Radiography is a radiation diagnostic method, accessible and informative, allowing one to examine the condition of the bone skeleton and its pathological changes. This is an integral part of diagnosis for injuries, degenerative, destructive processes and inflammation.
It is important to know the condition of the hand joints:
- To identify the cause of the disease;
- Determine the stage of its development;
- See which joints undergo changes.
The study is recommended for diagnosing pathologies - fractures, dislocations, joint diseases, arthrosis and rheumatoid arthritis.
How is the procedure performed?
No special preparation required.
- Metal decorations should be removed, as their presence negatively affects the quality of the image.
- To protect against radiation, the patient wears a special lead apron. If the diagnosis is performed on a child, then only the area being diagnosed is left open.
- During the X-ray, the patient sits with his arm bent at the elbow.
- The brush is placed on a special cassette, fingers together. It is important that the hand is on the same axis with the wrist and forearm. As a rule, x-rays are performed in frontal and lateral projections, unless there are special requirements.
The only contraindication is pregnancy. X-rays take a few minutes.
Advantages of using the method
Diagnostics allows:
- Recognize changes in the early stages;
- Make the correct diagnosis;
- Provide timely treatment.
X-ray radiation in small doses can be beneficial for the body, as it has a therapeutic effect. According to medical statistics, dosed radiation improves the condition of patients with arthrosis. X-ray therapy allows you to stop the inflammatory process and pain in the joints. Radiation therapy is an effective treatment method for joint pathologies.
X-ray of the ulna and radius in two projections 1000 X-ray of the wrist joint in two projections 1000
+7 (495) 320-43-41
Radiation anatomy of the wrist joint
Radiation anatomy of joints
- X-ray anatomy of the wrist and hand
- Normal hand anatomy
- MRI anatomy of the hand
- Ultrasound anatomy of the hand and wrist joint
- Radiation criteria for the normal wrist joint
X-RAY ANATOMY OF THE RADIAL JOINT AND HAND
The anatomical structure of the bones that form the wrist joint and the skeleton of the hand is relatively simple. The glenoid cavity of the wrist joint is formed by the carpal surface of the distal epiphysis of the radius and the triangular cartilage (disc) attached to the styloid process of the ulna. The articular head of this joint is formed by a complex of bones of the proximal row of the wrist. The distal epiphysis of the radius is relatively flat; at its radial edge there is a styloid process. The frontal size of the epiphysis is significantly larger than the sagittal one. On the ulnar surface of the distal metaepiphysis of the radius there is a slightly concave cylindrical surface for articulation with the head of the ulna (the glenoid cavity of the distal radioulnar joint). The head of the ulna has a rounded shape; on the ulnar side there is a styloid process.
In the proximal row of carpal bones there are 4 bones, of which the wrist joint includes the scaphoid, lunate and triquetrum. The proximal surfaces of all three bones are convex, while the distal surfaces of the first two are concave. The longitudinal axis of the scaphoid is deviated from the frontal plane in the dorsal direction at an angle of approximately 30°, the longitudinal axis of the lunate coincides with the sagittal plane. There is a distinct tuberosity on the dorsal surface of the scaphoid. The concave distal surfaces of the bones of the proximal row of the wrist together form the glenoid cavity of the intercarpal joint. The head of this joint is represented by a complex of convex proximal surfaces of the hamate, central bones, trapezium bone and trapezoid carpal bones. The metacarpal bones and phalanges of the fingers have the structure of tubular bones. The articular surfaces of the proximal epiphyses of these bones are moderately concave. The carpometacarpal joints are flat, with little range of motion; the metacarpophalangeal and interphalangeal joints are a type of block joint with predominant mobility in the sagittal plane (except for the joints of the first finger).
X-ray criteria for anatomical and topographic relationships
On a radiograph in the palmar projection, the following is assessed: in the wrist joint - the uniform height of the radiographic joint space between the articular surfaces of the epiphysis of the radius on one side and the scaphoid and lunate bones of the wrist on the other, as well as the location of the center of the articular surface of the lunate at the level of the distal radioulnar joint . In the distal radioulnar joint, the adjacent edges of the proximal surfaces of the radius and ulna are located at the same level and the width of the x-ray joint space is uniform. In the intercarpal joint, there is a uniform width of the x-ray joint space and the location of the middle of the articular surface of the central bone of the wrist at the level of the gap between the lunate and scaphoid bones. In the metacarpophalangeal and interphalangeal joints there is also a uniform width of the x-ray joint space and, in addition (subject to correct placement during x-ray), the location of the centers of the articulating articular surfaces at the same level.
On an x-ray in a lateral projection, the criterion for the correctness of the anatomical relationships in the wrist joint is the uniformity of the height of the arcuate x-ray joint space, as well as the coincidence of the location of the centers of the articular surfaces of the epiphysis of the radial and lunate bones of the wrist (provided the x-ray is performed in the middle position of the hand). In the joint between the central and lunate bones, the correctness of the anatomical relationships is also evidenced by the uniformity of the width of the x-ray joint space and the coincidence of the articular surfaces of the articulating bones.
Stages of ossification of the bones of the hand and wrist joint
In the process of enchondral bone formation of this part of the osteoarticular system, three periods can be distinguished:
- - first period - before the appearance of the first centers of ossification of anatomical formations that have a cartilaginous structure at the time of birth;
- - the second period, lasting 12 years, is the period of ossification of the epiphyses of the tubular bones of the forearm and hand and the bones of the wrist;
- - third - final - period of synostosis of metaepiphyseal growth zones.
Age up to 4 months. The distal metaepiphyses of the bones of the forearm and bones of the hand retain the degree of ossification achieved by the end of intrauterine development. During this period, the epiphyses of the short tubular bones of the hand and forearm bones, as well as all the bones of the wrist, have a cartilaginous structure.
From 4 months to 2 years (Fig. 19.42). The centers of ossification of the two carpal bones - the capitate and hamate - and the ossification nucleus of the distal epiphysis of the radius appear. The age for the onset of ossification of the carpal bones is 4 months, the epiphysis of the radius is 9-12 months.
Rice. 19.42. X-ray of the wrist joint (6 months).
Ossification centers can be traced only in the capitate and hamate bones. 1 - capitate bone; 2 - hamate bone.
Rice. 19.43. X-ray of the wrist joint (3-4 years).
Ossification nuclei can be traced in: 1 - capitate bone; 2 - hamate bone; 3 - triangular bone; 4 - lunate bone; 5 - distal epiphysis of the radius; 6 - epiphyses of the carpal bones; 7 - epiphyses of the proximal phalanges of the fingers.
During the same period, the metaphyses of the short tubular bones of the hand and forearm bones become ossified.
The criterion for the correctness of the relationships in all of these joints are: in the middle position of the fingers - the location of both (medial and lateral) edges of the metaphysis of the distal bone at the level of the same edges of the metaphysis of the proximal bone; with radial or ulnar deviation of the fingers - coincidence of the edges of the metaphyses of the articulating bones only on one side, on the one in which the finger is deviated (with radial deviation - coincidence of the radial edges of the metaphyses, with ulnar deviation - the ulnar edges).
2 years. Age of onset of ossification of the metacarpal bones and phalanges. Due to the independent center of ossification in these bones, only one epiphysis ossifies: in the metacarpal bones - distal, in the phalanges of the fingers - proximal. The only exception is the first metacarpal bone, in which the center of ossification has a proximal epiphysis. The sometimes observed ossification nuclei of the proximal epiphyses of other metacarpal bones, designated by the term “pseudoepiphyses,” are considered as a variant of the norm
At 3 years of age, the center of ossification of the third carpal bone, the triquetrum, appears.
At 4 years of age, the lunate bone of the wrist begins to ossify (Fig. 19.43, 19.44).
From 4.5 to 7 years, the main manifestation of enchondral bone formation of the wrist joint and hand is the beginning of ossification of the three bones of the wrist - the scaphoid, trapezoid and trapezoid bones. The beginning of their ossification does not have such exact age dates as the four carpal bones mentioned above. We can only note that in most cases the following sequence of appearance of ossification centers in them is observed: first the center of ossification of the trapezium bone, then the scaphoid bone, and lastly the trapezoid bone (Fig. 19.45, 19.46).
Rice. 19.44. X-ray of the wrist joint (4.5 years - 5 years).
1 - epiphysis of the base of the 1st metacarpal bone.
Rice. 19.45. X-ray of the wrist joint (6 years).
1 - ossification nucleus of the trapezium bone.
By the age of 7 years, the cartilaginous structure is preserved by: the marginal sections of the bones of the wrist, the apex of the styloid process of the radius and the head of the ulna along with the styloid process.
At 8-9 years of age, the main manifestation of enchondral bone formation during the period under review is ossification of the head of the ulna. The first stage of this process is the appearance of a center of ossification of the cartilaginous model of the head itself (Fig. 19.47). In parallel, over the course of several months, an ossification nucleus of the styloid process appears.
Rice. 19.46. X-ray of the wrist joint (6-7 years).
1 - ossification nucleus of the scaphoid.

Rice. 19.47. X-ray of the wrist joint (8-9 years).
1 - trapezium bone; 2 - trapezoid bone; 3 - epiphysis of the ulna.

Rice. 19.48. X-ray of the wrist joint (10-11 years).
1 — tubercle of the epiphysis of the ulna (styloid process).
Ossification of most of the head of the ulna and fusion of the styloid process with it occurs on average at 9 years. In parallel with the ossification of the head of the ulna, the degree of ossification of the carpal bones increases, up to complete ossification, which occurs by 10 years. The cartilaginous structure at the end of the age period under consideration is preserved by: the pisiform bone of the wrist, a small part of the head of the ulna, the sesamoid bone of the first metacarpophalangeal joint and the metaepiphyseal growth zones of the short tubular bones of the hand and the bones of the forearm.
At 10 years of age, the center of ossification of the pisiform bone of the wrist appears.
At this age, it is possible to analyze all radiological indicators of the anatomical structure of the wrist joint and hand (Fig. 19.48).

Rice. 19.49. X-ray of the wrist joint (12-13 years).
a - palmar projection: 1 - pisiform bone.
b — lateral projection: 1 — epiphysis of the radius; 2 - styloid process and epiphysis of the ulna;
3 - scaphoid bone; 4 - trapezium bone; 5 - lunate bone; 6 - capitate bone; 7 - I metacarpal
bone.
The age of 12-14 years corresponds to the final stage of postnatal formation of the wrist joint and hand skeleton (Fig. 19.49). An indicator of the onset of this stage is the ossification of the sesamoid bone of the metacarpophalangeal joint of the first finger (at the age of 12 years) and the onset of synostosis of the metaepiphyseal growth zone of the first metacarpal bone (the average age is 14 years). Synostosis of this growth zone occurs earlier than synostosis of the metaepiphyseal and apophyseal growth zones of all other bones of the skeleton and is considered a sign of the impending cessation of bone growth.
All radiological indicators of the anatomical structure of a given section of the osteoarticular system are available for X-ray analysis, without exception.
Normal hand anatomy
The eight carpal bones can be functionally divided into a proximal row (scaphoid, lunate, triquetrum, pisiform) and a distal row (trapezium, trapezoid, capitate, hamate). The pisiform bone is a variant of the sesamoid bone located in the flexor carpi ulnaris tendon and articulates with the triquetrum bone. The connection between the distal articular surface of the radius, ulna, triangular articular disc and proximal row of carpal bones forms the radiocarpal joint. In 15% of cases, this joint communicates with the pisiform-triquetral joint. The proximal and distal rows of carpal bones form the intercarpal joint. The distal row of carpal bones and the base of the metacarpal bones form the carpometacarpal joint, which is immobile due to the strong ligamentous apparatus (amphiarthrosis). The joints between the bases of the metacarpal bones are known as intermetacarpal joints. The carpometacarpal joint of the first finger and the distal radioulnar joint are distinguished separately. The articular surface of the radius is concave and forms a sigmoid notch for the ulna.
The anatomical structure of the ligamentous apparatus of the wrist is very complex. There are interosseous ligaments (between the bones of the wrist), which are partially attached to the internal joint capsule and are like internal ligaments, and extracarpal ligaments, which strengthen the joint capsule from the outside (external ligaments of the wrist).
Internal ligaments. The proximal row of carpal bones connects the interosseous ligaments (the scapholunate ligament between the scaphoid and lunate and the lunate-triquetral ligament between the lunate and triquetrum), forming a functional unit. These ligaments demarcate the wrist and intercarpal joints and prevent their communication (Fig. 19.50).
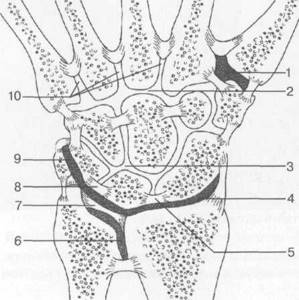
Rice. 19.50. Joints and interosseous ligaments of the wrist area.
1 - I metacarpal joint (I finger); 2 - common metacarpal-carpal joint; 3 - proximal intercarpal joint; 4 - wrist joint; 5 - scapholunate ligament; 6 - distal radioulnar joint; 7 - triangular (ulnar) disc; 8 - lunate-triquetral ligament; 8 - lunate-triquetral ligament; 9 - triquetral pisiform ligament; 10 - intermetacarpal spaces.
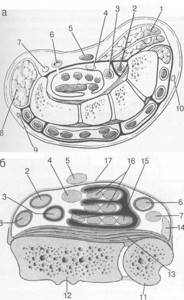
Rice. 19.51. Tendons of the wrist joint.
a - palmar surface at the level of the wrist bones: 1 - m. abductor pollicis brevis; 2 - tendon of the t. flexor carpi radialis; 3 - tendon of the t. flexor pollicis longus; 4 - nervus medianus; 5 - tendon of t. palmaris longus; 6 - arteria ulnaris; 7 - palmar branch n. unaris; 8 - m. abductor digiti minimi; 9 - dorsal branch n. unaris; 10 - superficial branch of n. radialis.
b - at the level of the wrist joint along the palmar surface: 2 - tendon m. flexor carpi radialis; 3 - tendon of the t. flexor pollicis longus; 4 - n. medianus; 5 - tendon of t. palmaris longus; 6 - a. ulnaris; 7 - n. ulnaris; 11 - ulna; 12 - radius; 13 - m. pronator quadratus; 14 - tendon m. flexor carpi ulnaris; 15 - tendon m. flexor digitorum profundus in the synovial vagina; 16 — tendon mm. flexor digitorum superficialis in the synovial vagina; 17 - lig. carpalis palmaris; 18 - a. radialis.
Like all ligaments, they are also subject to degenerative changes and damage. Thus, defects of the scapholunate and lunate-triquetral ligaments occur in 30% of elderly people who do not complain. The distal row of bones is also connected by interosseous ligaments. The shape of the arrangement of the interosseous ligaments and the ulnar disc contributes to the formation of various parts of the articular cavity. External ligaments. The entire wrist area is covered by a dense fibrous capsule, partially reinforced by strong ligaments. On the palmar side runs the radiocapitate ligament, which is part of the palmar radiocarpal ligament. It runs from the styloid process of the radius above the scaphoid to the capitate. The radiotriquetral ligament is also part of the palmar radiocarpal ligament. It starts from the styloid process of the radius and goes in an oblique direction, crosses the lunate bone and joins its fibrous fibers (in particular, the palmar radiocarpal ligament). On the ulnar surface of the palmar-carpal region, fibrous fibers begin from the styloid process of the ulna and form a triangular fibrocartilaginous complex. These ligaments, together with the radiopalmar ligaments, form a V-shaped figure and are known as the proximal and distal V-ligaments.
On the dorsal surface there are two powerful diagonal ligaments. The proximal ligament running from the styloid process of the radius above the lunate to the triquetrum is called the dorsal radiotriquetral ligament and is the dorsal component of the ligamentous attachment of the carpus. The triquetrum is the bony basis of this attachment. From the triquetral bone, wide fan-shaped fibrous fibers are stretched to the other bones of the distal row of the wrist and to the trapezium bone. They are called the dorsal carpal ligament. The radial and ulnar collateral ligaments are visible on the corresponding sides of the carpal region (Fig. 19.50).
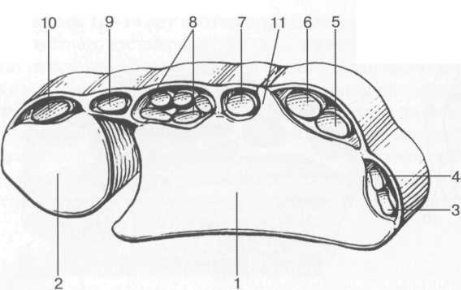
Rice. 19.52. Tendons of the wrist joint along the dorsal surface (each group in its own synovial sheath).
1 - radius; 2 - ulna; 3 - tendon m. extensor pollicis brevis; 4 - tendon of the abductor pollicis longus; 5 - tendon of the t. extensor carpi radialis brevis; 6 - tendon of the t. extensor carpi radialis longus; 7 - tendon of the extensor pollicis longus; 8 - tendon extensor digitorum communis et mm. extensor indicis proprius; 9 - tendon t. extensor digiti quinti; 10 - tendon of the t. extensor carpi ulnaris; 11 - Lister's tubercle of the radius.
The triangular articular disc is a fibrocartilaginous plate located between the distal ulna on one side and the triquetrum and lunate bones on the other. It is triangular in shape and arises from the hyaline cartilage of the distal articular surface of the radius, smoothly passing into the fibers and ligaments stretched between the styloid process of the ulna and the proximal row of carpal bones. Two bundles of fibers, starting from the ulna in two places: from the styloid process of the ulna and from the base of the distal end of the ulna, slide over the distal surface of the head of the ulna, covered with hyaline cartilage. The ulnar component of the wrist joint is located distal to the triangular disc. The central and radial part of the disc is practically not vascularized compared to the ulnar part. Due to good vascularization, the ulnar part of the disc has a high IS on T1- and T2-weighted images. Because the multiple fibrous structures of the ulnar wrist are difficult to separate on images, the triangular disc and ligamentous complex are called the triangular fibrocartilaginous complex. In addition to the disc, this complex includes the dorsal and volar radioulnar ligaments - fairly variable ligamentous structures between the triquetral and ulna bones, designated as the ulnocarpal meniscus, the ulnar collateral ligament, two ulnocarpal ligaments, the ulnolunate ligament and the ulnar triquetral ligament.
The ulnocarpal meniscus may contain an additional small bone called the os triquetrum secundarium or os triangulare.
The wrist joint undergoes flexion and extension, as well as radial and ulnar abduction. Flexion occurs more at the wrist joint, and extension occurs at the intercarpal joint. The scaphoid bone noticeably changes its position with ulnar and radial abduction. With radial abduction, this is usually a 45-50″ tilt to the palmar side relative to the longitudinal axis of the beam with abduction to the radial side. In ulnar abduction, it becomes straighter and occupies the area between the distal surface of the radius, the trapezium bone, and the trapezius bone.
The interphalangeal joints of the hand are located between the adjacent phalanges of each finger. The ligamentous apparatus of the interphalangeal joints of the hand is represented by palmar ligaments, which come from the lateral surfaces of the blocks and are attached: one to the lateral surface of the phalanges - the lateral ligaments, and the other to their palmar surface. The thumb has one interphalangeal joint.
Table 1 9.6. Tendons of the wrist joint and their location
| Dorsal tendons | Localization | |
| 1. Extensor pollicis brevis Abductor pollicis longus | Outer surface of the radius | |
| 2. Extensor carpi radialis longus Extensor carpi radialis brevis | Dorsal-external surface of the radius | |
| 3. Extensor pollicis longus | Dorsal central surface of the radius | |
| 4. Extensor digitorum Extensor indicis | Dorsal-ulnar surface of the radius (they have a common synovial bursa) | |
| 5.Extensor digiti minimi | Dorsal surface of the ulna | |
| 6. Extensor carpi ulnaris | Dorsal-ulnar surface of the ulna | |
| Palmar tendons | Localization | |
| 1. Flexor carpi ulnaris (p. ulnaris, a. ulnaris) | External volar-ulnar surface of the ulna | |
| 2. M. pronator quadratus | Covers the radius and ulna bones, located deep | |
| 3. Flexor digitorum superficial | Centrally, two - superficially, two - deeper below them, directly under the palmar carpal ligament | |
| 4. Flexor digitorum profundus | Directly below the superficial flexors. Four on one line in the area of the ulnar bursa. | |
| 5. Palmaris longus (n. medianus) | Central, radially offset from the superficial flexors, superficial to the palmar carpal ligament Directly beneath the tendon and palmar ligament | |
| 6. Flexor carpi radialis Flexor pollicis longus (a. radialis) | Along the volar-radial surface of the radius directly under the palmar ligament In the bursa radialis under the flexor carpi radialis Outward from the tendons | |
The muscle tendons, passing in the canals of the hand, are surrounded by synovial sheaths containing several tendons. The tendons of the wrist joint are divided into the palmar group and the dorsal (or dorsal) group of tendons. The palmar group includes a group of flexor tendons, and the dorsal group includes extensor tendons. The palmar group is located primarily in the carpal tunnel or carpal tunnel. The dorsal group is divided into 6 subgroups - pockets, in accordance with their location in relation to the bones of the wrist joint (Table 19.6, see Fig. 19.51; Fig. 19.52).
On the dorsum of the wrist there is a wide reinforcing fibrous cord - extensor retinaculi, which consists of several ligaments that form six pockets, or sections, each of which has a synovial sheath for the extensor tendons of the hand passing there (see Fig. 19.50). The first pocket, located near the styloid process of the radius, contains the fibers of the abductor tendon and the extensor digitorum brevis tendon. The extensor carpi radialis longus and brevis tendons lie in the second recess, lateral to the dorsal tubercle of the radius. The third pouch, medial to the dorsal tubercle, contains the extensor digitorum longus tendon. The fourth pocket contains the extensor tendons of the fingers and the extensor of the index finger. The fifth pouch contains the extensor tendon of the little finger; in the sixth pocket - extensor carpi ulnaris.
On the inner or palmar side of the wrist there is also a reinforcing fibrous cord, only the flexor tendons of the hand - flexor retinaculi, which forms the carpal tunnel (see Fig. 19.52). This fibrous cord is attached medially to the pisiform bone, laterally to the hamate bone, where it is divided into two layers, attached to the tubercles of the scaphoid and trapezius bones. The flexor carpi radialis tendon is located between two layers of fibrous cord, where the deep and superficial flexor digitorum tendons, the flexor digitorum longus tendon and the medial nerve pass. The flexor digitorum longus tendon runs closer to the radial surface of the canal and has its own synovial sheath. The other eight flexor tendons are enclosed in a common tendon sheath (see Fig. 19.51).
The medial nerve passes through the carpal tunnel lateral and superior to the digital flexor tendons. The flexor carpi ulnaris tendon is located medial to the ulna and is encased in a synovial membrane. Between the flexor digitorum tendons and the flexor carpi ulnaris tendon are the ulnar artery and nerve. The superficial flexor tendons of the fingers are attached to the proximal part of the middle phalanx of the fingers. The deep digital flexor tendons attach to the base of the distal phalanx. The finger flexor tendons are fixed to the phalanges with the help of annular (or anular) ligaments.
MRI anatomy of the hand
The coronal plane is the standard plane for visualizing the hand (Fig. 19.53). Bone marrow of the carpal bones, especially the lunate and scaphoid, can be easily assessed as a homogeneous high-intensity signal on T1-weighted images. A point decrease in signal intensity may correspond to compact bone “islands”, small cysts and feeding vessels. Uniformly high signal intensity reflects the absence of hematopoietic bone marrow in the distal limbs. The interosseous scapholunate and lunatetriquetral ligaments are not always visualized on coronal sections. Because the lunate triquetrum ligament is slightly smaller, it is less frequently visualized than the scapholunate ligament.
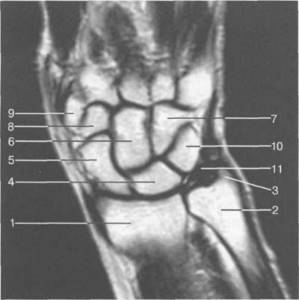
Rice. 19.53. MRI of the wrist joint and carpal bones (coronal plane).
1 - radius bone; 2 - ulna; 3 - styloid process of the ulna; 4 - lunate bone; 5 - scaphoid bone; 6 - capitate bone; 7 - hamate bone; 8 - trapezoid bone; 9 - trapezium bone; 10 - triquetral bone; 11—triangular disk.

Rice. 19.54. MRI of the wrist and hand in the axial plane.
a — level of the wrist joint: 1 — radius; 2 - ulna; 3 - group of the palmar surface of the tendons; 4 - group of the dorsal surface of the tendons.
b — level of the carpal bones: 1 — hamate bone; 2 - capitate bone; 3 - trapezoid bone; 4 - trapezium bone; 5 - group of flexor tendons; 6 - n. medianus; 7 - group of extensor tendons.
c — level of metacarpal bones: 1 — I metacarpal bone; 2 - II metacarpal bone; 3 - III metacarpal bone; 4 - IV metacarpal bone; 5 - V metacarpal bone; 6 - tendon m. flexor pollicis longus; 7 - palmar aponeurosis; 8 - flexor tendons; 9 - n. medianus; 10 - m. abductor digiti munimi; 1 1 - m. abductor pollicis brevis.
These ligaments do not occupy the entire intercarpal space, but are located mainly along the peripheral part of this zone. Therefore, on coronal sections they can be traced at the level of the wrist joint, and not at the intercarpal joint. As for the remaining intercarpal joints, their space is filled with hyaline cartilage of the articulating bones.
There are different attachments of the scapholunate ligament to the hyaline cartilage of the scaphoid and lunate bones. Most often, it is widely attached to the proximal articular surface of the lunate. The capsular ligaments, fibrocartilaginous disc and interosseous ligaments are characterized by low image signal intensity in all types of suspension. These fibrocartilaginous structures may have various deviations in the form of an “artificial” increase in IS on T1 and T2 WI and Pd images. At certain joint positions
Artifacts appear that simulate hyperintense zones in these structures (the “magic angle” effect). Many articles describe cases of increased IS from the scapholunate and triquetrum ligaments, detected in patients who do not complain, and which are a manifestation of degenerative changes. These signal changes can be pointwise or linear and are located both along the ligament and at the site of bone attachment. There are several options for increasing IC: triangular, linear and amorphous.
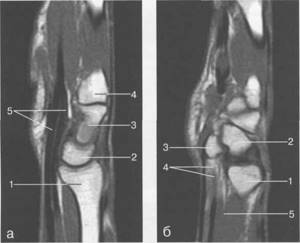
Rice. 19.55. MPT of the wrist joint in the sagittal plane.
a - through the plane of the radius: 1 - radius; 2 - lunate bone; 3 - capitate bone; 4 - base II! metacarpal bone; 5 - tendon m. flexor digitorum profundus et superficialis. 6 - through the plane of the pisiform bone: 1 - radius; 2 - triquetral bone; 3 - pisiform bone; 4 - tendon m. flexor digitorum profundus et superficialis; 5 - t. pronator quadratus.
Degenerative age-related changes in the ulnar disc usually appear after age 30. They are characterized by a zone of high intensity, which must be differentiated from rupture or inflammation. Histological studies of these areas revealed a small number of chondrocytes, reflecting changes in the fibrous matrix. On 71- and T2-weighted images a focal and linear increase in signal intensity is visualized. A linear increase in signal intensity extending to the articular surface usually corresponds to a complete old tear. These degenerative changes progress with age but are rarely accompanied by clinical manifestations. Fluid and effusion are usually not visualized in the capsule and pockets of the wrist joint of a healthy hand. However, when using T2-WI, STIR and GRE sequences, a small amount of fluid can be detected. Effusion exceeding 1 - 1.5 mm in thickness is considered pathological. Examination in the coronal plane with a slice thickness of 3 mm makes it possible to evaluate the triangular fibrocartilaginous disc. Its fibers have low signal intensity in the area of the distal articular surface of the ulna.
Sagittal plane. Images obtained in the sagittal plane allow the position of the carpal bones to be assessed in relation to each other, especially the axes of the radius, lunate, capitate and scaphoid bones, which can be measured. The efficiency of these measurements is superior to that of lateral radiographs, since there is no effect of overlapping bones on each other. Palmar and dorsal subluxations can only be accurately visualized in the sagittal plane. The sagittal plane is the primary plane for assessing instability and degenerative changes (Fig. 19.55).
The axial plane allows visualization of the carpal tunnel and its contents. The retinaculum, which is located between the distal surface of the scaphoid, the tubercle of the trapezium and the hamate, is visible as a low-IS structure. The median nerve is located immediately below it and, due to its water and fat content, exhibits a hyperintense signal compared to the flexor tendons in all types of VI. Various locations of the median nerve are clearly visible in the transverse plane and should not be mistaken for pathological changes. The superficial and deep flexor tendons are clearly differentiated, as well as the presence of even small liquid contents of the tendon sheaths, which can be recorded on T2-WI. The palmar and dorsal capsular ligaments are visualized on transverse sections, usually in the presence of pathological changes. Only in this plane can one adequately assess the anatomical and topographic relationships of the radioulnar joint and diagnose minimal palmar and dorsal subluxations (Fig. 19.56).
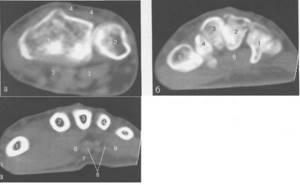
Rice. 19.56. CT scan of the wrist joint.
a — through the plane of the wrist joint: 1 — radius bone; 2 - ulna; 3 - flexor tendons; 4 - extensor tendons.
b - through the plane of the carpal bones: 1 - hamate bone; 2 - capitate bone; 3 - trapezium prominent bone; 4 - trapezium bone; 5 - base of the first metacarpal bone; 6 - tendon of the flexor muscles, c - through the plane of the metacarpal bones: 1 - T metacarpal bone; 2 - II metacarpal bone; 3 - III metacarpal bone; 4 - IV metacarpal bone; 5 - V metacarpal bone; 6 - tendon m. flexor pollicis longus; 7 - palmar aponeurosis; 8 - flexor tendons.
Ultrasound anatomy of the hand and wrist joint
Visualization of the large lateral ligaments of the wrist: the radial, attached to the styloid process of the radius and scaphoid, and the ulnar, starting from the styloid process of the ulna and attached to the triquetrum and partially to the pisiform bone, is also available with ultrasound. The patterns of their echographic picture do not differ from those of other large ligaments. On the dorsal and palmar side, the wrist joint is strengthened by the dorsal palmar and radiocarpal ligaments, which are defined as thin hyperechoic structures. Studies of the tendons of the carpal tunnel and the dorsum of the hand make it possible to well differentiate tendons, especially those located in the synovial sheaths. Scanning of the tendons and median nerve is carried out first in the transverse plane, then the sensor is oriented along the structure that is directly examined. The triangular articular disc in this case has the appearance of a triangular (meniscus-like) structure of moderately increased echogenicity (Fig. 19.57-19.59).
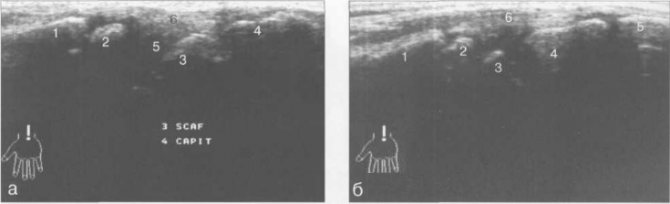
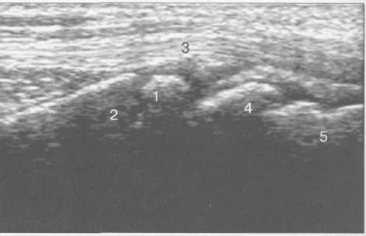
Rice. 19.57. Ultrasound of the wrist joint (6-7 years). Longitudinal scanning.
a - along the palmar surface: 1 - metaphysis of the radius; 2 - epiphysis of the radius; 3 - scaphoid bone; 4 - capitate bone; 5 - wrist joint; 6 - tendon m. flexor.
b — along the dorsal surface: 1 — metaphysis of the radius; 2 - epiphysis of the radius; 3 - scaphoid bone; 4 - capitate bone; 5 - base of the third metacarpal bone; 6 - tendon m. extensor digitorum.
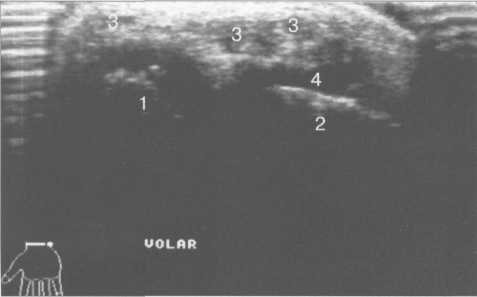
Rice. 19.58. Ultrasound of the wrist joint (6-7 years). Transverse scanning along the palmar surface.
1 - epiphysis of the ulna; 2 - epiphysis of the radius; 3 - tendon of the flexor muscles and their synovial sheaths; 4 - unossified cartilage of the epiphysis.
Rice. 19.59. Ultrasound of the wrist joint (12 years). Longitudinal scanning along the back surface along the axis of the first finger.
1 - metaphysis of the radius; 2 - epiphysis of the radius; 3 - tendon m. extensor carpi radialis; 4 - scaphoid bone; 5 - capitate bone.
Radiation criteria for the normal wrist joint
1. According to radiography:
- - the angle of the “carpal” joint in the palmar projection is 72-95° (it is formed by the intersection of lines running through the styloid processes of the radius and ulna, and the line of the axis of the diaphysis of the radius);
- — the angle of the “carpal” joint in the lateral projection is 79-94°;
- — the width of the joint space of the wrist joint does not exceed 2-2.5 mm;
- — the angle of the wrist joint in the palmar projection is about 30°. This angle is formed by a perpendicular to the axis of the diaphysis of the radial bone and a line running through the edges of the articular surface of the epiphysis of the radial bone;
- — the width of the intercarpal joint is 1.5-2 mm;
- — the width of the carpometacarpal joint is at least 1-2 mm;
- - the total thickness of the cortical layer is about 4-5 mm (measure the proximal phalanx of the index finger);
- — the width of the interphalangeal joints is 1-2 mm;
- - scapholunate angle (between the axes of the bones) no more than 70°;
- - the longitudinal axis passing through the radius, capitate bone and metacarpal bone must coincide.
2. According to MRI data:
- - the wrist angle in the coronal plane is 10-30°, and in the sagittal plane - 10-15°;
- — triangular ulnar disc has an average thickness of 16 mm + 5 mm;
- — the width of the joint in the area of the distal radioulnar space is 3 mm;
- — the width of other joints does not exceed 2 mm.
Indications for diagnostics
It is recommended to conduct research for injuries and inflammatory processes, signs of damage to the joints of the wrist and hand.
The indications are as follows:
- Swelling, deformation and hyperemia in the hand area;
- Pain at rest and movement;
- Hand injuries;
- Rheumatoid arthritis, arthrosis;
- Destructive changes (osteomyelitis);
- Intrauterine developmental anomalies;
- Neoplasms.
The most common referrals for x-rays of the hand are associated with disturbances in the structure of small joints.
An X-ray of the wrist joint diagnoses traumatic injuries based on:
- Contours of hand bones;
- Their integrity;
- Distances between them.
Our clinics in St. Petersburg
Structural subdivision of Polikarpov Alley Polikarpov 6k2 Primorsky district
- Pionerskaya
- Specific
- Commandant's
Structural subdivision of Zhukov Marshal Zhukov Ave. 28k2 Kirovsky district
- Avtovo
- Avenue of Veterans
- Leninsky Prospekt
Structural subdivision Devyatkino Okhtinskaya alley 18 Vsevolozhsk district
- Devyatkino
- Civil Prospect
- Academic
For detailed information and to make an appointment, you can call +7 (812) 640-55-25
Make an appointment
We draw your attention to the schedule of technological breaks in the CT and X-ray rooms.
X-ray, as one of the most informative and visual diagnostic studies, helps to identify various types of damage, developmental pathologies, injuries, inflammatory processes of the wrist joint, the condition of bones, cartilage, soft tissues of the lower part of the forearm, wrist. The most common diseases in this area of the upper limb are arthritis, arthrosis, tendinitis, necrosis, tunnel syndrome, trauma, and osteochondropathy.
X-ray of the wrist and hand
- The method is used in surgery and orthopedics to diagnose traumatic injuries - cracks, dislocations, fractures.
- In rheumatology, the study is important for diagnosing systemic pathologies affecting the joints.
- Endocrinologists use x-rays of the wrist and hand to determine bone age. Such studies are carried out on children whose development and growth differs from the average in one direction or the other.
- The study is prescribed if the patient is diagnosed with a disorder of phosphorus and calcium metabolism, which indicates pathology of the parathyroid glands
The joints of the hands change under the influence of rheumatic diseases. X-rays allow you to assess the extent of damage to bones and soft tissues, showing compactions and thickenings.
Classification of hand bone fractures
Depending on the presence or absence of skin damage over the fracture, the following are distinguished:
- closed fractures - the integrity of the skin is not compromised;
- open fractures - in the area of damage there is a wound in which bone fragments can be identified.
According to the position of bone fragments:
- without displacement - the broken bone maintains its position, the fragments exactly touch along the fracture line;
- with displacement - bone fragments diverge to the sides and, as a result, cannot heal along the fracture line without their comparison - reposition.
According to the involvement of articular structures in the fracture:
- extra-articular fractures - the fracture line passes outside the joint cavity;
- intra-articular fractures - the fracture line is located inside the joint cavity;
- fracture-dislocations - a violation of the integrity of the bone in combination with a dislocation in the adjacent joint.
According to the location of the fracture:
- wrist bone fractures;
- metacarpal bone fractures;
- fractures of the phalanges of the fingers.
You can also classify hand fractures depending on the number of fragments, degree of displacement, and infection. The etiology of the fracture is also important - whether it was traumatic or pathological - arising against the background of bone disease. All these factors influence the choice of treatment tactics for fractures and, ultimately, the possibility of completely restoring the function of the damaged hand.
What will x-rays show?
Diagnostics shows:
- Condition of bone structures;
- Growths of cartilage tissue;
- Lumps around joints;
- Contour of slots;
- Neoplasms on bones and tissues;
- Changes in tissue density, their thinning (signs of arthrosis);
- Intra-articular cysts
- Injuries – cracks, fractures and their exact location.
The radiologist examines the image and writes a conclusion, on the basis of which the orthopedist or trauma surgeon prescribes effective treatment for the patient.
X-ray or MRI of the wrist joint?
Radiography is a fast, affordable and fairly accurate diagnostic method. This method allows you to see the bone structure, analyze its condition, detect pathologies and injuries, displacements and disorders.
But in cases where it is necessary to assess the condition of soft tissues, muscles and ligaments, an MRI may be prescribed. SCT or MRI of the wrist joint is prescribed if certain diseases are suspected, such as carpal tunnel syndrome, cancer, abnormal development of the hand, etc. As a rule, the attending physician independently decides on the need to prescribe one or another method of diagnostic examination of the patient, taking into account the nature of the disease, injury and disorder, the characteristics of the patient’s body, his age, condition and other individual characteristics.










