Rheumatoid arthritis affects millions of people around the world, but we can only offer symptomatic care to the patient as a treatment. Stopping or slowing down the destruction of joints and making the lives of patients as comfortable as possible are the challenges facing the scientific and medical community. But this requires a deep understanding of the biology of the process that constrains the movements of patients. In this article we will try to understand the medical, biological and social questions that rheumatoid arthritis poses to us.
Classification of the disease by radiological stages
The pathogenetic mechanism for the development of rheumatoid arthritis is an autoimmune cross-reaction. The antigenic structure of hemolytic streptococcus, belonging to group B, is similar in structure to the connective tissue of the human body.
When infected with a microorganism (acute or chronic tonsillitis, pyelonephritis, intestinal pathology), the produced antibodies may damage one's own tissues. The joints are the first to suffer. With each new rheumatic attack, the affected area expands and the changes become irreversible and severe.
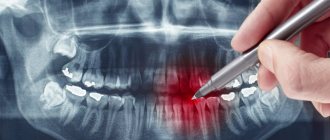
In the early stages, at the first signs, changes may not be detected on an x-ray. But the further the process progresses, the more obvious the damage becomes. There are four radiographic stages of pathology.
First stage
The first stage is characterized as the easiest, the changes are reversible and treatable. Clinically, the patient complains of morning stiffness in the movements of the hands, swelling is visually noted in the area of the small joints of the fingers. More often, the symptoms are associated with a recent infectious pathology (sore throat, tonsillitis, urinary tract infection, streptoderma, etc.).
First stage
The small joints of the hands and feet are the first to suffer. X-ray signs of the first stage of rheumatoid arthritis:
- predominant inflammation of the soft tissue component, which has the form of compaction of structures above the affected joint;
- slight narrowing of the interarticular space, which is not visualized on an x-ray;
- initial manifestations of osteoporosis in the form of local clearing of bone structures and loosening of only the articular surfaces.
Second stage
Clinically, the second stage manifests itself in the form of severe stiffness of the hands for several hours, mainly in the morning and evening. The changes are more pronounced, manifested in the form of swelling and visible deformation, manipulative movements of the hands are significantly difficult (it is difficult for the patient to thread a button into a buttonhole, a thread into a needle, or tie shoelaces).
Second stage
In the area of the joints, a seal is palpated, skin manifestations in the form of rheumatoid nodules are often added, the skin over them is hyperemic. Pain in the legs is acute, walking is difficult, and lameness is observed.
The second radiographic stage of the disease is divided into two subgroups, depending on the degree of damage in the form of erosion of the articular surface:
- What are the stages of rheumatoid arthritis, and how do they differ?
- subgroup A of the second radiological stage is characterized by the absence of erosions on the articular surfaces; the image reveals periarticular osteoporosis in the form of cysts (local clearing of bone structures), areas of bone compaction and a more noticeable narrowing of the gap between the articular surfaces;
- subgroup B of the second radiological stage of the pathology, in addition to the main manifestations, is characterized by the appearance of erosions of the surfaces of the joints, in no more than four places.
Third stage
Clinically characterized by complete immobility of small joints. The pathology extends to large ones: wrist, elbow, knee, ankle, upper shoulder girdle and even intervertebral joints in rare cases. The patient experiences difficulty walking due to severe pain and stiffness of the knee joints.
Third stage
Deformation of the hands occurs in the form of a “walrus fin” (subluxation of the metacarpophalangeal joints) or “swan neck” (formation of persistent flexion contractures of the metacarpophalangeal joints and hyperextension of the interphalangeal joints), inability to abduct the thumb. The patient cannot perform simple manipulative actions with his hands, including difficulty holding a cup, spoon, etc.
Bones become fragile due to a pronounced degenerative process. Cases of subluxations, dislocations, and pathological fractures are becoming more frequent. Healing of damage takes a long time and requires surgical interventions.
Third degree of rheumatoid arthritis on x-ray:
- formation of a single bone block in the area of small joints of the hands;
- more than 5 areas of bone tissue erosion;
- narrowing of the joint spaces of small and large joints;
- the appearance of osteoporotic cysts;
- the formation of soft tissue calcifications (rheumatoid nodules), which in the image appear as rounded areas of darkening, up to 2 cm in diameter, in the area of the soft tissue component around the joints (usually the hands, elbows, knees).
Fourth stage
The terminal stage of the rheumatoid process, which irreversibly disables the patient. Performing simple everyday activities is impossible due to severe pain and persistent joint contractures (immobility). The patient's muscles atrophy due to lack of movement. A person cannot take care of himself (eat, go to the toilet) and requires regular assistance.
Fourth stage
Based on the results of radiography of the joints, the following changes are revealed:
- absence of joint space with compaction in the articulation area and the formation of ankylosis (joint contractures) and subchondral osteosclerosis (due to increased friction of cartilaginous structures in the absence of joint space, they calcify and sclerosis, become dense, lose shock-absorbing capabilities);
- bone growths are formed on the articular surfaces - osteophytes, which have a pointed shape;
- osteoporosis can develop into osteonecrosis.
Process localization
Rheumatoid arthritis usually first affects the small joints of the hands, fingers, and feet. Appearance of the upper limbs:
- the fingers of the hand are deformed, often have a spindle-shaped shape, a “swan neck” or “button loop” shape;
- subluxation of the metacarpophalangeal joints of the hand develops, causing it to take on the shape of a “walrus fin”;
- when the elbow joints are damaged, their flexion contracture (immobility) appears;
- in the elbow area you can feel small painless rheumatoid nodules;
- The shoulder joint is usually affected secondarily; as the disease progresses, it becomes swollen and painful, worsening with movement.
Read more about finger joint arthritis here.
Crunching in joints - when to worry
Intra-articular injections of hyaluronic acid
Appearance of the lower extremities:
The hip joints are rarely affected.
Bone erosion in pathology
Erosion of bone structures is divided into three types:
- Marginal or superficial - detected already at the second stage in joints where there is no cartilaginous structure and friction is more severe.
- Compression - occurs due to aggravation of the process and failure of the bone at the site of injury.
- Deforming - formed due to the destruction of the bone plate, visible bone deformation is visually observed, characteristic of stage 4 of pathology.
Single erosions of the bones of the wrist
When bone erosions occur, it is practically impossible to cure the disease. Long-term multicomponent therapy only helps to stop the progressive process.
Treatment and prevention of rheumatoid arthritis
The pathology is treated by a rheumatologist. Treatment of the disease is complex and multicomponent:
- Diet therapy. The diet should be dominated by foods rich in calcium (milk, cottage cheese, fresh vegetables and herbs); if you are overweight, there is a need to lose weight to reduce the load on the joints of the lower extremities. Products that help maintain cartilaginous structures are also useful: jelly, agar-agar, jellied meat, jellied fish.
- Drug treatment.
- Pathogenetic therapy. Non-steroidal anti-inflammatory drugs (Diclofenac, Nimesil) and steroids (Prednisolone, Dexamethasone) are prescribed; they help relieve pain and reduce inflammation. To prevent the autoimmune process, cytostatics (Methotrexate, Cyclosporine) and biological drugs (Rituximab, Enbrel) are prescribed.
- Etiotropic therapy. Antibacterial agents (Bicillin) are used to prevent relapse of streptococcal infection.
- Symptomatic therapy. Includes the use of chondroitin preparations and hyaluronic acid preparations to maintain cartilage structures, calcium with vitamin D3.
- Physiotherapy and therapeutic exercises. Allows, with the help of physical exercises, electrophoresis, magnetic therapy, to improve hemodynamics in the affected area and activate regeneration processes.
- Operative methods. They are used in extreme radiological stages (third and fourth) in the presence of dislocations, contractures and ankylosis, and pathological fractures.
Prevention of rheumatoid arthritis is the timely and correct treatment of infectious diseases and the prevention of the appearance of chronic lesions. In the initial stages (1-2), it is necessary to develop fine motor skills of the hands and arms - this helps to avoid permanent changes due to normal hemodynamics.
Such patients are recommended to start embroidering, knitting, and drawing. It is also necessary to eat properly to prevent degenerative pathologies of cartilage and bone structures.
Rheumatoid arthritis is a serious pathology that, at extreme stages of development, leads to disability of the patient. The disease can develop both in adulthood and in childhood. Progression leads to a deterioration in overall health and the appearance of persistent irreversible changes in the joint area.
- Rheumatoid arthritis: prognosis and life expectancy
Course and possible complications
There are several flow options. In most children, juvenile arthritis occurs without complications, and long-term remission occurs. Under unfavorable circumstances, there may be relapses in the future. Sometimes juvenile rheumatoid arthritis has a continuously relapsing course. But timely prescribed treatment leads to the development of stable remission.
If the patient is not given adequate treatment in a timely manner, serious complications may develop:
- persistent impairment of limb mobility with subsequent disability;
- cardiopulmonary failure;
- severe visual impairment up to blindness, more common in school-age girls;
- amyloidosis of internal organs, as a result of a long-term inflammatory process, metabolism is disrupted, changes occur in organs and tissues - amyloid is deposited in them - a protein-saccharide complex, leading to the loss of the organ’s function (amyloidosis is a rare complication nowadays);
- infectious complications - bacterial and viral generalized lesions.
How effective is X-ray examination for RA?
Rheumatoid arthritis is commonly called an inflammatory disease of the joints, which is autoimmune (the immune system attacks the cells of its own body, mistakenly perceiving them as foreign and pathological). The reasons why this disease develops have not been precisely established. It is believed that RA can be triggered by:
- infectious diseases previously suffered by a person;
- exposure to toxic substances on the body;
- frequent joint injuries;
- constant hypothermia.
Risk factors include a family history of rheumatoid arthritis. As rheumatoid arthritis progresses, it primarily affects the small joints of the upper and lower extremities symmetrically. The pathological process immediately spreads to the synovial membrane, then to the cartilaginous tissue, eventually forming multiple erosions. The joints become deformed.
An X-ray examination allows the doctor to determine the degree of damage to the joints and determine how deformed the bone and cartilage tissues are. Using the image, the specialist counts the number of erosions that have formed in the bones.
In what cases is x-ray examination indicated and contraindicated?
An X-ray of the joints is prescribed to the patient if he has the following symptoms for a certain period of time:
- pain in the joints;
- limited joint mobility in the morning;
- swelling in the area of the affected joint;
- elevated rheumatoid factor detected in a blood test;
- the presence of rheumatoid nodules (multiple subcutaneous nodular formations near bone structures);
- deformation of the joints noticeable to the naked eye.
Since X-ray radiation is ionizing and can negatively affect the development of the embryo in the womb and small child, X-ray examination is not recommended for women during pregnancy and children. Patients who are in serious condition, suffering from epilepsy, acute and chronic mental illnesses are not examined. But the contraindications listed are relative.
If the attending physician decides that the benefit that radiography will bring to the patient by making a diagnosis will exceed the possible harm, he may, as an exception, prescribe the procedure.
Causes
The exact causes of the onset of this disease have not been established. But the main causative factors are known:
- Hereditary predisposition
– there are cases of family diseases. - The influence of internal (endogenous) factors
- most sick women and men have low levels of male sex hormones; It has been scientifically proven that after using oral contraceptives (OCs), the risk of developing the disease is reduced. - Influence of environmental factors (exogenous).
Infectious agents trigger an autoimmune reaction – an allergy to the body’s own tissues. This is due to the fact that some infectious pathogens contain proteins in their cells that are similar to proteins in human tissue. When these pathogens enter the body, the immune system produces antibodies (IgG), which, for a reason unknown to science, become antigens (substances foreign to the body). They produce new antibodies IgM, IgA, IgG (rheumatoid factors), which destroy them. An increase in the number of antibodies is accompanied by increased inflammation. Some pathogens secrete substances that promote the growth of the articular synovial membrane and enzymes that damage tissue.
As a result of a whole complex of reasons, the cells of the synovial membrane begin to secrete inflammatory cytokines - protein molecules that initiate and maintain inflammation. A long-term inflammatory process develops, cartilage and bone joint tissue is destroyed, and limb deformation occurs. Cartilaginous tissue is replaced by connective tissue, bone growths appear, and joint function is impaired. Very often, the cause of developing autoimmune joint damage is a herpes infection - herpes simplex viruses type 1, 2, cytomegalovirus, Epstein-Barr virus (causes mononucleosis) and other pathogens, for example, mycoplasmas.
Predisposing (triggering, trigger) factors:
- injuries, joint diseases;
- hypothermia, constant exposure to a damp room or damp climate;
- nervous tension, stress;
- the presence of chronic foci of infection is important - tonsillitis, carious teeth, any infectious and inflammatory processes;
- taking certain medications with mutagenic properties.
Stages of RA according to Steinbrocker classification
In modern medical practice, the classification of stages of rheumatoid arthritis developed by Steinbrocker is most often used. He based his research on plain radiographs of the hands and distal feet, performed in a direct projection. With their help, it was possible to identify 4 radiological stages of rheumatoid arthritis, which reflect the nature of the progression of the disease.
Stage 1
This stage is the initial one. It is called periarticular osteoporosis (decreased bone density). The pathological process involves the joints of the hands and metatarsophalangeal joints of the feet. The x-ray visualizes the compaction of the soft tissues surrounding the joint. The bone tissue is thinned, loose, and has increased porosity (these are signs of osteoporosis). There are already cyst-like clearings in its structure. Among the radiological symptoms of the first stage of rheumatoid arthritis may be a narrowing of the joint space.
An appointment with a rheumatologist is necessary for a person who is faced with even a slight restriction of joint mobility in the morning (within approximately 1 hour after waking up). At the first stage, symptoms such as slight swelling of the tissues in the area of the affected joint and short-term pain in the joint during physical activity may also occur.
Periarticular osteoporosis occurs in both adults and children. The disease can progress rapidly, or it can stop in its development for several years and then become more active.
Stage 2
X-ray signs of rheumatoid arthritis at the beginning of the second stage are increased osteoporosis, multiple cysts in the structure of bone tissue, as well as a decrease in the lumen of joint spaces. This stage is called stage 2A, which lasts until the first erosion occurs, that is, bone damage. After this, stage 2B begins, continuing until a maximum of 4 eroded areas appear.
It is customary to classify all bone erosions into 3 categories:
- Marginal superficial (formed in those areas where the articular bones are not covered with cartilaginous tissue).
- Compression (accompanied by the failure of a section of bone due to the formation of a cyst and the progress of periarticular osteoporosis).
- Erosion of the bone tissue of the endplates (appears where the joint connects to the ligaments).
The deformity of the hand or foot is not yet visible on an x-ray.
At the second stage of rheumatoid arthritis, the patient experiences limited joint mobility for several hours a day. During physical activity, pain increases.
Stage 3
This stage of disease development is characterized by the appearance of multiple erosions (from 5 pieces). The muscles around the affected joints atrophy. In addition to periarticular osteoporosis, decreased clearance of joint spaces, and cysts, X-ray signs of rheumatoid arthritis of the hands also include dislocations and subluxations of the joints, and their extended deformation. The most common types of deformities include:
- "button loop";
- "swan neck";
- "walrus fin"
The images show signs of calcification (accumulation of excess calcium salts) in the soft tissues surrounding the affected joint. They are round and dense rheumatoid nodules, the diameter of which is from 2 to 3 cm.
When palpating them, the patient does not experience any painful sensations.
The level of density of calcifications varies, and this is clearly visible on the x-ray. At this stage of the disease, joint pain and immobility are so progressive that many activities require significant effort.
Stage 4
The last stage of RA is manifested by extensive osteoporosis, the spread of erosion not only to the surface of the joints, but also to other areas of bone tissue. The photographs clearly show that osteophytes (bone growths) have formed along the edges of the joints, having different shapes (straight, wavy, with a short or long base).
The fourth stage is also characterized by subchondral osteosclerosis and ankylosis of the joints. A sign of the first is the presence of bone compaction under the articular cartilage, and the second is a fusion of the joint, causing its complete immobility.
The pain in the joints no longer stops. At this stage, the patient may lose the ability to independently care for himself and become disabled.
Physical therapy for knee arthritis
Daily therapeutic exercises for knee arthritis help slow the progression of the disease and reduce the load on the joint by strengthening the muscles and connective tissue. It also reduces pain and discomfort, helps maintain and even restore mobility in the joint.
Examples of exercises for knee arthritis:
- Stand straight, with your back to the wall. Raise your leg to the side so that your shin is touching the wall and your big toe is facing forward, then lower it.
- With your arms folded across your chest, sit on a chair, keeping your back straight. Slowly rise from the chair, and then slowly lower yourself down.
- Standing straight, lift your ankle behind your back so that your heel touches your buttocks. Do not help yourself with your hands unless this is indicated in the exercise for knee arthritis! After 3 seconds, lower your leg.
- Lie on your side on the floor and place your bent arm under your head. Bend your knee and hip joint approximately 90° and lift your knee as high as possible.
- Lying on your stomach, rest your forearm on the floor in front of you. Bend the knee opposite your forearm and, grabbing your ankle with your hand, slowly pull your leg up. During exercises for knee arthritis, the muscles on the front of the thigh should stretch. Then roll over onto your back and, holding your leg under your knee, pull it towards your chest, feeling the stretch in your back muscles.
- Perform the “lying bicycle” exercise until noticeable signs of fatigue appear. Avoid suddenly throwing your leg forward - if the leg muscles are not strong enough for prolonged work, it is better to return to the exercise later.
All exercises for arthritis of the knee joint should be performed 15 times on each leg or (for example, “bicycle”) for at least 1 minute.
Creating an individual set of exercises for knee arthritis and teaching the correct technique should be carried out by a qualified instructor.
Please note that exercise therapy for knee arthritis is only allowed in a state of remission. When arthritis worsens, rest is advisable.
Are the radiological signs of RA different from other types of arthritis?
Using an x-ray, the doctor is able to make a differential diagnosis between different types of inflammatory joint disease. For example, with gouty arthritis, urate crystals (accumulations of uric acid) are visualized on x-rays.
The places where crystals are localized are periarticular tissues and joint space.
At the end parts of the epiphyses (edge of the tubular bone), one can notice the presence of a sclerotic border, and in the cortical layers - cystic defects. The soft tissues along the affected joints are enlarged, and the joint space is widened.
Radiological signs of psoriatic arthritis are different. Osteoporosis, which is an integral companion of RA, in this case occurs only in mutilating forms of the disease. Psoriatic arthritis is accompanied by the appearance of erosions in the distal interphalangeal joints. Such lesions form in the marginal zones of the joints, and then spread to the center.
The tops of the terminal and middle phalanges are ground off, the articular surface is concave, resulting in the visual effect of a “cup and saucer” or “pencils in a glass.”
X-ray signs of glenohumeral periarthritis (inflammation of the soft tissues around the shoulder joint) are the presence of deposits of small calcium crystals (calculous bursitis), osteoporosis of the head of the humerus (this symptom is especially pronounced in the ankylosing form of the disease associated with fusion of the joint and, as a result, its complete immobility).
Alternative methods for diagnosing rheumatoid arthritis
If a classic radiograph did not allow the specialist to make a diagnosis and create a treatment program, computed tomography (CT) may be prescribed for clearer visualization of bone tissue. It is also based on the use of X-rays, but the images obtained during this procedure are not flat, but three-dimensional, layer-by-layer and more accurate. Therefore, even minimal changes in tissues are visible on them. However, CT is associated with greater radiation exposure to the patient's body.
To assess the degree of involvement of the soft tissues surrounding the affected joint in the pathological process, magnetic resonance imaging (MRI) is prescribed. It also allows, like CT, to obtain volumetric images, but involves exposing the patient to a magnetic field and radiofrequency pulses. It is known that X-rays tend to accumulate well in bone tissue and pass through soft tissue without hindrance. Therefore, if the nature of the changes in the latter is poorly visible on x-rays, then MRI displays them in the most complete volume.
Ultrasound examination (US) is more sensitive to detecting erosions in joints, compared to radiography. It is also prescribed to those patients who cannot undergo X-rays, CT, or MRI, since ultrasound has no contraindications. Thus, it is impossible to say unequivocally which examination method for rheumatoid arthritis is the best. The choice of diagnostic method is made by the attending physician based on the symptoms with which the patient came to him.
How rheumatoid arthritis is treated at the Paramita clinic
Our clinic’s specialists have developed their own approach to the treatment of rheumatoid arthritis. It is a combination of the most advanced Western and traditional Eastern techniques.
First, the patient is examined. Laboratory, instrumental and oriental methods for diagnosing rheumatoid arthritis are used. Then the attending physician draws up an individual treatment plan. Our clinic uses the following RA treatment methods:
- drug therapy – combinations of the most modern drugs and advanced techniques are used;
- herbal medicine and certain methods of traditional medicine - their skillful combination with drug therapy can reduce the drug load on the body;
- physiotherapeutic procedures - speed up the healing process;
- therapeutic exercises, kinesitherapy, massage - improve blood circulation, prevent joint destruction and muscle atrophy;
- PRP therapy (plasmolifting) is a modern method of stimulating recovery processes using the patient’s own platelets, processed using a special technique;
- reflexology (RT) – influence on active points (AP) on the surface of the human body associated with various organs and systems; our specialists have been trained in China and are proficient in all methods of influencing AT: acupuncture, moxibustion, acupressure and many others; RT courses can completely relieve the patient from relapses of the disease;
- pharmacopuncture – combines Western and Eastern methods: modern medications are introduced into the AT, which greatly enhances the effectiveness of treatment.
The result of this treatment is long-term remission, a positive prognosis and almost complete restoration of the patient’s quality of life.
We combine proven techniques of the East and innovative methods of Western medicine.
Read more about our unique method of treating arthritis
Conclusion
X-ray examination is a fast, inexpensive and very informative diagnostic method that allows not only to identify rheumatoid arthritis, but also to accurately determine its stage. Most often, x-rays are used as an initial examination of patients with symptoms of RA. If necessary, for the purpose of in-depth diagnosis, the attending physician may decide to prescribe a different instrumental research method to the patient.
An x-ray will help you understand how far the disease has progressed. The stages of rheumatoid arthritis are visible on it, but only a specialist can accurately determine the problem. In the later stages, almost anyone can determine the presence of a problem by appearance - deformation of organs occurs. However, there are changes that are not visible to the naked eye.
This:
- Reducing joint spaces;
- Erosion of bones (that is, their thinning, the appearance of “dips”);
- Ankylosis (bones fusion with each other).
But since there are so many diseases of bones and joints, one x-ray is not enough to diagnose and determine the stage of rheumatoid arthritis. A good doctor will supplement this with a blood test.
What will happen if left untreated?

Stages of rheumatoid arthritis
If rheumatoid arthritis is not treated promptly, it will begin to progress rapidly in the future, which increases the risk of developing possible complications:
- deformations and loss of joint functions leading to disability;
- changes in the neuromuscular system with neuropathies and a decrease in muscle volume;
- damage to the cardiovascular system in the form of vasculitis, endocarditis, microinfarctions;
- kidney disorders with the gradual formation of chronic renal failure;
- damage to the organs of vision, including ulcerative ones;
- damage to the pleura and lungs - the development of pleurisy and interstitial pneumonia;
- development of anemia and systemic thrombosis of small blood vessels.
Tests in addition to X-rays
To diagnose rheumatoid arthritis, tests are done for markers of inflammation (that is, markers that show that the body is fighting it) and rheumatoid factor. However, it is important not only to do the analysis, but also to interpret it correctly.
Analysis for inflammatory markers. If the result is positive, this may be an indication of some other disease, not necessarily arthritis. Which one exactly will be revealed by further research.
Analysis for markers of rheumatoid arthritis. It is worth diagnosing with great caution, because it occurs in 5% of healthy people (and indicates a predisposition to the disease, but not the disease itself), and it does not occur in approximately 50% of patients. That is, it is only indirect evidence of the presence of rheumatoid arthritis.
Therefore, tests for other diseases are also necessary. If, as a result of the examination, no other pathogens are found, and the x-ray indicates pathological changes, the doctor diagnoses “rheumatoid arthritis”.
General clinical recommendations
To prevent exacerbations of rheumatoid arthritis, it is necessary to reduce the activity of the pathological process. This can be achieved if:
- Lead a healthy lifestyle, follow a daily routine, avoid stress and high loads.
- Do not smoke, do not drink alcohol.
- Regularly perform exercises agreed upon with your physical therapy doctor.
- Follow the recommended diet.
- Treat concomitant diseases in a timely manner and eliminate foci of infection.
- Conduct courses of anti-relapse treatment for rheumatoid arthritis in a timely manner.
Rheumatoid arthritis requires a serious approach to treatment not only on the part of the doctor, but also on the part of the patient, who must follow all medical recommendations. At the Paramita clinic you will find such a serious approach to business. The main thing is not to delay your visit to the doctor!
Literature:
- Rheumatology: national guidelines. / Ed. E.L. Nasonova M.: GEOTAR-Media, 2008. 720 p.
- Karateev D.E. Retrospective assessment of long-term basic therapy in patients with rheumatoid arthritis // Scientific and practical rheumatology. 2003. No. 3. pp. 32–36.
- Chichasova N.V., Brodetskaya K.A., Igolkina E.V. et al. 18-month use of leflunomide - clinical effectiveness, tolerability and effect on the progression of erosive arthritis in patients with RA // Scientific and Practical Rheumatology. 2004, No. 2. Theses “School of Young Rheumatologists. No. 11, p. 124.
- Smolen JS, Landeve R, Breedveld FC et al. EULAR recommendation for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs // Ann. Dis. 2010, 69: 964–975.
- Emery P., Breedveld F.C., Hall S. et al. Comparison of methotrexate monotherapy with a combination of methotrexate and etanercept in active, early, moderate to severe rheumatoid arthritis (COMET): a randomized, double-blind, parallel treatment trial // Lancet. 2008, 372: 375–382.
- Dougados M., Emery P., Lemmel EM et al. When a DMARD fails, shoud patients switch to sulfasalazine or add sulfasalazine to continuing leflunomide? //Ann. Dis. 2005, 64: 44–51.
Themes
Joints, Pain, Treatment without surgery Date of publication: 03/26/2020 Date of update: 11/17/2020
Reader rating
Rating: 5 / 5 (2)
What does the lack of timely diagnosis using X-rays lead to?
Some people believe that due to their young age they cannot get rheumatoid arthritis, especially in the advanced stages. And this is a big mistake, because the disease is rapidly growing younger and occurs in those who are only 30 or 20 years old. The reasons are trivial - environmental degradation, unhealthy diet, sedentary lifestyle.
Heredity plays a big role. If there are people in your family who have had or are suffering from rheumatoid arthritis, the appearance of its symptoms is a very alarming symptom.
Etiology (causes)
The etiology of the disease is not fully understood, but it is believed that its main cause is a hereditary predisposition. This is proven by cases of family diseases. The environment in which the sick person lives and the climate are also important. More often, the development of the disease occurs in damp, cold climates. But climate still plays more of a triggering factor. They are also:
- infectious agents - bacteria, fungi, viruses (JRA develops some time after an infection);
- vaccinations - in some cases, the disease began after vaccinations against measles, rubella and mumps;
- joint injuries;
- hypothermia;
- prolonged exposure to direct sunlight, sunburn.
What signs of rheumatoid arthritis are visible on x-ray?
On an x-ray, the doctor can see various signs of the disease that are not noticeable at first glance and examination. An x-ray is taken of the part of the body in which the patient complains of pain. Rheumatoid arthritis can be concentrated in one part of the body or affect them all at once (hands, toes, knees, shoulders, elbows). Most often the problem begins in the extremities.
X-rays show erosion and inflammation. How strongly they will be expressed depends on the stage of the disease.
Morbidity statistics
Juvenile rheumatoid arthritis (JRA) is a special form of rheumatoid arthritis that develops before the age of 16 years. It is characterized by an acute onset, a chronic progressive course, damage to one or two large joints and internal organs.
Some statistics:
- the prevalence of this pathology in the world is 0.05 - 0.6%;
- number of cases per year per 100,000 children:
- in the world - 2-19;
- in Russia 16.2.
At risk are teenage girls aged 14 to 16 years.
In Russia, they officially adhere to the classification of juvenile rheumatoid arthritis according to ICD-10 (code M08).
Determining the stages of rheumatoid arthritis using x-rays
Doctors have their own requirements for how to make a diagnosis, which they follow. For example, the stage of rheumatoid arthritis is determined by the joint that suffered the most, judging by the x-ray.
That is, if damage to the joints of the legs corresponds to stage 2, and to the joints of the arms to stage 4, then the patient will receive a diagnosis of stage 4. In itself, it is very difficult, but since this concerns not the whole body, but its individual parts, the situation is not as hopeless as it might seem at first glance.
Of course, all this cannot be done by a non-specialist, but with appropriate training a person can roughly understand the condition of the joints. However, to make an accurate diagnosis and determine the stage, a doctor is needed. If there are doubts about the doctor’s qualifications (he is not interested in treatment, he prescribes only ointments and/or tablets), you can show the same x-ray to another specialist.
There is no need to take a new image (unless another doctor insists on this due to the poor quality of the old image or the large amount of time that has passed).
Still, every X-ray is radiation, albeit a small one.
To make a judgment regarding the stage of rheumatoid arthritis, rheumatologists analyze:
- The degree of destruction of joints, bones, cartilage on x-ray;
- Number of erosions;
- Signs of inflammation in the picture;
- Presence of cysts.
But in very early stages or in cases of small erosions, it is difficult to see all the details of rheumatoid arthritis on x-rays. Then MRI is used. The resolution of this equipment is higher and more details can be obtained.
Forms of juvenile arthritis
Based on the nature of the course and the predominance of certain symptoms, the following forms are distinguished:
- Pauciarticular juvenile rheumatoid arthritis in children aged 1 to 6 years.
The most common articular form. It occurs mainly in girls. One or two large joints (almost always the knees) are asymmetrically affected. The development of uvitis is characterized by the appearance in the blood of antinuclear factor (ANF) - antibodies to proteins of the cell nucleus and specific antibodies to tissues - rheumatoid factor (RF). It often proceeds favorably with long-term remissions, but sometimes turns into polyarthritis. Severe joint damage is possible in 40% of children. - Juvenile rheumatoid polyarthritis is seropositive.
It develops mainly in girls over 8 years of age. Joints of different sizes are affected. The earlier the disease begins, the more serious the prognosis, and disability is possible. RF and ANF are detected in the blood. - Juvenile rheumatoid polyarthritis is seronegative.
It occurs predominantly in girls under 15 years of age. Joint lesions are numerous, often involving the cervical and temporomandibular joints. RF is not detected in the blood. In its course, this form is similar to the adult version of the disease. Most often the course is favorable, but sometimes persistent dysfunction of the limbs appears. - Juvenile rheumatoid arthritis with systemic onset.
The incidence does not depend on gender and age. The onset is acute with damage to joints, lymph nodes and internal organs. In systemic juvenile rheumatoid arthritis, any joint can be simultaneously affected. High concentrations of RF in the blood. - Juvenile idiopathic arthritis.
A disease of unknown etiology. One of the most common diseases. The diagnosis is made after excluding other forms of JRA.

Diagnosis of juvenile joint lesions
What do the stages of rheumatoid arthritis look like on an x-ray?
The first stage is the easiest, but even it can be seen in the picture. As already mentioned, rheumatoid arthritis most often begins in the extremities, so photographs are taken of the hands where changes occur. Signs of the first stage of arthritis:
- The soft tissue around the affected joints is thickened;
- The bones themselves are more porous, even, one might say, loose;
- The joint space is narrowed, but still weakly.
At this stage, a person feels that it is more difficult for him to move his limbs in the morning. There is slight swelling. These two symptoms are enough to start sounding the alarm and taking an x-ray. Moreover, symptoms can appear in both adults and children. Pain may be added to limited mobility in the morning. If rheumatoid arthritis is diagnosed early at a young age, you can avoid its rapid development in adulthood and old age.
Second stage. Cysts are added to existing symptoms. These are growths on bone tissue that deform the arm and further limit its mobility. The joint gap becomes even smaller. Osteoporosis (fragility and looseness of bones) is on the rise. This is what is seen on an x-ray. But in real life, mobility decreases and pain manifests itself not only in the morning, but also during the day.
It is important to note that the second stage is divided into 2 types - 2A and 2B. At stage 2A of rheumatoid arthritis, there is still no erosion in the image - pronounced bone damage, but at stage 2B they already appear. The most common type of erosion is marginal, that is, along the border of the joint.
The most vulnerable areas are those where the cartilage does not cover it. Another type is the failure of a section of bone, this is called compression erosion. The third type is destruction of the endplate (it connects the ligament to the joint). And if only a very good specialist can determine stage 1 rheumatoid arthritis by x-ray, then even an average doctor should be able to handle stage 2. In real life, the patient suffers from pain during exercise.
The third stage of rheumatoid arthritis on x-ray is characterized by a large number of erosions, namely more than 5. The doctor also notes that the muscles atrophy due to rheumatoid arthritis, as a result of tissue damage and limited mobility of the organ. The interarticular spaces are still narrower. Subluxations and dislocations of the joints appear, they are already visually deformed.
In the soft tissues near the diseased joints, in the photographs you can see nodules that form from calcium salts. This is called calcification. The nodules not only contribute to the progression of the disease, but also cause pain when touched. This is about x-rays. But in real life, a person already has to make significant efforts to perform the simplest everyday operations.
This stage is especially painful for those who engage in sports or physical labor, as it deprives them of the opportunity to have a full load.
All the signs that were mentioned in the description of the previous stages are present in X-ray 4, but to a more pronounced degree. New ones are also appearing.
Erosion. At stage 4 of rheumatoid arthritis, on x-rays they are visible not only on the joints, but also on the bones. The joint spaces narrow so much that bone fusion occurs (ankylosis). Osteophytes appear. Roughly speaking, osteophytes are growths along the edges of joints. They have different shapes. At first they are small, and then they grow larger and larger.
Osteophytes even change the appearance of the limb, visible to the naked eye. A bone compaction is visible under the cartilage of the joint. It is called subchondral osteosclerosis. In fact, this compaction is an attempt by the body to protect itself from destruction, as the cartilage breaks down and the bones begin to rub against each other.
And to prevent their complete destruction, the body provokes the appearance of such compactions that are visible on x-rays. In real life, it becomes even more difficult for a person to perform the simplest household operations. The pain is very severe and difficult to endure without taking painkillers.
Symptoms and types of arthritis
There are several bases for classifying arthritis, which are used in making a diagnosis, clarifying the causes and symptoms of arthritis of the joints, and selecting treatment.
Due to origin
Based on their origin, arthritis is caused by:
- Infectious or parasitic infection of the body
. Reactive inflammation of the joints and periarticular tissues, as well as other symptoms of arthritis, can occur 4-6 weeks after the disease, as the body’s response to the vital activity of the pathogens themselves or a massive amount of antigens produced to combat them. Infectious arthritis also includes generalized pathologies that affect more than 3 joints and are associated with chronic infections (tuberculosis, syphilis, viral hepatitis, HIV and others). Infectious arthritis can also be triggered by the unwanted growth of microflora in the cecum in the postoperative period, as well as infection by worms or protozoa. In rare cases, inflammatory pathology occurs as a response to vaccination (usually occurs in children). With penetrating wounds and injuries, which are accompanied by ruptures of blood vessels, as well as with bites of blood-sucking insects in the periarticular area, direct infection of the joint capsule is possible. - Non-infectious reasons
. Symptoms and causes of arthritis of the joints may depend on the presence in the body of such pathologies as: - neoplasms (arthritis develops due to metastasis to articular or periarticular tissues or due to the body’s immune response to a tumor); - diseases of the blood and blood vessels (anemia, hemorrhages); - pancreatitis, pancreatic cancer (due to the influence of enzymes on the synovium of the joint); — decompression sickness due to non-compliance with safety precautions when diving; - metabolic disorders (diabetes mellitus, gout); - hormonal changes in the body (hormonal imbalances, menopause in men and women, age-related changes); - allergies to food, drugs, vaccines or chemicals, rejection of prostheses by the body; — bruises, sprains and ruptures of ligaments, muscles, tendons, fractures, as well as other injuries (including repeated microtraumas, for example, when working with vibration equipment); - wear of the joint due to instability of chondrocytes and other pathologies of cartilage tissue; - monotonous loads and the unfavorable influence of climatic and sanitary conditions in the workplace (in this case we can talk about the so-called benign arthritis, which goes away by itself when conditions change). - Unspecified reasons
. As a rule, these include secondary arthritis, which occurs against the background of autoimmune diseases (including hepatitis, rheumatoid polyarthritis, amyloidosis, systemic vasculitis, and others). Since the causes of these diseases are still not clear, the accompanying symptoms and types of arthritis also have an unspecified etiology.
According to clinical manifestations
Arthritis can affect both small and large joints, being limited to one joint or affecting several at once. Therefore, rheumatologists divide the disease into the following types:
- monoarthritis
(affects only one joint); - oligoarthritis
(observed in 2-3 joints); - polyarthritis
(occurs in 4 or more joints at the same time).
According to symptoms
According to the severity of arthritis symptoms:
- acute arthritis
(characterized by sudden onset, severe pain and rapid progression); - arthritis with a chronic course
(develops slowly, periods of remission alternate with periods of exacerbation, pain is less pronounced than with acute arthritis).

There are many symptoms of arthritis
How to recognize rheumatoid arthritis on x-ray
To understand that the X-ray shows exactly the signs of rheumatoid arthritis, you need to know how to interpret the image. Let's look at what certain signs look like on an x-ray.
Tissue compaction around the affected joint. This symptom is visible even in photographs of stages 1 and 2 of rheumatoid arthritis. The tissue around the diseased area appears smoother than that around the healthy area. They are also more transparent.
Calcifications. These are the nodules discussed above. On x-rays they simply appear as shadows or round formations. The shape does not need to be round. In rheumatoid arthritis, they can be in the form of dashes or small formations on the edge of the joint. Moreover, their density can also be different.
Some are just forming, while others are bone-like in density. Calcifications are more clearly visible on an MRI image.
Tendinitis and tenosynovitis. This is a hardening of a tendon or ligament where it attaches to the bones. This process is also visible on x-rays. An additional sign is calcifications around such compactions.
Osteoporosis. The actual destruction of the bone, increasing its fragility and weakness. Osteoporotic areas of the bone/joint appear to appear more transparent. The endplates appear thinner.
Narrowed joint space. It is possible to determine that it is narrowed due to rheumatoid arthritis only if there is a similar photograph of the healthy arm. The doctor can do this without such an image, since he knows exactly what the ratio should be. However, in later stages, even a non-specialist can see that the gap on the x-ray is significantly narrowed.
Unevenness of the articular surface. These can be both failures and growths. In the first case we are talking about erosion, in the second - about osteophyte. Osteophytes have different shapes on x-rays in rheumatoid arthritis. But it is important that they change the normal shape of the joint at a later stage. Possible crooked fingers. This is often visible without an x-ray, but the image confirms the suspicions.
Osteolysis. Rarely seen. This is a process in which bone is essentially resorbed. Accordingly, it is absent on x-rays in some areas. This sign indicates a big problem and the need for serious treatment of rheumatoid arthritis.
If tissue necrosis occurs (its death due to insufficient blood supply), this area will appear darker on the x-ray, looking like a shadow. In this case, this shadow is surrounded by a contour lighter than the color of the rest of the bone.
An indirect sign of necrosis in arthritis is the proliferation of osteophytes.
Osteophytes. Growths on the edges of joints in rheumatoid arthritis, which have already been discussed above. The more severe the stage, the larger the osteophyte. Thus, the answer to the question of whether arthritis is visible on an x-ray is yes.
It cannot be cured, but it can be alleviated. Current treatment strategies for rheumatoid arthritis
Since a clear target for the autoimmune process in rheumatoid arthritis cannot be found, it is not yet possible to develop a specific treatment. You can only reliably stop the inflammation and try to maintain the patient’s state of remission for as long as possible. The main modern treatment strategies are aimed at selecting the most effective anti-inflammatory drugs [20]. Below we will talk about their various options.
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen , reduce inflammation and reduce pain. They inhibit the activity of cyclooxygenase enzymes, which promote the production of prostaglandins - substances that increase the sensitivity of receptors to pain mediators. Unfortunately, NSAIDs, like any medicine, have side effects. As a result of long-term use of these drugs (especially if they are not selective - Ed.), damage to the mucous membrane of the stomach and duodenum may develop, which will lead to the formation of ulcers and bleeding. Diarrhea and nausea may also sometimes accompany treatment. In addition, suppression of prostaglandin production negatively affects the functioning of the vascular epithelium, which can lead to myocardial infarction, thrombosis and, due to decreased renal blood flow, acute renal failure.
Corticosteroids are another class of drugs that reduce inflammation and pain. These include, for example, prednisolone . These drugs are stronger than NSAIDs and therefore have more serious and frequent side effects, such as type 1 diabetes [21], obesity, and brittle bones caused by their loss of calcium. Because of this, corticosteroids are prescribed only when the severity of the symptoms of rheumatoid arthritis increases, and old methods of pain relief are no longer effective.
The so-called basic anti-inflammatory drugs (DMARDs) are usually considered as a separate therapeutic group. It is very important for the best long-term results that the patient begins taking these drugs as early as possible. The fact is that these drugs have immunosuppressive properties, that is, the ability to suppress the activity and division of immune cells, as well as joint cells. Accordingly, the autoimmune process, which literally eats up the joint affected by rheumatoid arthritis, can be limited at an early stage. The most common and effective DMARDs are methotrexate , leflunomide and sulfasalazine .
The effect of taking DMARDs is observed in 60% of patients with rheumatoid arthritis, but it develops very slowly, so the course of taking the drug lasts at least six months. If during therapy the patient does not feel any improvement, then, as a rule, he is prescribed combination treatment with several DMARDs. However, you need to be careful with this tactic, as it significantly increases the likelihood of side effects.
Side effects of DMARDs typically affect the gastrointestinal tract and hematopoietic system. The fact is that DMARDs suppress the proliferation of the most actively dividing cells in our body, that is, immune cells (which is what their therapeutic effect is based on), but also other blood cells (for example, megakaryocytes, from which platelets are formed, and red blood cells) and cells intestinal epithelium, suffering completely undeservedly.
Biologics are a relatively new treatment for rheumatoid arthritis. They are antibodies or soluble receptors and can therefore specifically block certain molecules involved in the development of rheumatoid arthritis. Such “target molecules” can serve as pro-inflammatory cytokines and receptors on the surface of immune cells (Fig. 6).
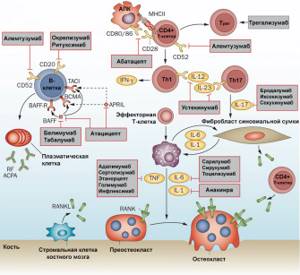
website
The most common drugs that block proinflammatory cytokines are antibodies to tumor necrosis factor (TNF), interleukin-6 and interleukin-1. The former include, for example, infliximab and adalimumab , monoclonal antibodies that bind TNF. To block TNF, etanercept , a drug consisting of a soluble TNF receptor and the Fc fragment of an antibody (IgG1). The therapeutic antibody tocilizumab blocks the interleukin-6 receptor, which also helps reduce inflammation. Anakinra is a genetically engineered version of the IL1-RA protein, a natural interleukin-1 receptor antagonist. By attaching to the receptor, anakinra blocks the transmission of a signal through it and, therefore, the launch of an inflammatory response.
As readers might have already guessed, in the treatment of rheumatoid arthritis it was simply impossible not to use agents that block the costimulatory signal to the T cell from antigen-presenting cells. This is the basis for the action of the previously mentioned abatacept , consisting of the CTLA-4 molecule (a blocker of costimulatory molecules on the surface of antigen-presenting cells) and the Fc fragment of IgG1.
Since B cells play an important role in the pathogenesis of rheumatoid arthritis, suppression of their activity can also be a fairly effective treatment strategy. The use of rituximab , an anti-CD20 monoclonal antibody drug, results in the selective removal of mature B cells (antibody-producing plasma cells are not affected) and a decrease in inflammation.
The use of biological drugs in combination with DMARDs mutually enhances their therapeutic effect, so these two groups of drugs have become the most significant in the treatment of rheumatoid arthritis. Alas, this is not the case in all countries. The high price of biological drugs greatly hinders their widespread use. In Russia, the cost, for example, of infliximab is about 50 thousand rubles per 100 mg. This is not sufficient even as a starting dose in a treatment that requires the patient to receive the drug at least every two months for a year or more [20].
Unfortunately, biological drugs are also not without serious side effects, primarily associated with a lack of selectivity in blocking molecules important for an effective immune response. The use of such drugs may weaken the adequate immune response to infection. Almost all biological drugs contain antibody fragments, and this can lead to the development of an autoimmune response in which they play the role of antigens. Targeting the action and reducing the immunogenicity of the drugs themselves are among the most important problems that can be solved using new approaches to the development of biological drugs.
Constant monitoring of a patient with rheumatoid arthritis and timely change of treatment strategy in case of ineffectiveness of a particular drug can maintain a state of remission for years and even decades. Without proper treatment, inflammation and associated symptoms develop quickly enough that it can lead to surgical removal of the affected joints.
X-ray or MRI for rheumatoid arthritis?
Those who suspect they have rheumatoid arthritis are faced with a choice: X-ray or MRI? It is ideal to use both methods in combination, supplementing them with analyses. At the first stage of the disease, x-rays are practically useless, since pathological disorders are poorly visible. If you are worried about immobility and pain in the morning, it is better to consult an MRI.
At the same time, MRI is a more expensive procedure. Magnetic resonance imaging also has another drawback - the image provides information about the existence of a problem, but it is difficult to determine from it what kind of joint disease the patient is affected by. To classify and confirm that it is rheumatoid arthritis, an x-ray will also be required.
Bibliography:
- https://www.rmj.ru/articles/revmatologiya/stadii_rentgenologicheskih_izmeneniy_v_sustavah_pri_revmatoidnom_artrite/
- https://osnimke.ru/kosti-i-sustavy/revmatoidnyj-artrit-rentgen.html
- https://prorentgen.ru/kosti/kak-opredelit-stadiyu-revmatoidnogo-artrita.html
- https://mysustavy.ru/priznaki-i-stadii-revmatoidnogo-artrita-na-rentgene-i-mrt/