Fingers are the main assistants in performing various movements in a person’s daily life. In cases where the injured finger was left without proper care or was treated incorrectly, discomfort can accompany its owner for the rest of his life.
A fractured finger is one of the most common injuries of the upper extremities, resulting from direct mechanical impact (impact) or indirect mechanical impact (severe dislocation or twisting).
Anatomy of the hand
The fingers are located on the hands and perform motor and tactile functions. The fingers consist of short, tubular-type bones connected by tendons. For mobility, muscles and vessels of various shapes are located on the bones.
In their structure, the phalanges of the fingers differ from the phalanges of the toes. The hand contains more than 30 bones and it itself consists of three sections: the wrist, metacarpus and fingers. The wrist consists of 8 bones, the metacarpus of 5. It is worth taking a closer look at the fingers, because this is often the area of the hand that is injured.
There are three types of phalanges:
- Proximal.
- Average.
- Nail.
It is important to note that the thumb does not have a phalanx. Inside the phalanx is the bone marrow.
Causes of fractures
The most common finger injuries occur in people actively involved in sports: boxers, volleyball players, boxers, gymnasts. In cases with boxers, specialized gloves do not always save the day. Children and elderly people suffering from osteoporosis also often suffer such injuries.
Injuries occur, as a rule, during work in production, but often also in the domestic sphere. This injury is not severe, but requires constant proper care and attention due to the importance of the fingers in a person’s life. Often, attempts at self-medication do not end well and lead to sad consequences: in case of severe injuries, complex reconstructive surgeries are performed. The rehabilitation period for such injuries is very long.
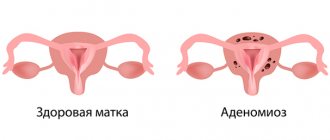
Deformation of the 5th toe: what is it?
It is not for nothing that the deformity of the 5th toe is also called tailor’s foot, because previously such a pathology was most typical for representatives of this profession. Due to a long stay in a forced position with crossed legs and performing monotonous movements, there was a constant load on the outer surfaces of the feet. This led to microtrauma of the bone structures and ultimately deformation of the 5th metatarsal bone. The consequence of this was the curvature of the little finger with the formation of a characteristic protrusion in the area of the metatarsophalangeal joint.
The second name of the disease, Taylor's deformity, comes from the English "tailor", which translates as "tailor".
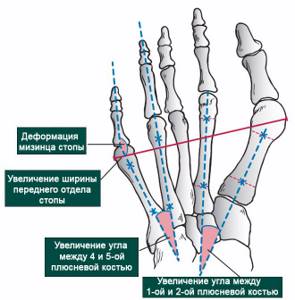
Thus, with Taylor or little toe deformity, the following is observed:
- widening of the forefoot due to an increase in the angle between the 5th and 4th metatarsals;
- an arched bend of the little toe inward, although sometimes a varus subtype of deformity occurs, the presence of which is indicated when the little toe is not turned inward, but when it is applied to the 4th toe;
- the formation of a lump in the area where the foot transitions to the toe. This protrusion is often called simply a bone.
Typically, Taylor's deformity occurs on both feet at the same time, although it can have varying degrees of severity. Moreover, it is often combined with hallux valgus deformity of the 1st toe or Hallux Valgus. As a result, the foot expands abnormally on both sides and the toes become crowded. This provokes the curvature of the fingers located between them and their acquisition of a hammer-like shape.
In any case, such changes in anatomy lead to significant inconvenience not only during active physical activity, but also during quiet walking. And when placing the little finger on the 4th finger, the risk of developing inflammatory processes in the synovial bursae of the interphalangeal and intermetatarsal joints sharply increases. This will contribute to a sharp increase in pain, redness and swelling of the soft tissues in the projection of the affected joints.
There are 3 types of deformation of the fifth toe:
- Type 1 – the head of the 5th metatarsal bone is abnormally widened while maintaining the normal 4-5 intermetatarsal angle.
- Type 2 is a congenital developmental anomaly with curvature of the 5th metatarsal bone against the background of a normal angle between the 4th and 5th metatarsal bones.
- Type 3 – increase in 4-5 intermetatarsal angle. It is this type of deformation that occurs in the vast majority of cases.
Normally, 4-5 intermetatarsal angle should be 6-8°.
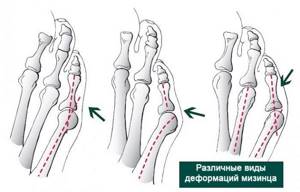
Often the curvature of the little finger is aggravated by its hammertoe deformity. This is especially facilitated by the adverse effects of external factors. But, in addition, the disease without timely treatment can lead to:
- reduction or loss of the ability to flex and extend the finger, which will affect the supporting ability of the foot;
- persistent, painful calluses that are prone to maceration and ulceration;
- purulent bursitis;
- numbness of the skin due to nerve damage;
- decreased quality of life due to severe pain when moving.
Symptoms of a broken finger
The types of finger fractures differ from each other. There are fractures of one phalanx and multiple fractures of several fingers. Determining a fracture is not difficult. With a recent injury, symptoms include the following:
- the finger becomes bluish and swells due to internal hemorrhage and vascular injury;
- very strong and sharp pain in the finger, intensifying with movement;
- in many cases you can see the deformed area with the naked eye;
- the damaged finger is shortened;
- unusual mobility of the phalanx, which has not been noted before;
- inability to fully clench the hand into a fist or fully unclench the hand;
- the appearance of hematomas under the nails, which cause acute pain;
- when you try to move your finger, you hear an uncharacteristic crunch;
- if there is an open fracture, then the victim experiences pain shock and bleeding.
How is a foot x-ray done?
X-rays of the foot are usually performed in two projections:
- Direct - done for a variety of diseases of bones and joints, injuries. The foot stands directly on the receiving device of the device. In such a picture, the bones of the heel and tarsus, the lower part of the lower leg, and the ankle joint will be clearly visible.
- Lateral - in addition to deformations, fractures and pathological changes, such an image will show longitudinal flat feet. The patient turns his leg sideways towards the device.
Less commonly, but an X-ray of the feet is used with an oblique projection - at an angle of 45 0. It is informative for diagnosing the front part of the foot, which may not fit into the image area with a direct or lateral projection.
An x-ray of the foot in two projections is taken with the patient lying or sitting. The leg is tightly fixed to avoid movement and blurred images.
Depending on the expected diagnosis, the doctor may prescribe a stress x-ray. In this case, an x-ray of the foot is also taken in 2 projections, but in a standing position, when there is pressure from the body weight. A study with a load is most informative for flat feet in order to assess the type and degree of deformation and the dynamics of its course.
The resulting images are analyzed by a radiologist, who gives a written report describing the detected pathologies and their features (location, size, structure).
Such a conclusion can become the basis for making a diagnosis. If you need to examine the soft tissues of the foot, your doctor will recommend an ultrasound or MRI of the foot.
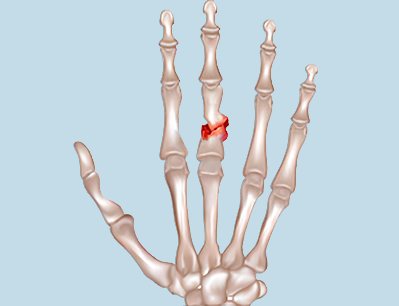
Types of fractures
Open and closed fracture

Closed fractures are very difficult to recognize without the help of a doctor. An open fracture is much easier to see, as it is often accompanied by bleeding. With an open fracture, the integrity of the skin is disrupted. Closed fractures can be complete or incomplete with the presence of cracks.
With and without offset
It is worst to treat displaced fractures, since the bone is fragmented and has many fragments.
The main signs of a displaced fracture are:
- shortening the deformed area of the finger;
- inability to move fingers;
- uncharacteristic mobility of the damaged area in the hand;
- strong pain.
Marginal fracture
This type of fracture concerns the phalanges of the fingers. Patients typically receive this injury in a variety of ways. As a result of the injury, complete or partial destruction of the phalanx of the finger occurs.
Classification of marginal fractures:
- injuries (strong blow, heavy object falling on the arm area);
- pathologies (appear against the background of diseases that cause bone fragility).
According to location, marginal fractures are:
- nails;
- average;
- combined;
- basic.
Index finger fracture
In cases of a fracture of the index finger, you should immediately consult a doctor. He will be able to put the dislocated bone back in place. In case of a dislocation, the doctor will apply a plaster cast to the damaged area. Moreover, traumatologists prescribe special medications to patients to reduce pain. As a rule, there are no complications or problems after a fracture of the index finger.
Fracture of the thumb
Mostly, a thumb injury occurs due to a strong blow. During treatment, certain difficulties may arise due to the special arrangement of the bones.
Such fractures are usually reduced by a doctor. For this purpose, special devices are used that have a stretching effect. After the injured finger is extended, a plaster cast is immediately applied to it, thanks to which the injured finger takes a certain position, and the bones are immobilized until the treatment process is completed.
Child's finger fracture

An injury such as a broken finger in a child occurs much less frequently than in adults and is usually amenable to outpatient treatment. But such injuries should be taken very seriously, since delayed treatment can cause problems with the functioning of the hand.
In order to confirm the diagnosis, it is necessary to take an x-ray and see what type of treatment the doctor will prescribe.
Indications
An orthopedic traumatologist, surgeon, neurologist, or rheumatologist can prescribe an x-ray of the foot.
Main indications:
- Pain in the foot (in any part), at rest, movement or after heavy loads on the foot.
- Limitation of mobility in one of the joints of the foot.
- Swelling, redness of the skin on the foot.
- Swelling, noticeable deformities (for example, crooked fingers, “bone” on the leg).
- Flat feet – reduction of the arch on the sole.
First aid
The victim can receive the highest quality care after contacting specialists immediately after receiving an injury. This range is considered to be a period from one day to 7 days.
Immobilization

If there are rings on your fingers, then for greater convenience it is recommended to remove all the rings from the area of the injured hand. This is done to avoid additional pressure on the fingers and the formation of edema, as well as necrosis of the finger.
Cold is immediately applied to the damaged area, and the hand is placed on an elevated surface. This is also done to prevent swelling.
The limb is immobilized using a splint. In cases where you are very far from a medical facility, the splint is made from available materials (you can use plywood, wood, plastic). The main goal of applying a splint is to avoid secondary injury to the area. If there is an open fracture, then a sterile bandage is applied to the wound, and the place is fixed with a splint.
If there are painkillers nearby and the pain is very strong, then it is recommended to give the victim 1-2 tablets.
X-ray of the hand for bone age
This manipulation is most often carried out in childhood to assess the correspondence of the child’s physical growth and the level of bone development. Thanks to this manipulation, it is possible to exclude developmental delays and a number of endocrinological pathologies. To determine bone age, the results in the image are compared with bone maturation standards using special tables. When assessing bone age, the doctor first of all pays attention to the presence of ossification nuclei and the formation of synostoses.
Possible complications
Complications after a finger fracture can be the following:
Your fingers may go numb. This often happens after the plaster cast is removed. Patients may also note that the hand does not seem to obey them. This is explained by the prolonged immobilization of the fingers at the time of bone fusion after a fracture. As a result, the normal conduction of nerve impulses in the wrist joint is disrupted. Also, at the time of surgery and the injury itself, small branches of the skin nerves may be injured, which also causes numbness. However, after a course of physiotherapy and exercise therapy, these unpleasant symptoms will be removed.
Incorrect healing of the fracture. If the finger does not fuse properly, the following signs are observed: shortening of the length of the finger, limited mobility of the hand. To get rid of this unpleasant phenomenon, the patient is prescribed physiofunctional treatment in combination with reconstruction surgery.
How does a thumb dislocate?
This type of injury is usually recorded in the metacarpophalangeal joint.
. The thumb is characterized by a fairly powerful ligamentous apparatus, but it is worth remembering that even it has a certain load threshold, if exceeded, the ligaments are stretched, and the proximal bone also shifts to the outside or to the back of the hand. The head of the metacarpal bone enters the torn articular capsule, and the proximal bone, in turn, occupies a position of 90 degrees relative to the plane of the capsule.
A dislocated thumb may result from an unfortunate fall.
, when a person lands on an arm extended in front of him with an open palm. A sharp directed blow to the thumb can also cause injury. Such injuries are a common companion for some athletes, such as boxers.
Treatment
The duration of healing of a finger fracture depends on a number of reasons:
- the presence of complications, infections, as well as damage to tendons and ligaments;
- the individual nature of the restoration of bone tissue of a certain person;
- what type of fracture was;
- how quickly treatment was prescribed.
Treatment of finger fractures can be medicinal, conservative or surgical.
Drug treatment
Painkillers and anti-inflammatory drugs are prescribed to the patient without fail. To block pain, the patient is prescribed the following drugs: ibuprofen, diclofenac and others.
For inpatient treatment, these drugs are prescribed intravenously or by injection. After the patient is transferred to home treatment, medications are taken in the form of tablets. Painkillers include analgin, novocaine, and baralgin. They are able to stop painful manifestations, but have no effect on inflammation.
Conservative therapy
With the conservative type of treatment, bone fragments are fused. Everything is done under local anesthesia. After this, the damaged phalanx is fixed with plaster or a bandage. To ensure a strong fixation, the damaged finger can be attached to the neighboring one. Treatment with a bandage is considered more preferable, since air flows better and it is easier to apply.
The cast is removed one month after a displaced injury, but in this case it is worn much longer than with normal non-displaced injuries. The patient is x-rayed several times throughout the treatment. This is done in order to find out whether the bones have shifted. In cases where displacement occurs under a cast, the patient is prescribed surgery.
Surgical therapy
Surgical intervention (osteosynthesis) is prescribed by specialists. With it, the integrity of the bones is restored. At the time of surgery, doctors use various metal materials to fasten the bone fragments to each other. To do this, experts use:
- metal plates;
- screws;
- various knitting needles of different shapes.
Which doctor should I contact?
A traumatologist treats finger fractures. However, in cases of nerve injury during injury, consultation with a neurosurgeon is required.
Is surgery necessary?
For open fractures and displaced fractures, surgical intervention is performed. This is done to avoid repeated displacement. This is done using local anesthesia.
Closed reduction
In a closed type of operation, needles are inserted under the skin. In this case, the recovery process slows down because there is a high risk of infection.
Open reduction
Open reduction (internal fixation) is performed to fix broken bones. The surgical intervention includes two stages: the damaged bone is replaced in its original place. After this, special plates and screws are installed directly on the bone.
Skeletal traction
If the reposition is unsuccessful or there is a high probability of displacement in the plaster cast, soft tissue traction or skeletal traction by the phalanges is performed. The traction frame is attached to a plaster cast, applied to the hand. The traction is removed after 3-4 weeks.
How long to wear a cast for a broken finger
The period of immobilization is always different and mainly depends on the type of injury received. Fractures of the fingers, with or without displacement, are usually fixed with a plaster for 2-3 weeks, and a person can resume normal life within 1 month. For atypical injuries, immobilization is usually performed after 3 weeks, and ability to work is restored after 7 weeks.
What will the examination show?
X-ray of the foot allows doctors to see in the pictures the anatomical features of the structure of the foot, the integrity of the bones, their thickness and structure, the condition of the joints and possible degenerative deformations and pathologies in them (osteophytes and others). X-rays clearly visualize the angle of inclination of the arch of the foot, the width of the joint spaces and other features that are important for diagnosis.
The examination is carried out if there is suspicion of:
- Gout, arthritis, arthrosis and other degenerative-dystrophic, inflammatory and infectious diseases of the joints.
- Osteophytes (heel spurs).
- Foot deformities - change in shape, drooping arches, curvature - flat feet, hallux valgus and others.
- Injuries – bone fractures, dislocations in the foot joints.
- Congenital anomalies of bone structures.
The doctor will also recommend examining the foot in case of ankle injuries, which can lead to foot deformation in the future.
X-rays of the feet allow you to clarify the expected diagnosis, choose the optimal method of treatment and correction, and evaluate the effectiveness of therapy over time. Examination is also necessary for periodic monitoring of patients with chronic diseases.
Rehabilitation
The rehabilitation and recovery period includes:
- a diet that includes foods fortified with calcium and protein;
- physiotherapeutic procedures;
- massage;
- special gymnastics are prescribed in the last week of wearing a plaster cast;
- the patient squeezes a piece of plasticine with his fingers;
- the patient rolls out plasticine with his hand;
- the patient rolls rice in his fingers;
- the use of warming ointments such as “Menovazina”;
- application of compresses with dimexide;
- the use of special salt baths;
- treatment with mud.
Advantages of X-ray diagnostics using digital equipment
The use of low-dose digital equipment has the following advantages, due to which a significant reduction in radiation exposure is achieved in comparison with the traditional film method:
- the process does not involve X-ray film or chemicals;
- the area under study is clearly limited - the beam flow is directed exclusively at the area being examined;
- the exposure time to X-rays required to obtain a high-quality image has been reduced;
- the clarity of the resulting images eliminates the need for repeated radiography due to the lack of information in the resulting image
In the German clinic, thanks to the use of modern equipment manufactured by GE, a reduction in radiation exposure is achieved in comparison with the traditional method of obtaining x-rays by almost 40%. Even the study of infants is permissible using such equipment. The price of an X-ray of the hand using digital equipment is quite affordable.
Physiotherapy
There are several specific requirements for the use of physiotherapy. This treatment method allows you to restore bone tissue and speed up rehabilitation. To do this, it is recommended to do the following:
- Physiotherapy procedures should change over time. The duration of the actions performed is adjusted based on the condition of the bone.
- Procedures must be carried out systematically. Their results will be visible after completing the course.
- There is no need to stop the treatment procedure on your own. In this case, the attending physician does not bear any responsibility for the lack of results.
- Combined procedures. It is allowed to use several physical factors simultaneously or with a short interval.
How long does it take for a broken finger to heal?
The healing process of an injury is very individual and depends on many factors. Firstly, the patient must follow all the recommendations of the attending physician. Secondly, all rehabilitation procedures must be carried out on an ongoing basis. Only by following all the doctor’s instructions and timely assistance can speed up the rehabilitation process.
Any injury is a reason to seek help from a traumatologist. If you self-medicate, the consequences can be disastrous, including amputation of the finger, and in cases of improper fusion, a second fracture may be necessary.
To avoid these consequences, do not self-medicate, but immediately seek help from a specialist. Take care of your health!
Contraindications for
X-rays of fingers are not recommended for pregnant women (especially in the 1st and 3rd trimesters). If possible, it is better to postpone this diagnostic procedure to the postpartum period.
X-rays are also rarely prescribed for patients in serious condition, non-transportable patients.
Caution should be exercised in giving directions for x-rays to children under 15 years of age. X-rays are prescribed only when the potential harm from an incorrect diagnosis significantly exceeds the harm from the influence of ionizing radiation.