1.General information
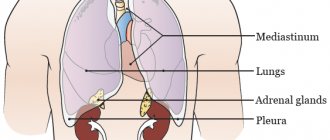
The compound word “atelectasis” can be translated from Greek as “incomplete, incomplete stretching,” although stretching here refers rather to the effect of a sail unfolding in the wind. In order to function normally and fully, providing rhythmic breathing and vital gas exchange, the lungs must be in a freely expanded state. However, under certain unfavorable conditions, they “collapse” - just like a helplessly drooping sail - which causes one or another degree of respiratory failure (depending on the scale of atelectasis).
There are many clinical types of atelectasis; each of them can be caused by various reasons (see below), but in any case this condition is dangerous, and in severe cases – life-threatening. Thus, atelectasis turns out to be a fatal factor in approximately 3% of cases of death on the operating table (and up to 20%, if we take only cardiac surgery); about 3.5% of newborn mortality is caused by congenital atelectasis, and up to 6% by respiratory distress syndrome.
A must read! Help with hospitalization and treatment!
Atelectasis versus pneumonia on ultrasound
Atelectasis must be distinguished from other consolidation variants such as pneumonia or pulmonary embolism.
During consolidation, alveolar air replaces exudate, and the density increases to that of the liver.
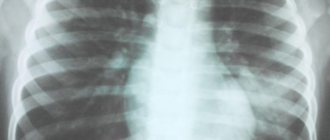
On X-rays and CT scans, pleural effusion, pneumonia, and atelectasis appear equally white.
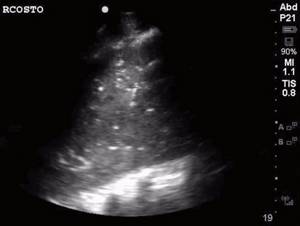
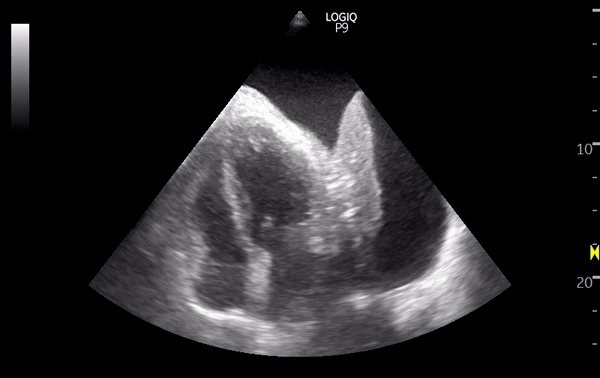
The ultrasound method is much better suited for the differential diagnosis of these conditions.
The effusion appears as an anechoic zone between the visceral and parietal layers of the pleura.
Pneumonia - consolidation with jagged edges and dynamic air bronchogram.
A dynamic bronchogram indicates airway patency and excludes atelectasis.
Parapneumonic effusions are modest to moderate and typically contain echogenic debris.
With atelectasis, a static air bronchogram may persist, but never a dynamic one.
You can notice the “pulse” of the lung, as the parenchyma moves synchronously with the contraction of the heart.
Compression atelectasis - tiny compressed lung, large pleural effusion.
Obstructive atelectasis - consolidation without bronchogram, moderate pleural effusion.
A tissue-like pattern appears after complete absorption of air by the capillaries of the lungs.
On the contrary, lung pulsation is immediately visible, since it arises from the lack of air exchange.
For example, when the right bronchus is intubated, ventilation of the left lung suddenly stops.
The sliding of the pleura disappears, the pulse of the lung appears, but the tissue-like pattern is absent.
With CDK, radial pulmonary trunks (arteries, veins) are identified in areas of consolidation.
It is possible to distinguish between normally branching vessels or crowded parallel ones in atelectasis.
Rice. The vascular trunks in pneumonia are radial, and in atelectasis they are crowded and parallel.

Rice. The pulmonary arteries have a high resistance pattern and the pulmonary veins have a phasic flow pattern.
2. Reasons
Atelectasis is not a disease, but a pathological phenomenon; Accordingly, there is no single pathogenesis here; the causes and mechanisms of development can be very different.
Primary, congenital atelectasis of newborns is caused, as a rule, by obstruction (clogging, blocking) of the airways with mucus and/or amniotic fluid, or by a deficiency of surfactant, a special surface-active secretion that normally lines the alveoli.
Secondary, acquired atelectasis occurs due to the following factors:
- complicated cardiac surgery, thoracic or abdominal open surgery, as well as intubation anesthesia as such;
- a number of diseases of the bronchopulmonary system (including tumor processes, tuberculosis, various types of pneumonia, pulmonary infarction, chronic bronchitis, and many others);
- severe open thoracic injuries with pneumo-, hydro-, hemothorax (penetration of air, liquid or blood into the pleural space, respectively);
- inhalation of foreign bodies or masses;
- prolonged adynamia (immobility) in bedridden patients.
The main risk factors include:
- infancy and old age (immaturity or aging of tissues, organs, structures of the respiratory system);
- neurological bulbar disorders that make swallowing difficult;
- fetal prematurity (sharply increases the risk of congenital atelectasis);
- overweight;
- smoking;
- long-term use of certain medications that are active against the respiratory system, etc.
Visit our Pulmonology page
Experience, the son of difficult mistakes

Rice. A tissue-like structure without a bronchogram may at first glance appear to be atelectasis.

Rice. With CDK, blood flow in a blood clot is not determined, unlike pneumonia and atelectasis.
Rice. Dynamic air bronchogram: echogenic mobile artifacts in consolidation.
Rice. Prominent pleural effusion and lung collapse are similar to cardiac tamponade.

Rice. Standard access along the axillary lines.

Subcostal access: diaphragm line - ascites in front, pleural effusion in back. Tags: easy lectures ultrasound
3. Symptoms and diagnosis
There are several clinical types of atelectasis (obstructive, distensional, compression, mixed), but its dominant and most dangerous consequence is respiratory failure. There is cyanosis (blueness of the skin), shortness of breath with arrhythmic, shallow, rapid breathing, tachycardia, “failure” of blood pressure, and, less often, pain in the area of the collapsed lung. In newborns, “moaning wheezing”, muscle tension, and cramps are often pronounced.
The severity of the clinical picture varies from asymptomatic to fatal. Acute deficiency of bound oxygen in the blood (hypoxemia), a shift in blood pH to the acidic side (acidosis), general oxygen starvation (hypoxia), progressive changes in the lung parenchyma and the structure of the respiratory tract (including due to chronically increased load on unaffected areas ) pose a real threat to life.
Timely and accurate diagnosis of pulmonary atelectasis is critically important, but it is often associated with a number of difficulties, since symptoms may be nonspecific. In addition to a thorough study of complaints and anamnesis, auscultatory and percussion examination is performed; a number of laboratory blood tests are prescribed (general clinical, biochemical, determination of pH and gas composition, detection of antibodies, etc.). According to indications, instrumental studies are carried out: spirometry, radiography, bronchoscopy (including for therapeutic purposes), CT, endoscopic biopsy for histological analysis.
About our clinic Chistye Prudy metro station Medintercom page!
Diagnostics
Diagnostic measures include collecting anamnesis, examining the patient, and using special research methods.
The patient's breathing weakens and asymmetry of respiratory movements appears. When percussing (tapping) the chest in the projection of the atelectatic focus, a shorter and dull sound is determined than in the surrounding tissues.
The most informative method to accurately make a diagnosis is radiographic examination. With atelectasis, the lungs change in density, which is reflected in the photographs as darkening of the affected area. The dome of the diaphragm changes configuration, the mediastinal organs move to the area of the compressed area. There is a decrease in the distance between the ribs in the area of the pathological focus.
To determine the gas composition of the blood, a biochemical study is carried out. To clarify the degree and extent of pathology, bronchoscopy, angiopulmonography and bronchography, and computed tomography are performed.
4.Treatment
First of all, it should be clearly understood: when symptoms of atelectasis (and, in general, respiratory failure) appear, any “folk”, “home” or other self-medication is deadly. Immediate hospitalization with round-the-clock monitoring of the condition in a specialized hospital is required.
The nature and scope of assistance is determined, of course, by the diagnostic results: the primary goal is to eliminate the immediate cause of atelectasis (see above). In some cases, solving this problem requires urgent large-scale surgical intervention, in others it is possible to manage with bronchoscopy and drainage. According to the indications, drug treatment is prescribed (for example, respiratory analeptic stimulants, corticosteroid hormonal drugs, antibiotics in case of infection, which almost always happens in cases of secondary atelectasis, surfactant substitutes in case of its deficiency in newborns, etc.), oxygen therapy, artificial ventilation. In most cases, once acute symptoms are relieved, physical therapy is very effective.
The prognosis depends on the specific etiology, the general condition of the patient, the accuracy of diagnosis, as well as the timeliness and adequacy of the care protocol applied.
Treatment
Therapeutic measures are carried out after diagnosis, taking into account the etiological causes of the disease.
If a foreign body is present, it is removed, after which the mucous membrane of the bronchial tree is washed with enzyme solutions with antibiotics and an antiseptic. The accumulated exudate is sucked off or drained through active coughing.
Treatment of the compression form requires eliminating the causes that led to compression - eliminating the defect of the pleural cavity, draining exudate, blood or pus.
The acinar form is treated by administering surfactant preparations. Postoperative atelectatic conditions are eliminated by suctioning secretions from the trachea and chest massage. In parallel, bronchodilators and enzyme preparations are used.
Contraction forms of pathology do not respond well to conservative treatment; the affected areas are excised surgically.
Regardless of the cause of pulmonary atelectasis, anti-inflammatory therapy is carried out, which is aimed at eliminating the inflammatory process (or preventing it).
At the recovery stage, patients are shown physiotherapeutic procedures in the form of electrophoresis with platyphylline and aminophylline.
Prevention
Preventive measures to prevent the development of such a disease include the following rules:
- maintaining a healthy and active lifestyle;
- competent management of the recovery period after serious illnesses and operations on the bronchi or lungs;
- taking medications strictly as prescribed by the attending physician;
- control of body weight so that it does not exceed the norm;
- preventing foreign objects from entering the bronchi;
- Regularly undergoing a complete preventive examination at a medical institution.
The prognosis of pulmonary atelectasis directly depends on the cause that caused it and timely treatment. A severe course or fulminant form of the disease very often leads to complications, often leading to death.
What to do?
If you think you have pulmonary atelectasis
and symptoms characteristic of this disease, then a pulmonologist can help you.
Source
Did you like the article? Share with friends on social networks: