08/15/2018 Fluorescein angiography of the retina is a type of contrast X-ray examination, the purpose of which is to visualize blood flow in the organ of vision. The condition of the vessels in the fundus, the anterior chamber of the eye and the choroid are important optical structures. Assessing their condition in medicine is important in both direct and indirect senses.
When is the examination scheduled?
An examination such as angiography may be prescribed by a doctor if the patient has the following indications:
- an ophthalmological examination
revealed primary signs of retinal dystrophy, which are hereditary in nature; - diabetes mellitus caused complications in the eyes (retinopathy);
- there are suspicions of tumors of the vascular membranes of the eye (melanoma, melanocytoma and others);
- blood flow in the vascular system of the retina is disrupted;
- the retina is affected by inflammatory processes;
- there are suspicions of optic disc disease (congestive optic disc, pseudocongestion, neuritis).
What diseases can retinal angiography diagnose?
A research method such as angiography helps to identify the following diseases:
- Thrombosis of the central vein or one of its branches. With this pathology, the veins expand and twist, resulting in retinal swelling and hemorrhages of various sizes. Symptoms of this disorder are pain in the eye, a sharp deterioration in vision (most often in one eye), and flashing lightning.
- Occlusion of the central retinal artery. Symptoms of this pathology are: a sharp decrease in vision, pain and pain in the eye, and the appearance of a veil.
- Vasculitis, accompanied by inflammation of the vessels of the retina. Symptoms: poor vision, twilight blindness, dry eye syndrome.
- Optic nerve atrophy. The main symptom of such a deviation is a decrease in visual acuity, which cannot be restored.
- Retinal tumors – retinoblastoma, melanoma. Complex diseases that also affect visual acuity and eye mobility. In the early stages, they may be amenable to surgical treatment.
- Retinal detachment, rupture or dystrophy.
Material and methods
The study of the state of microcirculation of the bulbar conjunctiva was carried out using our new method of fluorescein angiographic study of the blood circulation PSG, in which contrast is introduced directly into the capillary bed of the bulbar conjunctiva by application [5].
In order to clarify the normal FA picture obtained by this method, 30 individuals (41 eyes) without obvious ophthalmopathology and severe systemic diseases were examined. The age of the subjects ranged from 18 to 70 years (mean age 44.3±2.6 years), among them there were 15 men and 15 women.
To test the possibility of using the method in ophthalmopathology, we formed 2 groups of patients; The 1st group included 10 people (10 eyes) with anterior uveitis, the 2nd group included 9 people (10 eyes) with peripheral uveitis. There were 4 men in the 1st group, 6 women. In the 2nd group there were 6 men, 3 women. The age of the patients in the 1st group ranged from 43 to 57 years (average age 50.5±2.5 years ), in group 2 - from 17 to 29 (average age 22.8±1.4 years).
The choice of these two groups of patients was due, on the one hand, to the proximity of the localization of the inflammatory process in the PSG structures and, to a large extent, the common blood supply to these structures, and, on the other hand, to the previously noted differences in the state of PSG hemoperfusion in these two localizations of the inflammatory process [6]. The latter correlates with the well-known difference in the nature and intensity of the inflammatory process in anterior and peripheral uveitis.
To perform FA using the proposed method, a Topcon Mark II fundus camera (Japan) with installed light filters was used. The shooting was carried out at maximum magnification. The research results were stored in the IMAGEnet R4.0 program database for further processing. A 10% sodium fluorescein solution (Novartis, Switzerland) was used in the work.
In order to unify the results of the study, we chose the optimal area of the bulbar conjunctiva for this purpose - the intermediate capillary zone, located on the border of the prelimb and peripheral zones of the conjunctiva of the eyeball, in the middle third of the distance from the limbus to the fornix [3, 7]. The upper part of the bulbar conjunctiva, normally covered by the eyelid and least susceptible to the influence of environmental factors, was chosen for the study.
The capillary network of the intermediate zone is very rich and is formed by capillaries arising from both the arteries of the peripheral zone and the prelimbal arterioles. Venous outflow, in turn, is also carried out in two directions: to the upper fornix - by peripheral venules and to the limbus - by prelimbal venules.
Overall, this site provides a unique opportunity to study the two blood supply systems of the PSG. One of them is peripheral arterioles and their corresponding venules, which are superficial vessels not directly connected with intraocular blood flow. In relation to prelimbal arterioles and venules, this connection cannot be excluded. It is known that the prelimbal arterioles are rarely visible superficial recurrent branches of the anterior ciliary arteries. They appear at the limbus from subconjunctival tissue [3, 7]. This gives reason to assume their connection with deep vessels and, accordingly, with intraocular blood flow.
To introduce fluorescein into the capillaries of the intermediate zone, an applicator was used, which was a rectangle measuring 1.5 × 10.0 mm, cut from filter paper and soaked in a 10% sodium fluorescein solution and then dried. It was loosely placed on the upper surface of the bulbar conjunctiva, covering enough of the intermediate capillary zone to obtain convincing results. The applicator was firmly held on the surface due to adhesion forces, without exerting a compressive effect on the conjunctival tissue and the capillaries passing through it.
As unified indicators characterizing the microcirculation of the bulbar conjunctiva according to application FA, indicators similar to those used for intravenous FA were chosen, primarily quantitative parameters characterizing the rate of filling of vessels with fluorescein. There was also the possibility of calibrating vessels using the “Ruler” tool built into the IMAGEnet R4.0 program in micrometers. The state of vascular wall permeability was assessed by the presence of extravasal hyperfluorescence, the time of its appearance, and the degree of severity. All indicators were analyzed separately for the peripheral and prelimbal zones. In general, we can talk about the study of the capillary-venular link of local hemomicrocirculation of PSG.
The time parameters were counted from the moment the applicator was placed on the surface of the bulbar conjunctiva. With certain skills, placement takes 1-2 s, which is comparable to the time of fluorescein injection into the cubital vein during “classical” FA.
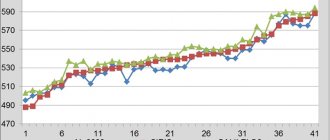
After entering the capillaries of the intermediate zone, the dye spread along the peripheral and prelimbal venules. We called the time from the moment the applicator was placed until the dye appeared in the venules “applicator-venules” (t1).
The next time parameter (t2) characterized the time period from the moment of laying to the maximum filling of the venules in each of the two analyzed zones. Another time parameter (t3) reflected the duration of the venular phase in both zones. It was calculated by the difference between the two previous indicators (t2-t1). The time of onset of extravasal hyperfluorescence was characterized by the t4 parameter. The period of time reflecting any of the moments of FA (except t1, t2, t3, t4) and counted from the moment of placing the applicator was designated as “t”.
Shooting began at 4-5 seconds from the moment the applicator was placed, the interval between frames was 1-2 s during the first 40-45 s, then it became less frequent (1 frame every 10 s). By analogy with intravenous FA, recording was carried out for up to 3 minutes.
How is the procedure done?
To conduct the examination, the patient must sit facing the camera. A special solution is instilled into his eyes, which promotes maximum pupil dilation. The patient then places his chin on the rest so that his forehead rests on the bar, his jaw closes completely, and his gaze is directed straight ahead.
Next, a contrast agent is injected into the patient’s vein and X-rays are taken simultaneously. In order for the images to be of high quality, the patient needs to sit motionless, in a relaxed state throughout the entire procedure and, of course, not blink.
When the doctor moves on to photograph the periphery of the eye, he asks the patient to shift his gaze to the desired direction.
As soon as the contrast begins to enter the vein, the doctor produces a series of photographs consisting of 25-30 frames. On average, 1 photo is taken per 1 second. After stopping the medication, the needle is removed from the vein, and a tight bandage is applied to prevent bleeding.
When the doctor needs to clarify some details, the examination can be repeated 20 minutes after the contrast is administered. There is no point in doing this later - the pictures will be uninformative.
4.What can affect angiography?
Cataracts, severely dilated pupils, and an inability to keep your head up or your eyes open may interfere with angiography.
Things to know
It is not recommended to undergo angiography during pregnancy, especially in the first three months. Breastfeeding mothers will not be able to breastfeed their baby for 24-48 hours after angiography, because the dye will pass into breast milk. Therefore, if you have excess breast milk, it is recommended to store it in the refrigerator for such an occasion.
After the test, your urine may be bright yellow or orange due to the dye. After an angiography, you may have blurred vision due to droplets. This will pass the next day.
Advantages and disadvantages of retinal angiography with fluorescein
The main advantage of retinal angiography with fluorescein is its high sensitivity and information content. Even the smallest capillaries of the eye are subject to evaluation. Changes in the pigment epithelium and optic disc are also detected, and choroidal neovascularization can be seen.
Contraindications for the study
Before starting to study the fundus using angiography, the doctor should carefully analyze possible contraindications to such a procedure:
- Low transparency of the eyeball environment. The contraindication is due to the fact that the pictures will most likely turn out dark and uninformative, so there is simply no point in the procedure.
- Inability to fully dilate the pupil (may be caused, for example, by glaucoma). As in the previous case, the picture will turn out blurry.
- Asthma, kidney disease, inflammatory vein diseases.
- Coronary heart disease, stroke, myocardial infarction (if it happened less than a year ago).
- Allergy to contrast.
- Children's age (up to 14-15 years), as well as the elderly (over 65 years).
- Mental disorders, epilepsy.
Diagnostic capabilities
Only a specialist in this field can interpret the results of fluorescein angiography. If you have the necessary experience, a doctor can determine a number of diseases using research:
- Arteriovenous shunt;
- Microaneurysm;
- Occlusion of a vein or artery, often accompanied by the formation of collaterals or recanalization;
- Neovascularization;
- Swelling in the area of the inflammatory process;
- Hemangiomas and aneurysmal vasodilatations;
- Signs of hypertensive retinopathy, in which there are microaneurysms around ischemic areas;
- Tumor growths with an atypical vascular pattern.
Not all patients with eye disease need fluorescein angiography. There are indications for this study:
- Monitoring the dynamics of the disease and the effectiveness of treatment;
- Diagnosis of the exact location of vascular pathology and determination of its extent;
- Determination of indications for laser coagulation of the retina;
- Clarification of the diagnosis and differential diagnosis of pathological foci in the retina.
This technique also has a number of contraindications:
- Reduced transparency of the light-transmitting media of the eyeball;
- The presence of diseases (pseudophakia, glaucoma) that do not allow performing medicinal mydriasis, which is necessary for fluorescein angiography;
- General somatic diseases (thrombophlebitis, renal failure with impaired excretory function, bronchial asthma);
- A history of cerebrovascular accident (ischemic or hemorrhagic type);
- Acute and subacute stage (during the first year) of myocardial infarction;
- Allergic reactions to drugs, especially radiopaque agents, antibiotics, mydriatics;
- Children's (up to 15 years) and elderly (over 65 years) age of patients;
- The presence of mental disorders and episyndrome.
Nursing mothers should stop breastfeeding for at least two days after fluorescein angiography. It is possible to conduct a test during pregnancy. Side effects after performing FA are not common and include:
- Skin itching and urticarial rash;
- Paresthesia of the tongue;
- Weakness, dizziness;
- Sneezing;
- Vomiting, nausea.

Are there possible complications during the procedure?
In some cases, the response to contrast injection may be nausea or a feeling of heat. These are temporary symptoms, they are harmless and go away fairly quickly.
If the body’s reaction turned out to be more serious - vomiting, a metallic taste appeared in the mouth, dizziness, a rash similar to hives appeared on the body - then prompt measures must be taken to eliminate such symptoms. It is possible that resuscitation measures will be required.
Within 2 days after the diagnosis, the patient may have a changed color of urine and skin. Such symptoms persist until the contrast is completely removed from the body.
Also, in the first 12 hours after the examination, the patient may notice that he cannot focus on close objects. During this period, you need to reduce the strain on your eyesight and protect your eyes from bright light.
Side effects of the procedure
The FA study can cause a number of side effects, including mild dizziness or weakness, nausea (up to 5% of cases), allergic rashes and itchy skin, sneezing, numbness of the tongue, vomiting (no more than 1% of cases). All of these side effects are reversible and, as a rule, do not require medical attention.
In very rare cases, the procedure may be accompanied by more serious complications (anaphylactic shock, respiratory arrest, disruption of the cardiovascular system, etc.), requiring emergency resuscitation measures. That is why the diagnostician and the nurse who administers the contrast must be trained to recognize dangerous symptoms of complications in a timely manner and must be able to carry out the necessary resuscitation measures.
Decoding the results
Images taken during the early stages of contrast administration show microaneurysms, arteriovenous shunts, and neovascularization. Signs such as slow or complete absence of arterial blood flow, stenosis, or slow emptying of the veins indicate arterial occlusion.
If the images reveal areas of large tortuous vessels, microaneurysm can be traced in areas where capillary perfusion is not observed, we can talk about the presence of hypertensive retinopathy.
There are other markers of fundus diseases. an experienced ophthalmologist can accurately recognize them and make a correct diagnosis.
.
conclusions
1. The data obtained using the proposed method of non-invasive application of FA reflect the state of hemomicrocirculation in the capillary-venular link of the bulbar conjunctiva.
2. In patients with anterior uveitis in the acute stage of the disease, signs of hyperhemoperfusion of PSG in combination with a pronounced increase in vascular permeability were revealed.
3. In patients with peripheral uveitis, along with increased vascular permeability, signs of PSG hypohemoperfusion were noted.
4. The proposed method of non-invasive application of FA PSG can be used to control the course of the inflammatory process in anterior and peripheral uveitis.