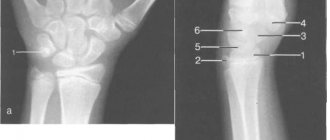
X-rays of the foot and ankle are a painless test that uses a safe amount of radiation to image these structures. During the examination, an x-ray machine emits x-rays through the foot and the image is recorded on special x-ray film or a computer. This image shows the soft tissues and bones of the foot, which include the bones of the lower leg (the fibula, tibia, and talus, which together make up the ankle joint), the metatarsals (the forefoot), and the phalanges (toes).
The X-ray image is black and white. Dense structures that block the passage of X-rays, such as bones, appear white. Softer tissue, such as muscle, allows X-rays to pass through and appears darker.
A radiographer in a hospital's radiology department monitors the taking of x-rays. Typically three different pictures of the foot are taken: one from the front (antero-posterior view), one from the side (side view), and one from an angle (oblique view).
Anatomy of the foot and ankle
Content:
- Anatomy of the foot and ankle
- Indications for the study
- Preparing for the study and carrying out the procedure
- Getting Results
- Risks of X-rays of the foot and ankle
The feet are a flexible structure of bones, joints, muscles and soft tissues that allow you to stand upright and perform activities such as walking, running and jumping. The forefoot contains five toes (phalanxes) and five longer bones.
The middle of the foot consists of pyramidal bones that form the arches of the legs. These include the three sphenoid bones, the cuboid bone and the scaphoid bone.
The back of the foot forms the heel and ankle. The talus supports the lower leg bones (tibia and fibula) to form the ankle. The heel bone is the largest bone in the leg.
Muscles, tendons and ligaments run along the surfaces of the feet, allowing complex movements to be made. The Achilles tendon connects the heel to the calf muscle and is important when running, jumping and standing on your toes.
The ankle joint allows you to move your leg up and down. The subtalar joint sits below the ankle joint and allows lateral movement of the foot.
Numerous ligaments (made of tough, flexible tissue) surround the true ankle and subtalar joints, connecting the leg bones to each other.
Own muscles and tendons of the foot
Flexor digitorum brevis (FDB)
The muscle starts from the internal (medial) process of the calcaneus and the central part of the plantar fascia. It is attached to all 4 small toes. At the level of the PFJ, each muscle tendon is divided into 2 bundles, each of which goes around the tendon of the long flexor of the finger and is attached to the middle phalanges of 2-5 fingers.
The muscle performs flexion (plantar flexion) of the middle phalanges of the fingers in the PIPJ. As the muscle continues to contract, the proximal phalanges flex at the MCP joint.
Vermiform muscles
These are 4 small muscles starting from the 4 flexor tendons on the foot. The tendon of each lumbrical muscle is attached to the tendon extension of the long extensor muscles on the dorsum of the proximal phalanges of the fingers. Contraction of the lumbrical muscles leads to extension of the fingers in the PIPJ and DIPJ. Because the tendons are located below the point of rotation of the MCP joint, they also perform flexion at these joints.
Indications for the study

Without a doubt, osteoarthritis is the most common foot disease, primarily due to mechanical wear and tear on the cartilage. However, this location is not unusual for inflammatory rheumatic diseases (rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and Reiter's syndrome), often first appearing or being diagnosed in the lower extremities. In addition, gouty arthritis and diabetic neuropathic osteoarthropathy often affect the foot.
Diagnosis of foot tumors using x-rays
In the distal part of the leg, isolated new growths in the bone are sometimes found. Fortunately, most of these growths are benign. For example, a single bone cyst, enchondroma.
Some lesions have characteristic radiographic features. However, some are similar to others and may not be distinguishable by X-ray alone.
To evaluate these lesions, it is necessary to recognize the x-ray characteristics. These data can be used not only as diagnostic clues, but also to determine the rate of growth or aggressiveness of the lesion.
A list of potential differential diagnoses can then be formulated based on these data.
Diagnosis of foot fractures
Medical dictionaries define a fracture simply as the breaking of a bone. However, the doctor must also know the anatomical location of the fracture, its direction, and whether it is linear, crushed, and also distinguish it from a dislocation.
The biomechanics of different fractures may vary, and depending on this, the rate and type of fusion differ.
An x-ray of the foot is the best method for screening and determining the presence of a fracture. X-rays reveal changes that help describe the type of fracture and the position of the bone fragments.
For fractures that are difficult to visualize, additional imaging modalities such as computed tomography or radioisotope skeletal imaging may be required.

Indications for x-rays of the foot and ankle:
- fracture;
- neoplasms;
- flat feet;
- osteoarthritis;
- rheumatoid arthritis;
- psoriatic arthritis;
- Reiter's syndrome;
- ankylosing spondylitis;
- neuropathic osteoarthropathy;
- septic arthritis.
Forefoot fractures and dislocations are usually easy to identify if the potentially damaged bone is completely visible in two planes. The contour of the bony cortex of all bones should be carefully checked.
Dorsal plantar and oblique are the standard projections of the forefoot. If only a phalangeal fracture is suspected, dorsal and oblique views of the fingers can be obtained. Lateral views may also be helpful.
If the patient has such complaints, an x-ray of the foot and ankle may be prescribed:
- periodic pain in the foot area, especially if this pain is not preceded by any physical activity, for example, long walking, prolonged standing of the patient, lifting heavy objects, uncomfortable shoes.
- changes in the appearance of the foot - violation of the size, shape, color of the skin;
- the presence in the patient’s life history of frequent injuries, such as various fractures, dislocations, hematomas, sprains;
- the patient has risk factors for developing diseases associated with the musculoskeletal system, for example, participation in certain sports, obesity, genetic predisposition.
A foot x-ray can help find the cause of common signs and symptoms such as pain, tenderness, numbness, swelling or deformity. It can detect a broken bone or dislocated joint.
Once a bone fracture is determined, x-rays can help determine whether the bones are in the correct position and have healed properly.
If surgery is required, an x-ray may be taken to plan the surgery and evaluate the results of the surgery. X-rays can also help detect cysts, tumors, and advanced bone infections.
Decoding the results
First of all, a radiologist must understand what an x-ray of the foot shows. He does not make preliminary diagnoses, but simply describes the anatomical features of the bones of the foot. The radiologist’s task is to identify fractures, neoplasms, foci of inflammation and other abnormalities. Based on the description of the image, the diagnosis will be made by the attending physician - surgeon, orthopedist, oncologist or others.
Normally, an x-ray of a healthy person’s foot should visualize bones of homogeneous structure, the integrity of which is not compromised. The contours of the bones should be uniform and clear, without darkening.
Symptoms of flat feet

To identify flat feet, an x-ray of the feet is usually performed with a load in the lateral projection. To do this, the foot is placed on a stand with the inside facing the X-ray cassette. The other leg is moved to the side. With this installation, three features are noted in the photographs:
- I – passes from the first toe to the heel bone;
- II – runs from the point of connection of the calcaneus with the first line to the scaphoid-sphenoid joint;
- III - passes from the same joint to the first metatarsal bone.
Correlating these lines, measure the height and angle of their intersection. Height is a perpendicular descended from the point of connection of the second and third lines down to the first horizontal line. Normally, the height should be more than 35 mm, and the angle should be from 125 to 130°.
Deviation from these norms indicates the presence of flat feet. To identify the degree of pathology, you need to assess how much the actual parameters of the foot differ from normal:
- I degree. The height of the arch is 25-35 mm, the angle is 131-140°. With this pathology, the patient is bothered by fatigue in the legs during physical activity.
- II degree. The height of the arch is 17-24 mm, the angle is 141-155°. In this case, the patient feels increased pain with prolonged walking and physical effort.
- III degree. Height – less than 17 mm, angle – more than 155°. With this pathology, the patient constantly feels pain in the legs, lower back and feet.
Injuries and fractures
Fractures and cracks on x-rays of the foot are visualized as small elongated shadows with uneven contours. From the image you need to assess where exactly the fracture line or crack is located, whether there are fragments, and whether they are displaced. To clarify the location of the fracture, in addition to x-rays, an external examination is also performed and the foot is palpated. At the fracture site, when pressed, the patient feels acute pain.
Preparing for the study and carrying out the procedure

X-ray of the foot does not require special preparation. The patient should remove clothing (including shoes), jewelry, or any metal objects that may interfere with the image.
A developing fetus is more sensitive to the effects of radiation than an adult and therefore is at greater risk of harm from X-ray examinations, so if the patient is pregnant, the doctor should be informed.
Although the procedure may take about 15 minutes or longer, the actual radiation exposure is usually less than a second.
The patient enters a special room, which will likely contain a table and a large X-ray machine hanging from the ceiling.
Parents can usually come with the child to ensure peace of mind. Accompanying persons will need to wear a special protective apron to protect certain parts of the body.
The x-ray technician positions the patient both on and off the table to achieve the required position. Then he goes behind the wall, or into the next room to control the machine.
The three x-rays are usually taken from the front, side and angle, so the technician will return to reposition the leg for each new x-ray. Sometimes doctors ask for x-rays of the opposite leg for comparison.
Contraindications for diagnosis
When X-raying the foot, the patient's body is exposed to minimal radiation exposure. Absolute contraindications to x-rays of the feet
does not stand out, but in some cases the appointment must be made with caution. This applies to pregnant women, as well as children under 15 years of age.
How often can you get x-rays of your feet?
To determine how often you can do X-rays of the feet in two projections, you need to know what dose of radiation the X-ray machine produces in one shot. Next, you can refer to SanPiN, which indicates what radiation dose is permissible for the patient annually. By comparing these two parameters, it will be possible to draw a conclusion about the frequency of the diagnostic procedure.
Usually, X-rays are first prescribed when signs of pathology appear. Then they give a second referral after some time (for example, after a month) to assess the effectiveness of treatment. This frequency of x-rays is quite acceptable.
Getting Results
The patient will not feel anything during the x-ray. The x-ray room may be cool due to the air conditioning used to keep the equipment operating properly.
The positions required for x-rays may be uncomfortable, but only need to be held for a few seconds.
If the patient is injured and cannot remain in the required position, the technician may find another position that will be easier for him.
A radiologist is a doctor specially trained in interpreting x-ray images. He will be the one to review the patient's x-rays.
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
After evaluating the results, the radiologist will send a report to the attending physician, who will discuss with the patient what the images show and explain what it means.
In emergency situations, X-ray results can be available quickly. And usually the results are ready in 1-2 days. In most cases, results can be given directly to the patient or family during the examination.
Functional structure of the foot
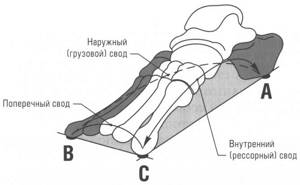
The foot, as a structure, has a rather complex arched shape, reminiscent of a spiral or propeller blade. The foot has an arched structure. It is customary to distinguish between two longitudinal arches and one transverse arch.
Longitudinal bone arches: internal (spring) is formed by the calcaneus, talus, navicular, three wedge-shaped, 1,2,3 metatarsal bones, is an arch that runs through the entire foot, starts from the calcaneal tubercle and ends at the fulcrum of the head of the 1st metatarsal bone;
the outer (cargo) is formed by the calcaneus, cuboid, 4th and 5th metatarsal bones, and also has the shape of an arc that runs through the entire foot, starting from the heel tubercle and ending at the fulcrum of the head of the 5th metatarsal bone.
The vast majority of doctors do not doubt the existence of the transverse fornix, but there are two opinions regarding its localization. First: the transverse bony arch is an arch formed by all the heads of the metatarsal bones. It is located in a plane perpendicular to the arcs of the longitudinal arches. Second: the transverse arch is most clearly expressed in the area of the sphenoid, cuboid and bases of the metatarsal bones.
It is possible to consider the arches of the foot as independent elements only conditionally, since in reality they are in constant interaction and function as a single organ. In maintaining the arched shape of the foot, the leading role belongs to the ligaments, plantar aponeurosis and tendons of the muscles that pass from the lower leg to the foot, and the actual muscles of the dorsal and plantar surfaces of the foot.
The foot is supported at three points: the area of the heel tubercle, the heads of the 1st and 5th metatarsal bones. The pressure between the front and rear support points is normally distributed as 1:4.
Between the bony skeleton of the foot and the supporting surface there are soft tissue structures (muscles, ligaments, subcutaneous tissue, the layer of skin itself), which form the relief of the plantar surface of the foot; numerous vessels and nerves of the foot pass through here. The skin of the plantar area in places of contact with the support has a cellular structure. Fibrous cords are located perpendicularly in it, between which there are areas of adipose tissue, which are good shock absorbers. In the area of support points (heel, area of metatarsophalangeal joints) the skin is denser and resistant to compression.
Features of a child's foot
In children under 3 years of age, the subcutaneous fat layer is significantly developed; it fills the entire niche of the internal longitudinal arch, performing an arch-forming role and the role of a shock absorber.
The ligaments of a child’s foot contain few elastic fibers and a lot of ground substance. The main role in the passive fixation of the arches belongs to the plantar aponeurosis.
Children have wider joint spaces than adults. This makes the joints mobile and reduces the role of the articular surfaces as a passive stabilizer of the arches. Up to 6 years of age, X-rays do not show lines of force in the bones of the foot, which indicates their functional failure and vulnerability. The tarsal bones are not differentiated until the age of 6 years.
Only a doctor can assess the true condition of a child’s feet based on clinical examination data, measurements of foot parameters, and plantography.
It should be noted that in children under 3 years of age, upon examination, this fat pad gives false impressions of a decrease in the size of the soft arch and flattening of the internal longitudinal arch.
How to do a foot x-ray
X-rays are a quick procedure, except in cases where a complex injury prevents the limb from being quickly fixed to obtain an image. There is no need to prepare in any way; it doesn’t matter whether you come on a full or empty stomach. Directly in the office, you will need to take off your shoes, socks, roll up your trouser legs, and for women, remove jewelry from your ankles and toes.
- X-rays of the foot without weight-bearing are usually done in a supine position. The patient is placed on the couch, the examined leg is fixed so that the X-ray beam passes through it at the required angle - usually, projections from below and from the side are chosen.
- X-rays with a load are done standing, in some cases - sitting. The patient is helped to place the leg being examined on a special platform, and then they are recommended to try to transfer their body weight to it so that the image projected onto the photosensitive film more accurately conveys the condition of the bones and joints at the time of walking.
Where to get a foot x-ray in Khimki
We offer X-rays without queues and much cheaper than in Moscow, at our medical center. We are located 50 meters from the Khimki station at the address: Moskovskaya St., 14. The diagnostic room is open seven days a week from 8.00 to 21.00.
Call or use the form on the website to make an appointment at a convenient time. We offer qualified doctors, a comfortable environment, modern equipment and reasonable prices.
Prices for services
| Name | Time | Price |
| Digital radiography of one foot (2 projections) | 1650 | |
| Digital radiography of the calcaneus (2 projections) | 1450 |