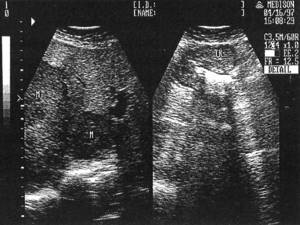
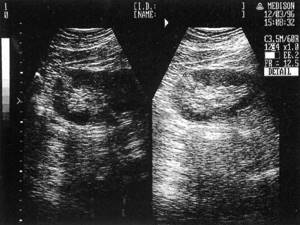
Rice. 1.
Sonographic picture of normal left and right lobes of the liver.

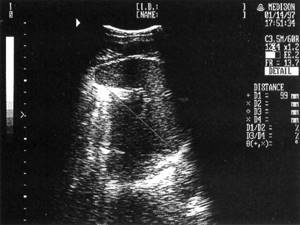
Rice. 2.
One of the options for an echogram of normal liver parenchyma.

Rice. 3.
Sonographic picture of the lobar hepatic duct.

Rice. 4.
Echogram of the right lobe of the liver with its enlargement: Liver - liver, Kidney - kidney.

Rice. 5.
The echographic picture of fatty infiltration of the liver is an increase in the echogenicity of the parenchyma with a weakening effect in the deep parts of the liver.

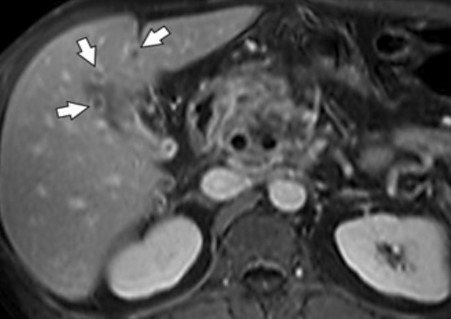
Rice. 6.
Sonographic picture of a focal form of fatty infiltration (marked with arrows).
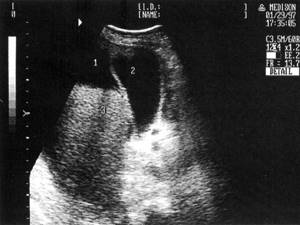
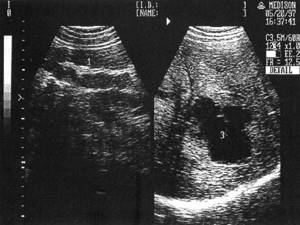
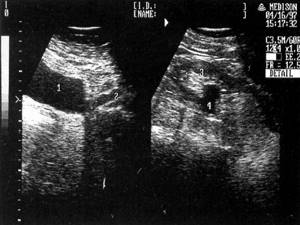
Rice. 7.
An echographic picture of one of the variants of decompensated cirrhosis of the liver: 1 - ascites, 2 - gall bladder, 3 - liver.

Rice. 8.
Sonographic picture of porto-caval anastomoses at the porta hepatis: 1 - liver, 2 - gallbladder, 3 - porto-caval anastomoses, 4 - liver cyst.

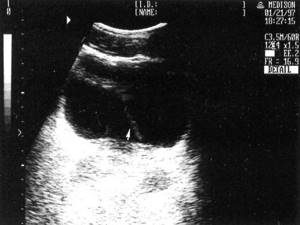
Rice. 9.
An echographic picture of one of the options for depicting a capillary hemangioma of the left lobe of the liver.

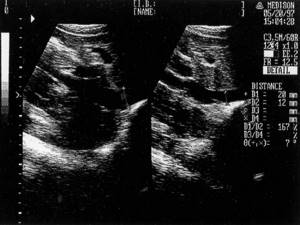
Rice. 10.
Sonographic picture of a simple salitary cyst of the right lobe of the liver (marked with markers).

Rice. eleven.
Sonographic picture of polycystic liver disease.

Rice. 12.
Sonographic picture of fine calcification of the liver (marked with an arrow).

Rice. 13.
Sonographic picture of multiple metastatic liver lesions: M - metastases.
Gallbladder and bile ducts
Echography of the gallbladder and bile ducts must be carried out on an empty stomach, no earlier than 8-12 hours after eating. This is necessary to sufficiently fill the bladder with bile. The patient is examined in three positions - on the back, on the left side, standing, at the height of a deep breath. Normally, the gallbladder is located on the dorsal surface of the liver; it has a fundus, a body and a neck, which passes into the cystic duct. During longitudinal scanning, the gallbladder is located as an echo-negative oval, elongated or pear-shaped formation, 4 to 9.5 cm long, up to 3-3.5 cm wide, with thin (up to 1.5-2 mm) walls. Normally, the contents of the bladder are uniform and homogeneous (Scheme 4).
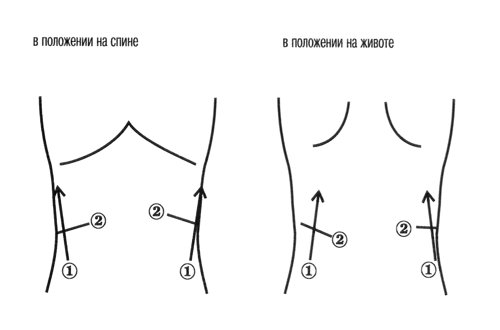
Scheme 4.
The position of the sensor when scanning the gallbladder. 1.3 - in the supine position; 2.4 - in a position on the left side.
The intrahepatic bile ducts run parallel to the branches of the portal vein, located ventral to them. Small bile ducts (normally practically invisible) join into larger ones in the direction of the hepatic hilum, forming the right and left hepatic ducts, which merge at the hepatic hilum into the common hepatic duct (normally its diameter does not exceed 4-5 mm).
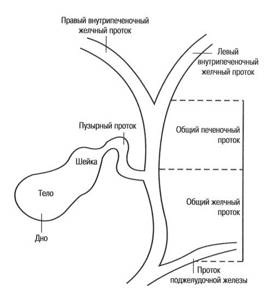
Scheme 5.
Anatomy of the gallbladder and bile ducts.
The latter, connecting with the cystic duct, forms the common bile duct (normally its diameter does not exceed 7 mm), which opens into the duodenum. The ducts have smooth, clear walls, the lumen is free of echo signals (Diagram 5).
Research results

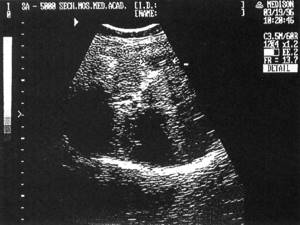
Rice. 14.
Sonographic picture of a normal gallbladder.

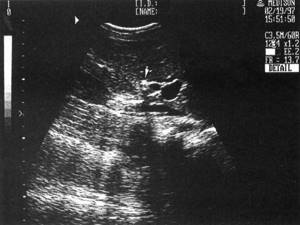
Rice. 15.
Sonographic picture of a deformed gallbladder.

Rice. 16.
Sonographic picture of gall bladder cholesterosis (cholesterol polyps are marked with arrows).

Rice. 17.
An echographic picture of putty-like bile in the cavity of the gallbladder, reminiscent of a solid formation (marked by an arrow).

Rice. 18.
The echographic picture of one of the variants of cholelithiasis is multiple small (1-2 mm) floating stones in the cavity of the gallbladder.

Rice. 19.
An echographic picture of one of the variants of cholelithiasis (two “soft” cholesterol stones are marked with arrows).

Rice. 20.
The echographic picture of one of the variants of cholelithiasis is a calculus measuring 1.9 cm, giving behind an acoustic shadow.

Rice. 21.
The echographic picture of one of the variants of cholelithiasis is a disabled gallbladder. In the area of the projection of the gallbladder, a conglomerate of dense echo structures is visualized (marked with an arrow), giving behind an acoustic shadow.

Rice. 22.
An echographic picture of one of the variants of the image of the gallbladder during exacerbation of chronic cholecystitis (thickening and layering of the wall).

Rice. 23.
One of the variants of the complicated course of the postoperative period is infiltration (circled with the cursor) in the area of the gallbladder bed after its removal.
Rice. 24.
One of the possible complications of cholecystectomy is that a small calculus is visualized in the stump of the gallbladder (marked by arrows), giving an acoustic shadow.
Rice. 25.
An echographic picture of choledocholithiasis (a stone giving an acoustic shadow is marked with an arrow).

Rice. 26.
Sonographic picture of the dilated common bile duct (diameter 21 mm) after cholecystectomy: 1 - common bile duct, 2 - stomach, 3 - dilated duct of Wirsung, 4 - portal vein, 5 - superior mesenteric artery, 6 - aorta.
Pancreas
Sonography of the pancreas is performed at the height of forced inspiration or with an inflated abdomen, when the left lobe of the liver significantly descends into the abdominal cavity, providing a good environment for ultrasound. In some cases, for better visualization of the gland, the patient can be recommended to drink 300-500 ml of warm degassed water in small sips, thereby creating an acoustic window.
When examining the pancreas, first a transverse and then a longitudinal scan is performed. Transverse scanning is carried out at approximately an angle of 10-20° along a conventional line drawn from the hilum of the right kidney to the hilum of the spleen or the upper pole of the left kidney, by sequentially shifting the transducer from the xiphoid process towards the navel. Longitudinal scanning is performed by sequentially moving the sensor from the right midclavicular line to the left anterior axillary line. The main anatomical landmarks for identifying the pancreas: the splenic vein, located under the lower edge of the gland, the superior mesenteric artery - a rounded anechoic formation below the vein, and even lower and to the left - a rounded anechoic formation - the aorta, and to the right and below - an anechoic oval formation - the inferior hollow vein (diagram 6).
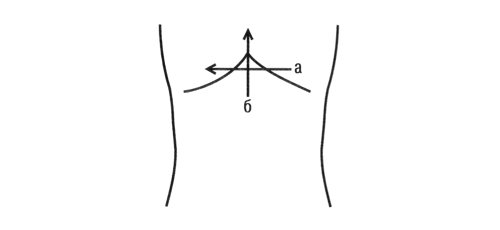
Scheme 6.
Sensor positions when scanning the pancreas: a) - transverse scanning; b) - longitudinal scanning.
In terms of its echogenicity, the pancreas either approaches the internal structure of the liver or slightly exceeds it. The parenchyma of the gland is in most cases homogeneous, but in some cases it can be fine-grained. With age and in obese people, the echogenicity of the gland gradually increases. Determining the size of the gland is of paramount importance for diagnosing its various diseases. Thickness, i.e. the anteroposterior size of the head is 2.5-3.0 cm, the body -1.5-1.7 cm and the tail up to 2.0 cm. Normally, the Wirsung duct can also be visualized; its diameter in the body of the gland in healthy individuals does not exceed 1 mm, and in the head - 2 mm.
Research results

Rice. 27.
One of the options for an echographic image of the anatomy and topography of a normal pancreas: 1 - liver, 2 - head, 3 - body, 4 - tail of the gland, 5 - portal vein, 6 - splenic vein, 7 - superior mesenteric artery, 8 - inferior vena cava , 9 - aorta.

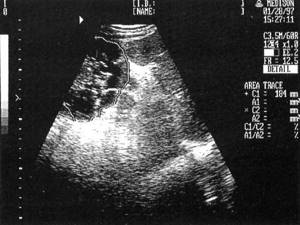
Rice. 28.
Sonographic picture of a pancreatic pseudocyst: 1 - liver, 2 - stomach, 3 - cyst.

Rice. 29.
Sonographic picture of a pancreatic tumor: Hepar - liver, Pancreas - pancreas, Tumor - tumor, Vp - portal vein, AMS - superior mesenteric artery, Aorta - aorta.
Spleen
It is better to perform echography of the spleen at a depth of high inspiration with the patient positioned on the right side. Its outer surface is slightly convex, the inner one is slightly concave, and it has the shape of a crescent, the long axis of which is directed from top to bottom and forward. Sometimes the spleen is covered by the lungs and is not visualized. In this case, a study is proposed through the intercostal spaces on the left, in which the resulting ultrasound image is similar to the image of the organ along the long axis. On the inner surface of the spleen, its gate is visualized - the place where arteries and veins enter the parenchyma. The spleen parenchyma has the appearance of a homogeneous formation with a fine-grained internal structure, its echogenicity is significantly lower than that of the liver and slightly higher than that of the kidney parenchyma. Normally, the length of the spleen does not exceed 11-12 cm, thickness - 4-5 cm, area - 50 sq.cm. The diameter of the splenic vein in the hilum area is 5-7 mm (Diagram 7).
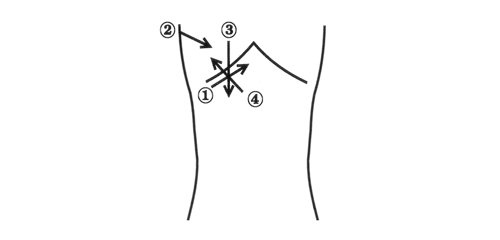
Scheme 7.
Sensor position when scanning the spleen: 1-2 - transverse scanning; 3 - longitudinal scanning.
Research results
Rice. thirty.
Sonographic picture of a normal spleen.

Rice. 31.
Sonographic picture of the accessory spleen.

Rice. 32.
Sonographic picture of an enlarged spleen (1) due to cirrhosis of the liver, dilated splenic (2) and gastric (3) veins.

Rice. 33.
Sonographic picture of a splenic cyst: C - spleen, K - cyst, S.V. - splenic vein.

Rice. 34.
Sonographic picture of splenic infarction (marked with an arrow).
Esophagus, stomach, intestines
Echography of the esophagus and stomach is carried out on an empty stomach, and it is better to do the intestines after defecation. The position of the patient can be different and is chosen taking into account the possible localization of the pathological process and its best visualization. On a sagittal section passing through the esophageal opening of the diaphragm (the transedducer is installed in the epigastrium under the xiphoid process), the normal esophagus is located as a tubular structure formed by two anechoic stripes corresponding to the anterior and posterior walls of the esophagus, and a hyperechoic central zone enclosed between them, corresponding to its mucous membrane. The diameter of the esophagus is measured from its anterior to posterior wall (external-external dimension) along a plane perpendicular to the axis of the esophagus, and does not normally exceed 10.5 mm. The length of the abdominal esophagus is 15-20 mm in healthy individuals.
Ultrasound examination of the stomach is carried out in the epigastrium in longitudinal and cross sections. The thickness of the stomach wall is normally 3-7 mm, in some cases it is possible to visualize 5 layers of its wall (the first is echogenic, corresponding to the mucosa; the second is anechoic - the muscular plate of the mucosa; the third is echogenic - submucosal; the fourth - anechoic - muscular and the fifth - echogenic - serous membranes) and trace peristaltic contractions.
The echographic picture of the small and large intestines is largely similar; the wall thickness of both is normally 2-5 mm, depending on peristalsis and the degree of distension. The main ultrasound sign of damage to the stomach or intestines is thickening of their walls, the appearance of the so-called pseudokidney symptom (damage to a hollow organ).
Research results

Rice. 35.
Sonographic picture of the unchanged abdominal esophagus: 1 - liver, 2 - abdominal esophagus, 3 - heart, 4 - diaphragm.
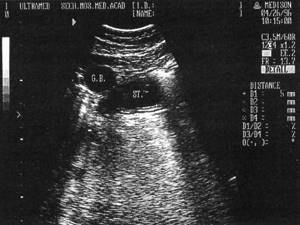
Rice. 36.
Sonographic picture of hypersection of the stomach, 5 layers of the wall are visible: St. - stomach, GB - gallbladder.
Rice. 37.
An echographic picture of one of the variants of the body of the stomach and metastatic lesions of the liver: 1 - the stomach wall thickened to 17 mm, 2 - liver, 3 - metastasis.
Rice. 38.
Sonographic picture of colon cancer and metastatic liver damage: M - metastases, TK - thickened intestinal wall.
Kidneys and bladder
Since the upper segment of the kidneys is covered by the ribs, to reduce the interference caused by them, echography is performed from the back (front and side surfaces of the abdomen) while holding the breath during the deep inspiration phase. If the kidneys are located high, as well as to determine their mobility, scanning is carried out with the patient in an upright position. To determine the position of the kidneys, a series of transverse scans are initially performed (from the back in a prone position), sequentially moving the transducer from the lower to the upper pole. Longitudinal scanning is carried out by moving the sensor from the outer surface of the kidneys to the inner. To get a more accurate idea of the condition of the parenchyma, the size of the pelvis and determine the vessels, the study is also carried out from the anterior surface of the abdomen. On longitudinal sections, the kidney is visualized as an elongated oval, and on transverse sections, an ovoid-shaped formation, clearly differentiated from the surrounding tissues. Normally, the length of the kidney is 7.5-12.0 cm, the width is 4.5-6.5 cm, and the difference in the length of both kidneys does not exceed 1.5-2.0 cm (Diagram 8).
Scheme 8.
Sensor position when scanning the kidneys: 1 - longitudinal scanning; 2 - transverse scanning.
The kidney parenchyma has a very delicate, almost anechoic internal structure. Between the kidney capsule and the pelvicalyceal system, especially in young and middle-aged people, one can see multiple almost round-shaped echo-negative formations, which are pyramids. The diameter of the pyramids ranges from 0.5 to 0.9 cm. The calyceal complex is detected as a formation of increased echogenicity located in the center of the kidney. Normally, the ratio of renal parenchyma to the alyceal complex is approximately 2:1.
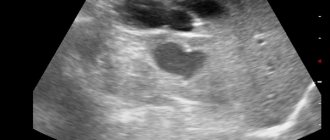
The bladder is examined from the anterior abdominal wall. A necessary condition is its good filling, since an empty bladder cannot be detected sonographically. Moreover, the more liquid in the bubble, the more reliable the results will be. Normally, an unchanged bladder is visualized on transverse sections as an echo-negative barrel-shaped formation, and on longitudinal sections as an echo-negative formation of an ovoid shape, clearly defined, with a flat and smooth surface, free from internal structures.
Research results
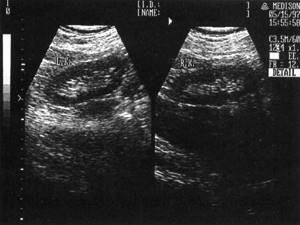
Rice. 39.
Sonographic picture of normal right (RK) and left (LK) kidneys.

Rice. 40.
Sonographic picture of a simple uncomplicated cyst (K) of the left kidney.
Rice. 41.
Sonographic picture of polycystic kidney disease (the left kidney is circled with a cursor).
Rice. 42.
Sonographic picture of the left and right kidneys with small angiomyolipomas in the parenchyma.

Rice. 43.
An echographic picture of a kidney with a calculus in the neck of the calyx with symptoms of its obstruction and hydrocalycosis (arrow).

Rice. 44.
Sonographic picture of a kidney with a stone in the pelvis: 1 - kidney, 2 - stone, 3 - acoustic shadow.

Rice. 45.
Sonographic picture of a kidney with a dilated pelvis (indicated by arrows).
Rice. 46.
Sonographic picture of the kidney with dilatation of the pelvis and proximal ureter: 1 - bladder, 2 - ureter, 3 - kidney, 4 - pelvis.
Rice. 47.
An echographic picture of a normal bladder (the release of a stream of urine from the mouth of the left ureter is indicated by an arrow).

Rice. 48.
Sonographic picture of a bladder diverticulum: 1 - bladder, 2 - diverticulum.
Abdominal vessels
Echography of the vessels of the abdominal cavity is carried out through the anterior abdominal wall at the height of a deep inspiration and during free breathing. Ultrasound examination makes it possible to easily locate most of the great vessels: aorta, celiac trunk, superior mesenteric, hepatic and splenic arteries, inferior vena cava, portal, splenic, superior mesenteric and right renal veins. Their visualization is important, since the great vessels are a kind of “road map”, the use of which allows you to determine the location of organs and other anatomical structures of the abdominal cavity, in some cases correctly assess the severity of the pathological process in the organ, as well as diagnose various injuries and vascular diseases.
On longitudinal scans, the abdominal aorta has the appearance of a pulsating tubular structure located slightly to the left or above the spine, somewhat tapering in the caudal direction, formed by two echo-positive linear structures with an echo-negative central zone. The normal diameter of the aorta is 2.0-2.5 cm. The inferior vena cava has the appearance of a similar tubular structure with clearly defined walls, located slightly to the right of the spine; the largest diameter, which changes with straining (!), does not normally exceed 2.5 cm .
Research results

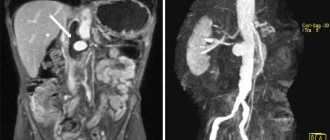
Rice. 49.
Sonographic picture of the longitudinal section of the aorta (1), superior mesenteric (2) and celiac (3) arteries.

Rice. 50.
Sonographic picture of the cross section of the aorta, celiac artery and its branches: 1 - aorta, 2 - celiac artery, 3 - hepatic artery, 4 - splenic artery, 5 - portal vein, 6 - inferior vena cava, 7 - spine.

Rice. 51.
Sonographic picture of the abdominal aorta in the bifurcation area (marked with an arrow).

Rice. 52.
Ultrasound picture of an abdominal aortic aneurysm: 1 — aortic lumen, 2 — thrombotic masses filling the aneurysm, 3 — recanalization site.
Rice. 53.
Sonographic picture of the inferior vena cava (on the left - with free breathing, on the right with straining).
All studies were carried out using a SonoAce-5000 ultrasound scanner (Medison, South Korea) equipped with a 3.5 MHz convex sensor.
Ultrasound scanner WS80
An ideal tool for prenatal research.
Unique image quality and a full range of diagnostic programs for an expert assessment of a woman’s health.
Gallbladder
The protocol will describe the shape (pear-shaped or cylindrical), size (length and width), volume of the organ, and thickness of its walls. Normally, there are no formations in the lumen. An acoustic shadow can be described in the presence of stones or tumors in the bladder, and the type of stones can be determined from it. The sonologist can note whether the formations are moving or motionless.
Using these data, a specialist can determine abnormalities in the development of the organ (septa, kinks), the presence of acute or chronic cholecystitis, empyema, and gallstone pathology.
Preparation for ultrasound examination
Ultrasound scanning of abdominal vessels requires special preparation.
Diet
The day before diagnosis, the patient needs to exclude the following foods from the diet: dairy and fermented milk, black bread, soda, sweets and flour, cabbage, legumes. In other words, it is not recommended to consume foods that contribute to excessive gas formation in the intestines.
Body cleansing (one day before the procedure)
A day before the procedure (or two days before, as recommended by the doctor), the patient needs to take 4-5 tablets of activated carbon 3 times a day. You can replace charcoal with any other carminative drug after consulting your doctor. If the patient's digestion is impaired, he is recommended to take the enzyme preparation after meals. The final meal is 5 hours before bedtime. The study is carried out on an empty stomach.
MRI of internal organs - indications and contraindications
Magnetic resonance imaging is unacceptable if the patient has:
- orthopedic structures made of metal (prosthetic joints), staples for fixing bones, etc.;
- vascular stents;
- functioning devices - cardio-, myo-, neurostimulator, drug delivery system, cochlear implant.

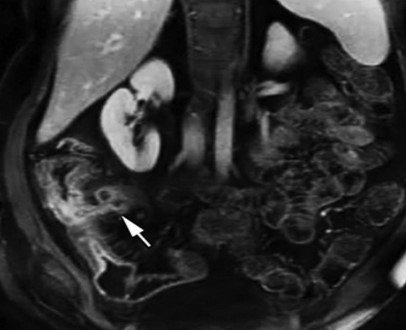
Renal vein thrombosis (arrow)
Relative contraindications:
- first trimester pregnancy;
- age up to 4 weeks;
- acute conditions requiring resuscitation measures;
- severe pain syndrome;
- neurological and psychiatric diseases accompanied by intrusive movements, lack of control over behavior: for claustrophobia, dementia, epilepsy, Parkinson's and Alzheimer's diseases, MRI of internal organs is done in a hospital setting after immersion in medicated sleep;
- obesity over 150 kg, abdominal circumference greater than the diameter of the tomograph ring.
MRI of internal organs with contrast enhancement is not suitable for patients with an allergic reaction to gadolinium, renal failure with high creatinine levels, implying hemodialysis.
The study will help clarify the cause of symptoms from the gastrointestinal tract:
- pain in the epigastrium, right or left hypochondrium, groin, periumbilical region: intensity - from dull, aching to acute, paroxysmal or constant, may be accompanied by a temperature reaction;
- brown urine;
- nausea, vomiting, unstable stool;
- yellowing of the skin, palms, sclera;
- visualization of blood, mucus, fat, undigested food in the stool;
From the kidneys:
- acute or dull pain in the lumbar region, with irradiation along the ureter;
- discharge of cloudy urine (in case of tumors, stone formation, glomerular diseases - with blood);
- fever with chills, etc.
Liver metastases (arrows)
From the reproductive and lower urinary system:
- discomfort in the perineum;
- dysuric disorders;
- acute urinary retention;
- sexual dysfunction;
- pain during sexual intercourse, changes in the quality of ejaculate, infertility, etc.
Magnetic resonance imaging of organs with contrast

To improve visualization, the study is performed with intensification
Native MRI has high soft tissue contrast. But in some cases (tumors, inflammatory processes, vascular malformations, pathologies of brain tissue), the diagnostic accuracy may be qualitatively different when using chelated gadolinium. In its pure form, rare earth metal is highly toxic, but in its transformed form it is practically safe. Adverse reactions - nausea, burning at the injection site, rash, headache - are recorded extremely rarely and are mild. The administration of contrast agents during pregnancy is not recommended, since the rate of clearance (purification coefficient) of the dye from the amniotic fluid is unknown.
Post-contrast MR image of the abdomen showing a fistulous tract between the distal ileum and the abscess (arrow)
Depending on the area of interest, the amplifier can enter the body:
- orally - in the form of a drink;
- intravenously - often into the ulnar vessel;
- transrectally - through the anus.
When examining the intestines, double contrast is used.
With the help of research you can:
- establish the stage of the disease in a previously identified tumor process: MRI of internal organs shows the degree of interaction of the malignant neoplasm with surrounding tissues;
- determine the scope of the operation, clarify the anatomical features of the structure;
- assess dynamic changes during treatment.
Doppler ultrasound indicators
When analyzing and interpreting the results of Doppler ultrasound of the abdominal vessels, the doctor takes into account the following indicators:
- vascular patency;
- diameter and features of the location of the lumen of the vessel;
- length of visibility of the changed lumen;
- speed of blood flow in arteries and veins.
If blood clots or atherosclerotic plaques are detected (which should not normally be present), the doctor must determine their exact location, analyze the structure and density.
How is MRI performed on human organs?

Preparing for magnetic resonance imaging
Algorithm of actions:
- Preparation. Choose a suitable clinic. The highest quality images are obtained when undergoing a diagnostic procedure on a tomograph with a force field strength of 1.5 Tesla. Low-power units can miss pathology located in hard-to-reach places.
- At the medical center. The patient arrives for the procedure with a small amount of time to complete paperwork. After instructions, it is necessary to deposit items with paramagnetic properties - telephone, keys, coins, etc.
During a planned intestinal examination with contrast, the patient is given a special solution to drink half an hour before the procedure.
- In the diagnostic room. The X-ray technician places the patient on the tomograph table and places the coil over the body. The nurse inserts a conductor into the vein and connects an automatic injector through which a paramagnetic agent will flow at a given time. After the initial examination, wait for the dye to spread throughout the body and continue scanning.
The medical staff monitors the progress of the diagnosis through a window from an adjacent room; the patient has a special button at hand to communicate with the doctor. Noise from operating equipment is reduced using headphones. Upon completion of the examination, the catheter is removed from the vein and a pressure bandage is applied.
CT or MRI of internal organs, which is better?
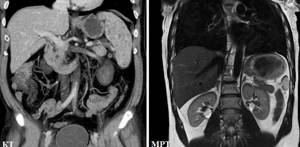
Sample pictures
Experts consider magnetic resonance imaging and computer scanning as complementary diagnostic methods. What is best should be decided by the attending physician, taking into account all available data.
The tumor process of a parenchymal organ, the degree of spread of the tumor is more accurately shown by MRI. In urological practice, CT is preferred for nephrocystolithiasis. Based on the study, the density of stones is determined, which is inaccessible to magnetic resonance imaging: hard stones practically do not contain water, and therefore are not visualized on images. Computer scanning is the diagnostic choice in urgent situations, when the speed of obtaining results is important to save life.
At the Magnit clinic in St. Petersburg, you can do MRI of the abdomen, retroperitoneum, pelvis and other areas using expert-class equipment from Siemens, Germany. A closed-circuit tomograph (field strength 1.5 Tesla) allows you to identify pathological changes in the body at the preclinical stage - in the absence of symptoms. In the medical center, MRI with bolus contrast is performed according to indications. Discounts are available at night. Come - we will be glad to help you!
Advantages of performing ultrasound at Medscan
You can get an ultrasound done at the Medscan clinic at the best prices in Moscow. The medical center has ample capabilities to conduct comprehensive diagnostics of a wide range of pathologies of various systems and organs. The clinic is equipped with modern expert-class ultrasound machines, which allows you to make an accurate diagnosis and, based on the results obtained, prescribe effective treatment.
The scan is carried out in accordance with the recommendations of European medical imaging societies. The results obtained are accepted both in Russia and abroad.
Sign up for diagnostics by phone or on the website. We also suggest that you read the reviews of our patients, which confirm the high quality of the services provided.
Sign up
Examination technique
The method is based on the unique property of ultrasound waves to easily penetrate the layer of skin, fat and muscles, and be reflected by internal organs, which have a high density. The device's sensor catches the reflected waves and forms a picture of the organ. From this image you can:
- Determine the condition of the examined organs;
- Perform comparative diagnostics;
- Detect all changes over a certain period.
In combination with an ultrasound of the gastrointestinal tract, the doctor can check other internal organs, but the stomach and intestines are practically invisible in such an image. They are hollow and do not reflect ultrasound waves. To examine them, a contrast or water-siphon test is performed.